Archived Content
The National Institute of Mental Health archives materials that are over 4 years old and no longer being updated. The content on this page is provided for historical reference purposes only and may not reflect current knowledge or information.
Study Shows Possibilities for Predicting How Patients Will Respond to Antidepressants
• Science Update
In a study of an experimental treatment for major depression, pretreatment testing to probe the function of a specific brain center predicted how patients would respond to ketamine, a medication that can lift depression rapidly in some people. The work suggests it may be possible to develop ways to use such assessments in the future, not only to better understand depression, but to guide treatment choices for individuals.
Background
There remains an urgent need for new antidepressant medications that work by alternative mechanisms than those of existing treatments. There is a particular need for medications that can act more rapidly than those currently available, which can take weeks; and for ways to predict which patients are likely to be helped by specific medications. Ketamine, the drug used in this study, can relieve symptoms of depression within hours. While ketamine has side-effects that rule it out as a depression treatment, continuing research on ketamine can help provide the basis for developing other medications with a similar and rapid mechanism of action.
One avenue towards developing new medications is to map the brain circuits that are not functioning normally in depression. Scientists can monitor the level of function of specific brain areas while a subject is carrying out a mental task. The same type of monitoring might also be used before starting an antidepressant treatment to determine how baseline activity in the brain in patients with depression might correlate with subsequent clinical improvement.
This Study
Fifteen patients with major depression took part in this study. Before receiving ketamine, patients carried out a test that involves working memory, the kind of short-term memory called upon, for example, when briefly holding in mind a telephone number when dialing it right after reading it.
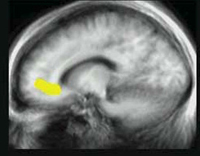
While patients carried out the task, investigators monitored activity in an area of the brain that has connections to both emotional and cognitive brain centers, the pregenual anterior cingulate cortex (pgACC). The monitoring technology used is called magnetoencephalography (MEG) which tracks the magnetic fields created by electrical activity of neurons in the brain.
In depressed patients doing the working memory test (which involves no emotional content) those in whom the pgACC was least active had the most improvement in symptoms in response to ketamine. By contrast, in previous research, when depressed patients viewed images with emotional content (fearful faces), those in whom the pgACC was most active had the most improvement in symptoms in response to ketamine. Together, the results suggest that low activity of this part of the brain in response to non-emotional tasks, and high activity in response to emotional content, predicted that a person with depression would respond to ketamine.
This study also looked at whether the activity of the pgACC seemed to be reflected in simultaneous activity of the amygdala—a part of the brain that plays a role in emotional processing. Patients in whom there was a tight synchrony between both brain centers during the working memory task were less responsive to ketamine.
Significance
In this study, carried out by scientists Giacomo Salvadore, Carlos Zarate, and colleagues in NIMH's intramural research program, activity in the pgACC, and the degree to which it was functionally linked to the amygdala, provided indicators, or biomarkers, of the extent to which patients would respond to treatment with ketamine. Giving individuals a task that engages the brain in specific ways helps scientists measure the efficiency with which a given brain circuit is functioning. The authors explain that in studies of healthy subjects, activity of the pgACC is increased when a person is processing information with emotional content but not when a person is focusing on more emotionally neutral information processing. Depressed persons in whom the pattern of pgACC activation was closer to that seen in nondepressed persons had better responses to treatment. The authors also observe that the mood-regulating circuitry studied in this work seems to be active in depressed patients, even when they are given a task without emotional content.
In addition to developing medications with new mechanisms of action, it will be important to develop ways to predict who will respond. This study provides clues to the circuitry underlying major depression and for possible future approaches to matching treatment to patient.
Reference
Salvadore, G., Cornwell, B.R., Sambataro, F., Latov, D., Colon-Rosario, V., Carver, F., Holroyd, T., Diaz-Granados, N., Machado-Vieira, R., Grillon, C., Drevets, W.C. and Zarate, C. A. Anterior cingulated desynchronization and functional connectivity with the amygdala during a working memory task predict rapid antidepressant response to ketamine. Neuropsychopharmacology. 2010 Jun;35(7):1413-4.
