Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Imaging Studies Help Pinpoint Child Bipolar Circuitry
In-Scanner Tasks Reveal Divergences with Overlapping Disorders
• Science Update
A series of imaging studies are revealing that the brain works differently in youth with bipolar disorder (BD) than in chronically irritable children who are often diagnosed with pediatric BD.
"This suggests that chronically irritable children may suffer from a syndrome distinct from BD and may require different treatments," said Ellen Leibenluft, M.D., chief of NIMH's Section on Bipolar Spectrum Disorders, which is conducting the studies.
Episodic vs. Chronic Irritability
Like BD in adults, some children have classic episodes of mania, with a distinct change in mood becoming more irritable or euphoric than usual – along with a simultaneous change in sleep, activity, and thought patterns. Instead of such clear-cut episodes interspersed with periods of normal mood or depression, many more children present with chronic, severe irritability. Whether these children also have pediatric BD has been at issue.
To capture these severely irritable children without clear episodes, Leibenluft and her colleagues have defined a syndrome they call severe mood dysregulation (SMD). Youth with SMD share certain overlapping features with their bipolar peers, such as poor frustration tolerance and impaired ability to recognize emotional facial expressions, but differ in symptoms, course, and pedigree.
Leibenluft's team showed in earlier studies that children with BD tend to come from families with histories of the disorder and tend to carry the disorder into adulthood, while children with SMD don't. Children with SMD are more prone to developing depression or anxiety disorders rather than BD as adults.
SMD is now embodied in the similar Temper Dysregulation Disorder with Dysphoria (TDD) category of the recently proposed psychiatric diagnostic manual revision (DSM-V), which cites the NIMH team's studies in defining TDD. SMD/TDD is much more common than pediatric BD, affecting about 3.2 percent of children, but no less disabling.
Children with BD or SMD both tend to have attention deficit hyperactivity disorder (ADHD) symptoms, but children with just ADHD differ from those with SMD in not experiencing marked irritability, and from those with BD in not having episodes of mania or depression. To further clarify distinctions among these diagnoses, the NIMH researchers are using brain imaging to compare the workings of neural circuits in pediatric BD and these seemingly related disorders.
"We're finding that the same clinical symptom, or behavioral deficit, may be mediated by more than one brain mechanism," explained Leibenluft.
Reading Fear into Neutral Faces
Previous studies also suggested that children with BD have weakened connections between the amygdala, the brain's fear hub, and other brain structures involved in processing facial emotion. These weakened connections may contribute to the children's impaired ability to recognize emotional expressions.
In a follow-up study, reported in the January 2010 issue of the American Journal of Psychiatry, Melissa Brotman, Ph.D., Leibenluft and colleagues compared amygdala activity in children with ADHD, BD, SMD, and healthy controls while they rated emotion in neutral faces. Functional magnetic resonance imaging (fMRI) revealed that this task seemed to engage unique neural mechanisms in each syndrome.
For example, when rating how fearful the neutral faces appeared, the amygdala over-activated in ADHD, under-activated in SMD, and unexpectedly – activated normally in bipolar disorder relative to controls.
In previous such studies, children with bipolar disorder showed increased amygdala activity - and even in this study, they subjectively rated the neutral faces as more fearful than did controls. So the latter outcome may be a fluke. Still, the findings add to evidence of divergence between bipolar and SMD in the way the brain processes facial emotion.
Since studies have shown that depressed children have reduced amygdala activity, and SMD is a risk factor for adult depression, the researchers suggest that amygdala dysfunction in SMD might be a predictor of later depression.
This first fMRI study to include children with SMD and the first to compare amygdala activation across these groups suggests that, despite some overlapping symptoms, the brain may be working differently in each disorder.
Amygdala (yellow area where lines intersect) over-activated in subjects with ADHD and under-activated in those with SMD while they rated the fearfulness of neutral faces.
Slow to Recognize Emotion
In an earlier study, children with BD, SMD and controls were asked to label the emotion emerging as faces morphed from a neutral to full expression. Children with either BD or SMD took significantly longer than controls before recognizing fear, surprise, disgust and happy expressions, report Brendan Rich, Ph.D., Leibenluft and colleagues in the Spring, 2008 issue of Development and Psychopathology.
Since another NIMH study had found that this impairment is not shared by children with ADHD or other childhood disorders, the results suggest that the two disorders may be on a continuum in terms of their underlying biological and psychological causes. Yet, the impaired face labelling was linked to different psychosocial impairments in the two groups – perhaps also hinting at some differences in underlying brain mechanisms, suggest the researchers. It was associated with dysfunctional family relationships among children with SMD, in contrast to deficient social reciprocity skills among youth with BD.
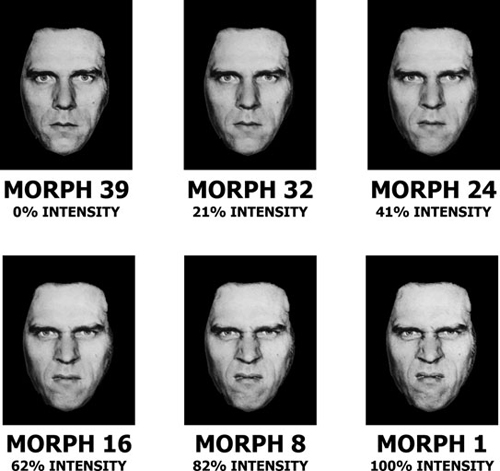
Children with both bipolar disorder and SMD were slow to identify emotional facial expressions, such as disgust (above) as they morphed from neutral to full intensity.
Accentuating the Negative
Although chronic severe irritability is the hallmark symptom of SMD, irritability is also common in youth with BD, both within and between manic and depressive episodes. Children with irritability tend to have difficulty coping with frustration. The NIMH researchers had shown earlier that when frustrated by negative feedback, youth with BD emit brain wave patterns signaling impaired attention.
To pinpoint the underlying neural circuitry, the researchers turned to an imaging technique called magnetoencephalography (MEG), which can detect even fleeting, millisecond events deep in the brain. Rich, Leibenluft and colleagues reported on the first MEG study of childhood BD online December 27, 2009 in the journal Depression and Anxiety. They scanned youth with the disorder and controls while they performed an attention task rigged to frustrate them by leading them to believe – for a time – that they were losing money won earlier (Ultimately, their winnings were restored).
As expected, youth with BD reported being more upset by the frustration-inducing negative feedback than did the controls. This irritability was associated with over-activation of an emotion-processing circuit centered on a brain area earlier implicated in BD called the anterior cingulate cortex (ACC).
Youth with BD showed greater activation than controls after negative feedback (losing money) in an area of the left ACC. By contrast, controls showed greater activation than bipolar youth after positive feedback (winning money) in an area of the right ACC.
Such over-activation in the left ACC likely reflects exaggerated attention and disproportionate thinking about their performance in response to negative feedback among bipolar youth, suggest the researchers. This would exacerbate irritability and frustration, perhaps distracting them from positive information.
Related studies show that children with either SMD or BD experience increased frustration in such attention tasks relative to controls, but the SMD and BD children differ in the way their brains process the tasks. The SMD children's brains respond more like those of children with ADHD.
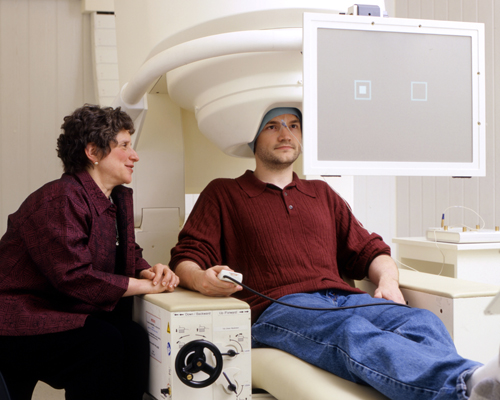
Leibenluft looks on as research fellow Tyler Ard demonstrates the attention task in MEG scanner.
| Left Anterior Cingulate Cortex | Right Anterior Cingulate Cortex |
|---|---|
|
|
Left: Left anterior cingulate cortex (where lines intersect) over-activated in pediatric BD in response to negative feedback. Right: Right anterior cingulate cortex (where lines intersect) under-activated in pediatric BD in response to positive feedback. MEG data superimposed on MRI data.
Different Circuitry May Call for Different Treatments
On the mistaken assumption that they have BD, many children with SMD have been prescribed anticonvulsant and antipsychotic medications. Such misdiagnosis can expose children unnecessarily to risks of serious long-term side effects with these agents, including weight gain, diabetes and heart disease.
Leibenluft's team is conducting a clinical trial to test whether children with SMD might be better helped instead with treatments more appropriate for depression and anxiety – disorders more related to their illness – and their ADHD symptoms. After discontinuing their other medications, children in the study are first given a stimulant medication, followed by a randomized course of treatment with either an antidepressant or placebo.
"In many ways, this is the single most important study we're doing, in terms of public health impact," noted Leibenluft.
References
Amygdala activation during emotion processing of neutral faces in children with severe mood dysregulation versus ADHD or bipolar disorder . Brotman MA, Rich BA, Guyer AE, Lunsford JR, Horsey SE, Reising MM, Thomas LA, Fromm SJ, Towbin K, Pine DS, Leibenluft E. Am J Psychiatry. 2010 Jan;167(1):61-9. Epub 2009 Nov 16.PMID: 19917597
Face emotion labeling deficits in children with bipolar disorder and severe mood dysregulation. Rich BA, Grimley ME, Schmajuk M, Blair KS, Blair RJ, Leibenluft E. Dev Psychopathol. 2008 Spring;20(2):529-46.PMID: 18423093
A preliminary study of the neural mechanisms of frustration in pediatric bipolar disorder using magnetoencephalography. Rich BA, Holroyd T, Carver FW, Onelio LM, Mendoza JK, Cornwell BR, Fox NA, Pine DS, Coppola R, Leibenluft E. Depress Anxiety. 2009 Dec 27. [Epub ahead of print] PMID: 20037920
Temper Dysregulation Disorder with Dysphoria (TDD)http://www.dsm5.org/Proposed%20Revision%20Attachments/Justification%20for%20Temper%20Dysregulation%20Disorder%20with%20Dysphoria.pdf
