Section on Development and Affective Neuroscience (SDAN)
Anxiety and depression in children are serious conditions that carry an increased risk for anxiety or depression in adulthood. The Section on Development and Affective Neuroscience (SDAN) seeks to understand how information processing in the brain differs among children, adolescents, and adults with anxiety and depression across the lifespan, in comparison to healthy volunteers. We aim to use this information to develop better treatments for these conditions. SDAN is led by Dr. Daniel Pine and is housed in the Emotional and Development Branch of the National Institute of Mental Health (NIMH)’s Division of Intramural Research Programs.
Understanding Brain Circuitry
Over the last decade, brain circuitry that plays a major role in fear and reward emotions has been linked to several different brain structures and regions. Researchers in SDAN study how this circuitry relates to impairment and recovery from anxiety and depression.
Some children and adolescents with anxiety disorders may continue to have those disorders as adults, may develop mood disorders, or may have no psychopathology as adults. It is important to understand how brain circuitry plays a role in these outcomes. For this reason, we also investigate how this circuitry changes and functions over time in those at risk for development of these conditions.
Research Goals
In SDAN, we apply insights from neuroscience to inform understandings of risk, diagnosis, and treatment of pediatric mental disorders. This approach is translational in its attempts to answer questions that are essentially clinical through applications of basic science. We conduct this work by applying brain-oriented tools through three sets of studies, each focused on anxiety disorders.
These sets comprise studies on:
1) Heterogeneity in clinical aspects of anxiety disorders, including both comorbidity and outcomes,
2) Brain-based predictors of response to treatment, and
3) Implementation of randomized controlled trials that use novel therapies discovered through basic research.
Finally, a key focus of SDAN research is the development and distribution of state-of-the-art approaches to the analysis of neuroimaging data, including sophisticated methods for examining connectivity and inter-regional relationships in the brain. We strive to make these tools publicly available to scientists around the world.
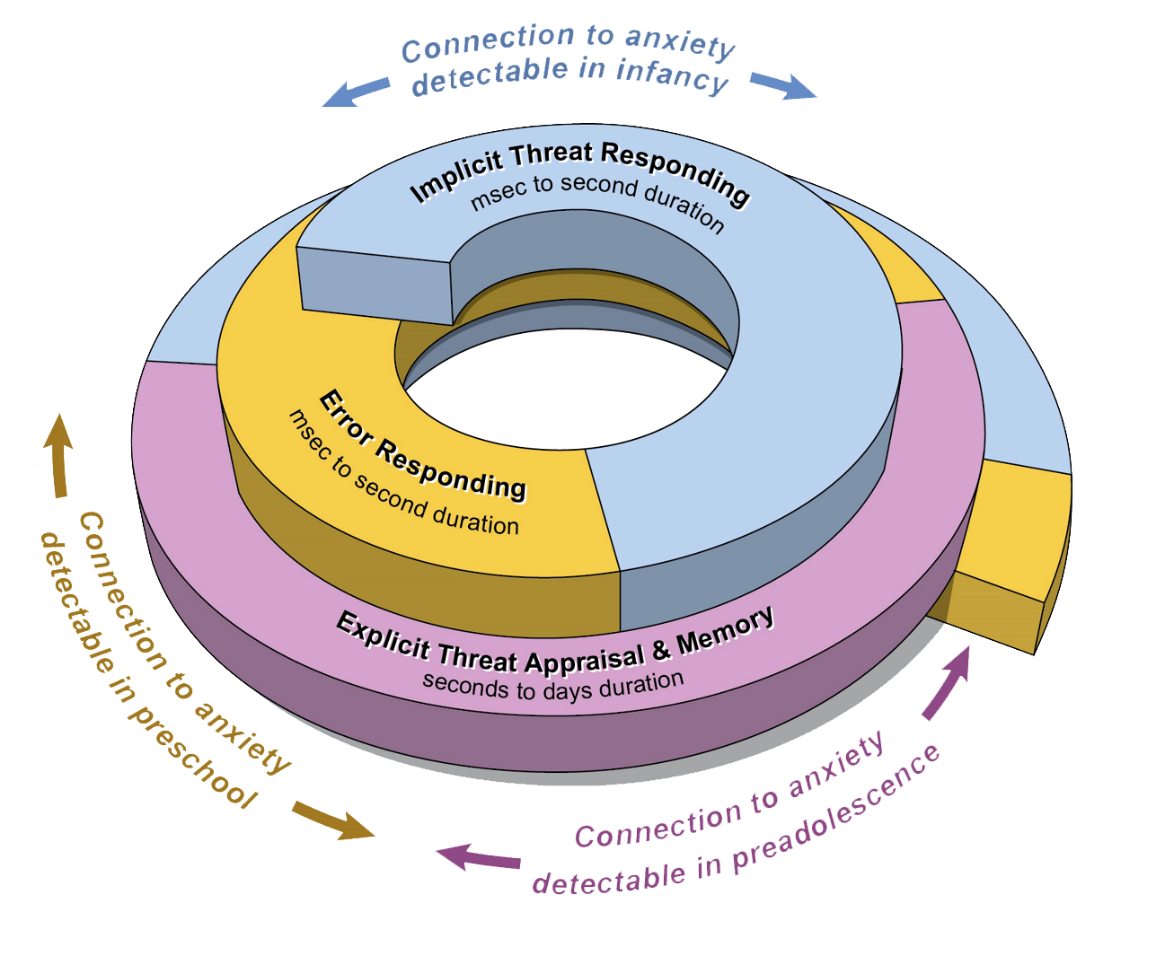
Researchers in SDAN study three sets of core psychological processes through laboratory-based tasks. These processes are functions performed by the brain. They show relations to anxiety that first arise in different stages of life.
- The first process is implicit responding to threats, meaning the body’s involuntary response to things that could cause harm. This process begins in infancy and continues throughout life.
- The second process is the brain’s response to errors. This process begins in preschool and continues throughout life.
- The third process involves threat appraisal (how the brain assesses the level of a threat) and episodic memory (the ability to recall and re-experience specific memories). This process begins in preadolescence and continues throughout life.
SDAN research examines interactions among these three processes as they occur through adolescence.
Select Publications
- Shared and Anxiety-Specific Pediatric Psychopathology Dimensions Manifest Distributed Neural Correlates
- Childhood Antecedents and Risk for Adult Mental Disorders
- The Risk for Early-Adulthood Anxiety and Depressive Disorders in Adolescents With Anxiety and Depressive Disorders
- Fluvoxamine for the treatment of anxiety disorders in children and adolescents
- Infant behavioral inhibition predicts personality and social outcomes three decades later
Contact Information
Section on Development and Affective
Neuroscience NIMH
15K North Drive, MSC-2670
Bethesda, MD 20892-2670
Phone: 301-594-1318
Email: Dr. Pine (pined@mail.nih.gov)
Banner artwork by Sonia Ruiz

