From Lab to Clinic: The Power of Translational Research for Mental Health
By Craig Fisher, Mi Hillefors, Erin King, Sarah Morris, Jenni Pacheco, Chris Sarampote, and Julia Zehr on behalf of the Division of Translational Research
• 75th Anniversary
For 75 years, NIMH has transformed the understanding and treatment of mental illnesses through basic and clinical research—bringing hope to millions of people. This Director’s Message, guest written by NIMH’s Division of Translational Research, is part of an anniversary series celebrating this momentous milestone.
At the National Institute of Mental Health (NIMH), the Division of Translational Research directs, plans, and supports research and training to build that bridge between basic and clinical research. NIMH’s investments in this research area have led to many scientific advances that have transformed care for the millions of people who live with mental illnesses.
As NIMH celebrates its 75th Anniversary, we are reflecting on some of the transformative milestones of the past, focusing on our present, and envisioning the future. We’ve made some exciting leaps forward that demonstrate why our mission continues to depend so heavily on impactful translational research.
From Neuroscience Tool to Personalized and Targeted Brain Stimulation Therapy
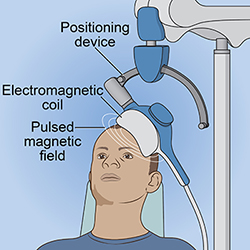
Transcranial magnetic stimulation (TMS) traces its origins to the mid-20th century when researchers began exploring the effects of magnetic fields on the human brain. With TMS treatment, a clinician places an electromagnetic coil over the patient’s head to deliver repeated low-intensity magnetic pulses to specific brain sites.
Some of the first TMS studies in North America were conducted at NIH, within the intramural research programs of NIMH and the National Institute of Neurological Disorders and Stroke. These studies showed that daily, repetitive left prefrontal TMS was safe and well tolerated and might alleviate depression symptoms . NIMH helped researchers take technology that was originally used to study brain function and advance it to a point where it could be tested and used in clinical settings.
NIMH continued to support additional research, including through the Optimize TMS (OPT-TMS) study . This NIMH-funded research, combined with industry-sponsored work, helped provide the pivotal clinical evidence that resulted in the 2008 Food and Drug Administration (FDA) clearance for TMS as a treatment option for depression.
Today, there is substantial evidence that TMS can reduce symptoms of depression and is an effective option when other treatments, such as medication or electroconvulsive therapy, have not been effective or are not well tolerated. It is widely used for research and clinical purposes and is even effective and FDA approved for treating other mental disorders, including severe obsessive-compulsive disorder.
For the transformative care of tomorrow, NIMH is funding more refined and personalized approaches to treat individuals using TMS, including efforts to improve person-specific targeting of brain areas and decrease the amount of time to deliver a full course of treatment . NIMH is also supporting research efforts to combine TMS approaches with psychotherapy to improve treatment outcomes. Additionally, NIMH-supported researchers are now testing the effectiveness of TMS for other mental disorders, such as obsessive-compulsive disorder , anxiety disorders , and post-traumatic stress disorder .
From Understanding Childhood Irritability to Predicting Risk and Treating Mental Illnesses Later in Life
As most parents can tell you, it’s normal for preschool-aged children to throw tantrums and be irritable sometimes. However, some children experience excessive, intense, and frequent explosive tantrums. These extreme tantrums could signal that they’re having difficulties managing their negative emotions and inhibiting their behavior, which are risk factors for developing mental disorders later in life. But how do we know when this behavior isn’t typical?
NIMH is currently supporting research focused on better understanding irritable behavior in children and identifying when we need to intervene. For example, NIMH-supported researchers developed a measure of preschool disruptive behavior, the Multidimensional Assessment of Preschool Disruptive Behavior (MAP-DB) , to help clinicians clarify when tantrums and irritability are age-typical and when they are not. And, research shows that, based on measures of preschool irritability, we can predict children’s risk of developing mental health problems when they reach preadolescence .
Helping children stop extreme tantrums before they happen and better control their irritability may break the link between early irritability and the development of later mental illnesses. Researchers on another NIMH-funded project investigated tantrums and irritability in real time with the goal of developing next-generation technologies to assist in recognizing and preventing clinically meaningful severe irritability. Such efforts could help prevent, diagnose, and treat mental illnesses earlier in the lifespan.
Researchers in the NIMH Intramural Research Program and others supported by NIMH have also begun to develop interventions, such as interpretation bias training and a medication-based intervention , aimed at treating severe irritable behavior in children.
By identifying early signs of mental illness, translational researchers can build a bridge between our understanding of emotional and cognitive processes and our understanding of therapeutic approaches, informing new treatments that can positively impact children’s developmental trajectories.
From Data to Personalized Diagnosis and Treatment
Imagine being able to go to a clinician’s office and get a lab or medical test for depression that helps your doctor know exactly which type of treatment will be most effective for you.
This is a reality in some fields of medicine, like oncology, but we’re still striving for this type of personalized medicine in the mental health field. The current reality is that people who meet the diagnostic criteria for the same mental disorder can often have very different symptom profiles—for example, there are many ways to meet the symptom criteria for a diagnosis of major depressive disorder. This variation across people and the lack of objective markers of mental disorders means that it is often challenging to predict the course a certain disorder might take in any given person or to know when and how to best intervene.
A new NIMH initiative called Individually Measured Phenotypes to Advance Computational Translation in Mental Health (IMPACT-MH) aims to address this problem. IMPACT-MH will support studies that use machine learning and other data-driven approaches to integrate clinical data with data from behavioral assessments. The goal is to identify objective and observable characteristics that can be used to inform and improve clinical decision-making. Consistent with the Research Domain Criteria (RDoC) framework, these objective clinical phenotypes have the potential to enhance diagnosis, predict disorder prognosis, and improve clinical practice by identifying who needs intervention, when they need it, and what type of treatment might work best.
Depression also comes in many forms. Although there are several treatment options, determining the most effective treatment often relies on trial and error, with as many as 40% of people not fully recovered after a year of treatment with one or more available treatment options. Thus, there is an urgent need for tools that can help clinicians predict whether a person with depression will respond to a specific treatment. NIMH is supporting research that aims to take a precision medicine approach to depression treatment. The initial research will test the validity and feasibility of easy-to-use and widely accessible tools for predicting depression treatment response at the individual level.
Building the Bridge to a Brighter Mental Health Future
Although these examples are just a small sampling of past successes, current research, and future potential advances supported by NIMH, they illustrate how critical this area of research is to the mission of transforming research into treatment and solutions for the millions who live with mental illnesses, their loved ones, communities, and society. Translational research is the scientific bridge we need between basic and clinical research—a bridge NIMH will use to transform the future of mental health care.

