Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Thinning Tissue in Right Half of Brain Signals Increased Risk of Inherited Depression
• Science Update
In cases of familial depression, changes in tissue thickness in key brain structures in the right half of the brain may increase a person's risk for developing depression, according to NIMH-funded researchers. Similar changes in the left half of the brain were linked to the severity of a person's existing depression or anxiety symptoms. Based on their findings, the researchers proposed a possible mechanism for how these brain changes affect depression risk in the April 14, 2009, issue of the Proceedings of the National Academy of Sciences.
Background
Some types of depression run in families, and certain changes in brain structure and function have been observed in people with the disorder. However, until recently, scientists have been unclear on the exact relationship between these brain changes and depression.
Building on previous research with a three-generation study population, Myrna Weissman, Ph.D., and Bradley Peterson, M.D., both of Columbia University College of Physicians & Surgeons and New York State Psychiatric Institute, and colleagues used magnetic resonance imaging (MRI) to assess brain changes in 131 people, ages 6-54. Roughly half of these participants were considered at high risk for major depressive disorder (MDD), due to having at least one parent or grandparent in the study diagnosed with the illness. The other half, considered at low risk, had no family history of the illness.
Results of the Study
From pre-scanning interviews, the researchers found that people in the high-risk group were more likely than those in the low-risk group to report having MDD or an anxiety disorder at some point in their lives. MRI scans showed that, on average, those in the high-risk group had 28 percent thinner brain tissue across a broad range of brain structures in the right half of the brain. These changes were observed in young children in the high-risk group and in older high-risk individuals who had never suffered from MDD or an anxiety disorder themselves.
The brain areas most affected by this thinning govern attention and the ability to process emotional or social cues (such as faces or family pictures). In tests involving these right-brain tasks, the researchers found that thinner tissue in these areas was linked to greater inattention and poorer performance in immediate and delayed visual memory.
Similar patterns of tissue thinning in the left half of the brain appeared to be related to the severity of a person's existing MDD or anxiety disorder symptoms in both the high- and low-risk groups. This thinning was not as pronounced as the thinning in the right half of the brain, and the difference in tissue thickness between the high- and low-risk groups was not statistically significant.
Significance
The findings strongly suggest that changes in tissue thickness in the right half of the brain directly affect a person's inherited risk for developing MDD. The pattern of tissue thinning appears to be related to problems with attention and processing of emotional or social signals. Such problems may increase a person's vulnerability to developing mood or anxiety disorders, according to the researchers.
That the thinning was present in people at high risk, but who had never had MDD or an anxiety disorder, as well as in high-risk children who had not been diagnosed with depression, shows that these brain changes likely come before illness onset and that they occur very early in life, possibly before birth, say the researchers. Furthermore, while thinning in the right half of the brain contributes to risk, thinning in the left half of the brain appears to be required in order for a person to show symptoms of these illnesses.
What's Next
More research is needed to determine if the inherited risk for MDD is purely genetic, if there are specific environmental factors necessary for triggering genetic risk, or whether there is a combination of factors involved. Increased understanding of how risk translates into developing MDD or other mental disorders may lead to new methods of diagnosing, treating, or preventing these illnesses.
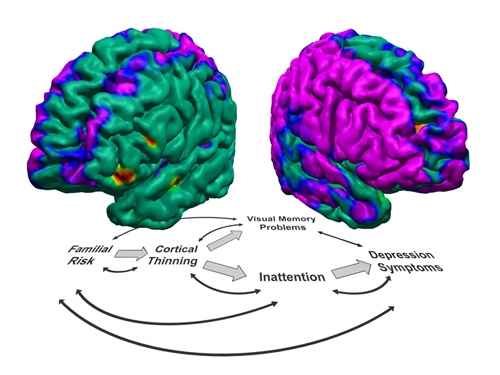
Top: Color coded MRI brain maps of differences in tissue thickness between study participants at high- vs. low-risk for familial depression. Left half of brain is shown on the left and right half on the right. Cool colors (blue and purple) denote thinner areas in the high-risk group; warm colors (yellow, orange, and red) are significantly thicker areas; green areas show little to no difference in tissue thickness.
Bottom: Flowchart represents a proposed model for how some MDD or anxiety disorders develop. Double-headed arrows indicate factors that may influence each other and jointly contribute to disease risk. Block arrows show the hypothetical progression from inherited risk to development of symptoms.
Reference
Peterson BS, Warner V, Bansal R, Zhu H, Hao X, Liu J, Durkin K, Adams PB, Wickramaratne P, Weissman MM. Cortical thinning in persons at increased familial risk for major depression . Proc Natl Acad Sci U S A. 2009 Apr 14;106(15):6273-8. PMID: 19329490
