Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Bipolar Youths’ Misreading of Faces May be Risk Marker for Illness
Linked to Genetics, Altered Brain Circuitry
• Science Update
Youngsters with pediatric bipolar disorder and healthy peers who have first-degree relatives with bipolar disorder share the same difficulty labeling facial emotions, NIMH researchers have discovered. Reporting in the February 2008 online edition of the American Journal of Psychiatry, the scientists suggest that the facial emotion recognition impairment might be part of an inherited predisposition to the illness.
Two related imaging studies traced face emotion labeling deficits in youngsters with pediatric bipolar disorder to weak connections and differences in activity of a brain circuit responsible for interpreting the meaning of social and emotional stimuli. Evidence suggested that the differences were stable traits, unrelated to effects of medications or mood states.
“Since we know more about the circuitry of basic processes like facial emotion processing than we do about the circuitry of complex psychiatric symptoms like mania and depression, it serves as a kind of Rosetta Stone for unearthing new clues,” explained Ellen Leibenluft, M.D., chief of the intramural NIMH Section on Bipolar Spectrum Disorders, Mood and Anxiety Disorders Program, which is conducting the studies.
Understanding such specific vulnerabilities in emotional processing may someday lead to improved treatment, diagnosis, and ultimately prevention of bipolar disorder in children, say the researchers.
Disorder-Linked Trait Runs in Families
Having a sibling or parent with bipolar disorder greatly increases the risk of a child having bipolar disorder, indicating that the illness has a substantial genetic component. Difficulty identifying facial emotions might be a marker of that risk.
To examine this, Melissa Brotman, Ph.D., Leibenluft and colleagues tested 52 youths with bipolar disorder, 24 healthy youths who have first degree relatives with bipolar disorder, and 78 controls, ages 4-18, all unrelated, on a facial emotion recognition task (below). Participants indicated if faces that appeared for two seconds presented happiness, sadness, anger or fear. Both bipolar and at-risk groups were equally prone to mis-identifying face emotions on the task when compared to controls. The researchers later confirmed these results in expanded samples that included some patients from the same families.
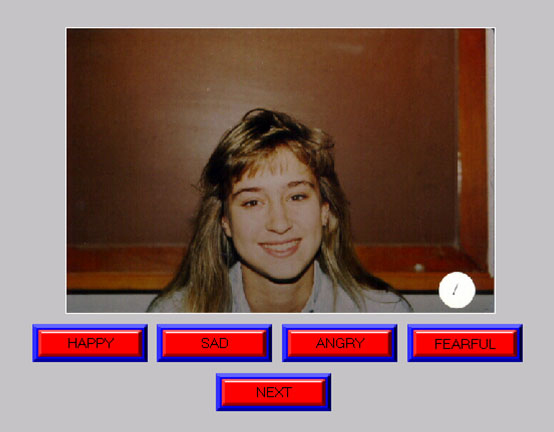
Healthy youths with family histories of bipolar disorder, like youths with the disorder, made more errors on this task (see above), which required them to identify various facial emotions as the faces flashed on a screen.
Reproduced with permission from Stephen Nowicki, Ph.D., Emory University
Weakened Brain Circuit May Skew Perception
The NIMH researchers reported in an earlier imaging study that the amygdala, a brain area associated with processing fear-producing stimuli, is over-activated when youngsters with bipolar disorder misread neutral facial expressions as threatening.
In a follow-up study published in the January 2008 issue of the Journal of Child Psychology and Psychiatry, Brendan Rich, Ph.D., Leibenluft and colleagues found that youngsters with bipolar disorder have weakened connections between the amygdala and three other brain areas critical for processing faces and emotional stimuli.
Using functional magnetic resonance imaging (fMRI), the researchers scanned 33 patients with bipolar disorder and 24 healthy youngsters while they rated faces expressing different emotions on measures such as hostility and fear. The analysis measured the extent to which the amygdala communicated with other brain areas during the task – circuit connectivity.
Since one of the amygdala’s jobs is to assign emotional significance to faces, diminished input from the three key brain areas involved in face emotion processing could cause the amygdala to “aberrantly perceive neutral faces as threatening,” as the earlier imaging study found. Poor connections could also lead to the misinterpretations of social signals and impaired emotional learning and memory that is characteristic of the disorder, the researchers said.
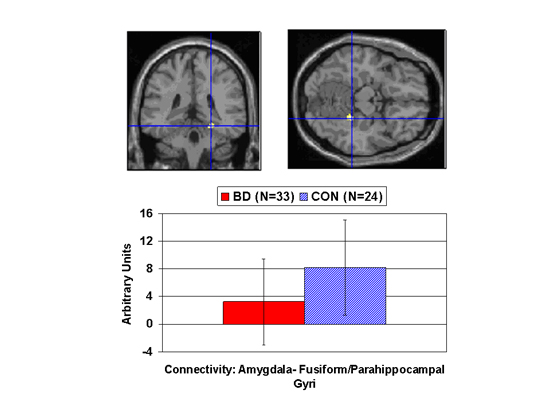
Compared with controls (blue), youngsters with bipolar disorder (red) had lower connectivity between the amygdala, a fear hub, and other parts of a circuit that processes facial emotion, including the fusiform gyrus, the white area where lines intersect in the scan images. This area is important for imparting social meaning to information. Arbitrary Units indicates the strength of the correlation in activity between the amygdala and the other circuit areas. The researchers suggest impairments in this circuit could lead to misperceptions of emotional expressions.
Fearful Faces Forgotten, Yet Happy and Angry Faces Provoked Stronger Reactions
Since pediatric bipolar disorder is characterized by extremes of both positive and negative emotion, the NIMH researchers suspect that patients’ brain activity might differ from that of controls while processing both kinds of facial emotion.
Indeed, Daniel Dickstein, M.D., Leibenluft, and colleagues found in an fMRI study that youngsters with bipolar disorder had reduced overall memory for emotional faces – especially for fearful faces. However, when they did successfully remember happy or angry faces, their brains showed greater activity than control subjects. The researchers report their findings in the November, 2007 issue of the journal Bipolar Disorders.
The researchers scanned 23 patients and 22 control subjects while they viewed and rated emotional faces. A half hour after the scan, subjects were given a surprise memory test in which some of the same test faces appeared – but this time showing neutral expressions. Thus, the researchers had data on subjects’ recollection of faces, as well as their initial face emotion ratings and brain activity while making these ratings.
The striatum and anterior cingulate are key hubs in the brain’s reward system. The researchers found that happy faces triggered over-activation in these regions in youth with bipolar disorder compared to healthy youth. This is consistent with other evidence that youngsters with bipolar disorder are impaired on behavioral tasks involving reward-processing.
Angry faces triggered increased activation in patients, compared to controls, in the orbitofrontal cortex. This region is a seat of irritability and aggression in response to frustration or perceived threats – behaviors characteristic of bipolar disorder. Thus, in youths with bipolar disorder, positive and negative face stimuli elicited over-activation in brain regions involved in regulating emotions and behavior.
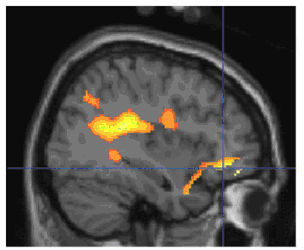
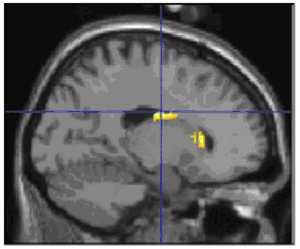
When successfully encoding angry faces, youngsters with bipolar disorder showed increased activity in the right orbitofrontal cortex, the yellow area where lines intersect in the image to the left, compared with healthy youth. Those with bipolar also showed increased activity in the striatal region, the yellow area where lines intersect in the image to the right, when successfully encoding happy faces. These areas are parts of a circuit that processes facial emotion and regulates emotions and behavior. Yellow indicates differences in activity between youth with bipolar disorder and controls during the experimental task. Functional MRI data superimposed on structural MRI scans.
Brotman MA, Guyer AE, Lawson ES, Horsey SE, Rich BA, Dickstein DP, Pine DS, Leibenluft E. Facial Emotion Labeling Deficits in Children and Adolescents at Risk for Bipolar Disorder.Am J Psychiatry. 2008 Feb 1; [Epub ahead of print] PMID: 18245180
Rich BA, Fromm SJ, Berghorst LH, Dickstein DP, Brotman MA, Pine DS, Leibenluft E. Neural connectivity in children with bipolar disorder: impairment in the face emotion processing circuit. J Child Psychol Psychiatry. 2008 Jan;49(1):88-96. PMID: 18181882
Dickstein DP, Rich BA, Roberson-Nay R, Berghorst L, Vinton D, Pine DS, Leibenluft E. Neural activation during encoding of emotional faces in pediatric bipolar disorder. Bipolar Disord. 2007 Nov;9(7):679-92. PMID: 17988357
