Blocking HIV Enzyme Reduces Infectivity and Slows Viral Rebound
• Research Highlight
HIV, or human immunodeficiency virus, is a virus that attacks the body’s immune system. Antiretroviral medications can eliminate the symptoms and prevent the spread of HIV, but there is no cure. People with HIV always carry the virus, and the virus can replicate and infect new cells if people stop taking the medications. A pair of new studies funded by the National Institute of Mental Health (NIMH), National Institute on Aging (NIA), and National Cancer Institute (NCI), all part of the National Institutes of Health, showed that blocking an enzyme involved in forming HIV particles stopped the virus from becoming infectious, suggesting a possible new target for treating HIV infection.
What did researchers look at in these studies?
HIV is an enveloped virus , which means it has an outer layer that surrounds and protects it. This outer layer, known as its viral envelope , is essential for new HIV particles to correctly form and be able to replicate and infect other cells. Norman Haughey, Ph.D. , and Barbara Slusher, Ph.D. , at Johns Hopkins University School of Medicine and Eric Freed, Ph.D. , at the NCI Center for Cancer Research led a multi-center research team in studying the role of a cellular enzyme called neutral sphingomyelinase 2 (nSMase2) in forming the HIV viral envelope.
Haughey, Slusher, Freed, and colleagues looked at the role of nSMase2 in regulating the late stages of HIV assembly via its key role in forming the HIV viral envelope. Their goal was to determine whether blocking nSMase2 could prevent the formation of infectious HIV particles. They also aimed to assess the effects of blocking nSMase2 on viral rebound , which refers to the resurgence of the virus that occurs when people stop taking antiretroviral medications.
What did researchers do in these studies?
To investigate nSMase2’s role in HIV formation, the researchers monitored the effects of blocking nSMase2 in HIV-infected cells using a new compound they developed. The compound can strongly and selectively inhibit the enzyme’s release. Then, they used molecular tools to monitor HIV’s viral spread in both human cell lines and mice with a humanized immune system.
Several types of human cells were infected with HIV. Across all cell lines, blocking nSMase2 in the HIV-infected cells resulted in the production of non-infectious HIV particles and reduced cell survival while having no impact on uninfected cells. Genetically knocking out nSMase2, or preventing its expression, had the same result.
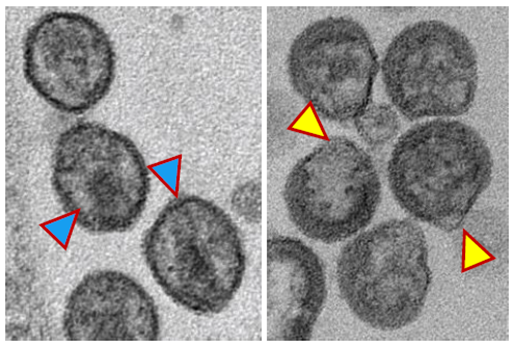
The researchers determined that blocking nSMase2 disrupted the proper formation of the viral envelope and prevented the processing of an HIV protein required for the virus to mature and become infectious. As a result, the HIV particles that developed were misshapen, not fully mature, and not infectious. The authors concluded that nSMase2 is critical for creating the HIV envelope and plays some (yet to be determined) role in the maturation of HIV particles.
Next, the researchers treated HIV-infected mice with either standard antiretroviral medications or the compound they developed to block the release of nSMase2. After several weeks, they stopped treatment in both groups and tracked plasma viral loads , reflecting the amount of actively replicating virus in the body.
Both treatments effectively decreased HIV levels, pushing viral loads to undetectable levels after a few weeks. However, in mice treated with the typical combination of antiretrovirals, their HIV levels quickly rebounded after stopping the medications. In contrast, mice treated with the nSMase2 blocker did not show viral rebound—if they reached undetectable levels of HIV, the virus was not detected for up to 4 weeks after treatment was stopped.
This lack of viral rebound in mice treated with the nSMase2 blocker occurred alongside the death of specific cells known to replicate HIV. The latter finding suggests that blocking nSMase2 may have worked by selectively destroying HIV-infected cells in the body.
What have we learned from these studies?
Collectively, the findings indicate that nSMase2 plays a crucial role in the final stages of HIV assembly, replication, and infectivity. Blocking nSMase2 greatly diminished the ability of HIV particles to reproduce and infect new cells. Notably, the benefits of blocking nSMase2 were maintained a month later in 80% of infected animals even after removing the treatment.
These studies have the potential to lead to better methods for effectively treating HIV long-term or potentially curing HIV infection. By demonstrating for the first time the use of an nSMase2 blocker to stop actively replicating HIV in living cells, the researchers identified an important new therapeutic target and introduced the possibility of developing medications that can kill HIV-infected cells—something that no HIV drugs currently on the market can do. Although these pre-clinical studies are only a first step, the researchers are optimistic about the potential to advance future HIV treatments.
References
Waheed, A. A., Zhu, Y., Agostino, E., Lar Naing, L., Hikichi, Y., Soheilian, F., Yoo, S.-W., Song, Y., Zhang, P., Slusher, B. S., Haughey, N. J., & Freed, E. O. (2023). Neutral sphingomyelinase 2 is required for HIV-1 maturation. Proceedings of the National Academy of Sciences, 120(28), Article e2219475120. https://doi.org/10.1073/pnas.2219475120
Yoo, S.-W., Waheed, A. A., Deme, P., Tohumeken, S., Rais, R., Smith, M. D., DeMarino, C., Calabresei, P. A., Kashanchi, F., Freed, E. O., Slusher, B. S., & Haughey, N. J. (2023). Inhibition of neutral sphingomyelinase 2 impairs HIV-1 envelope formation and substantially delays or eliminates viral rebound. Proceedings of the National Academy of Sciences, 120(28), Article e2219543120. https://doi.org/10.1073/pnas.2219543120
