FY 2020 Budget - Congressional Justification
- Organization Chart
- Appropriation Language
- Amounts Available for Obligation
- Budget Mechanism Table
- Major Changes in Budget Request
- Summary of Changes
- Budget Graphs
- Budget Authority by Activity
- Authorizing Legislation
- Appropriations History
- Justification of Budget Request
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
Department of Health and Human Services
National Institutes of Health
National Institute of Mental Health
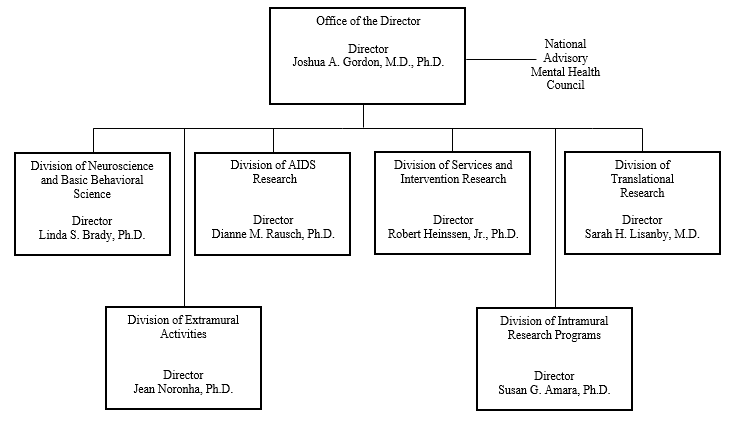
Organization Chart
[Top]
Appropriation Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, [$1,812,796,000]$1,560,422,000.
[Top]
NIH INNOVATION ACCOUNT, CURES ACT
(INCLUDING TRANSFER OF FUNDS)
For necessary expenses to carry out the purposes described in section 1001(b)(4) of the 21st Century Cures Act, in addition to amounts available for such purposes in the appropriations provided to the NIH in this Act, [$711,000,000]$492,000,000, to remain available until expended: Provided, That such amounts are appropriated pursuant to section 1001(b)(3) of such Act, are to be derived from amounts transferred under section 1001(b)(2)(A) of such Act, and may be transferred by the Director of the National Institutes of Health to other accounts of the National Institutes of Health solely for the purposes provided in such Act: Provided further, That upon a determination by the Director that funds transferred pursuant to the previous proviso are not necessary for the purposes provided, such amounts may be transferred back to the Account: Provided further, That the transfer authority provided under this heading is in addition to any other transfer authority provided by law.
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2018 Final |
FY 2019 Enacted |
FY 2020 President's Budget* |
| Appropriation2 | $1,754,775 | $1,870,296 | $1,630,422 |
| Mandatory Appropriation (non-add) | |||
| Type 1 Diabetes | (0) | (0) | (0) |
| Other Mandatory financing | (0) | (0) | (0) |
| Rescission | 0 | 0 | 0 |
| Sequestration | 0 | 0 | 0 |
| Secretary's Transfer | -3,223 | 0 | 0 |
| Subtotal, adjusted appropriation | $1,751,552 | $1,870,296 | $1,630,422 |
| OAR HIV/AIDS Transfers | 2,882 | 0 | 0 |
| HEAL Initiative Transfer | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,754,434 | $1,870,296 | $1,630,422 |
| Unobligated balance, start of year | 0 | 0 | 0 |
| Unobligated balance, end of year | 0 | 0 | 0 |
| Subtotal, adjusted budget authority | $1,754,434 | $1,870,296 | $1,630,422 |
| Unobligated balance lapsing | -11 | 0 | 0 |
| Total obligations | $1,754,423 | $1,870,296 | $1,630,422 |
1 Excludes the following amounts for reimbursable activities carried out by this account: FY 2018 - $8,531 FY 2019 - $10,050 FY 2020 - $10,050
2 Of which $43.0 million in FY 2018, $57.5 million in FY 2019, and $70 million in FY 2020 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
[Top]
Budget Mechanism - Total
| Mechanism | FY 2018 Final | FY 2019 Enacted | FY 2020 Presidents Budget | FY 2020 +/- FY 2019 Enacted | ||||
| No. | Amount | No | Amount | No. | Amount | No | Amount | |
| Research Projects | ||||||||
| Noncompeting | 1,484 | $791,480 | 1,518 | $814,336 | 1,560 | $871,375 | 42 | $57,039 |
| Administrative Supplements | (138) | 19,887 | (124) | 16,604 | (75) | 10,000 | (-49) | -6,604 |
| Competing | ||||||||
| Renewal | 59 | 37,621 | 91 | 84,042 | 27 | 17,493 | -64 | -66,549 |
| New | 542 | 306,114 | 611 | 315,411 | 274 | 176,051 | -337 | -139,360 |
| Supplements | 1 | 120 | 1 | 138 | 1 | 56 | 0 | -82 |
| Subtotal Competing | 602 | $343,855 | 703 | $399,591 | 302 | $193,600 | -401 | -$205,990 |
| Subtotal RPGs | 2,086 | $1,155,222 | 2,221 | $1,230,531 | 1,862 | $1,074,975 | -359 | -$155,556 |
| SBIR/STTR | 103 | 54,423 | 122 | 59,001 | 105 | 49,788 | -17 | -9,213 |
| Research Project Grants | 2,189 | $1,209,645 | 2,343 | $1,289,532 | 1,967 | $1,124,763 | -376 | -$164,769 |
| Research Centers | ||||||||
| Specialized/Comprehensive | 36 | $66,838 | 32 | $68,861 | 25 | $54,332 | -7 | -$14,529 |
| Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 0 | 50 | 0 | 50 | 0 | 50 | 0 | 0 |
| Comparative Medicine | 0 | 276 | 0 | 276 | 0 | 276 | 0 | 0 |
| Research Centers in Minority Institutions | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Research Centers | 36 | $67,164 | 32 | $69,187 | 25 | $54,658 | -7 | -$14,529 |
| Other Research | ||||||||
| Research Careers | 316 | $53,427 | 337 | $57,575 | 337 | $57,575 | 0 | $0 |
| Cancer Education | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Cooperative Clinical research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Minority Biomedical Research Support | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Other | 62 | 38,339 | 79 | 47,646 | 62 | 37,641 | -17 | -10,006 |
| Other Research | 378 | $91,766 | 416 | $105,221 | 399 | $95,216 | -17 | -$10,006 |
| Total Research Grants | 2,603 | $1,368,575 | 2,791 | $1,463,940 | 2,391 | $1,274,636 | -400 | -$189,304 |
| Ruth L. Kirschstein Training Awards | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 233 | $10,480 | 231 | $10,492 | 231 | $10,492 | 0 | $0 |
| Institutional Awards | 479 | 26,452 | 482 | 27,633 | 482 | 27,633 | 0 | 0 |
| Total Research Training | 712 | $36,932 | 713 | $38,125 | 713 | $38,125 | 0 | $0 |
| Research and Develop Contracts | 180 | $83,037 | 180 | $85,318 | 142 | $67,453 | -38 | -$17,865 |
| (SBIR/STTR)(non-add) | (0) | (109) | (0) | (618) | (0) | (540) | (0) | (-78) |
| Intramural Research | 287 | 181,946 | 296 | 194,674 | 296 | 170,793 | 0 | -23,881 |
| Res. Management and Support | 263 | 83,944 | 267 | 88,239 | 267 | 79,415 | 0 | -8,824 |
| Res. Management and Support (SBIR Admin) (non-add) | (0) | (0) | (0) | (0) | (0) | (0) | (0) | (0) |
| Construction | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Buildings and Facilities | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Total NIMH | 550 | $1,754.434 | 563 | $1,870,296 | 563 | $1,630,422 | 0 | -$239,874 |
1 All items in italics and brackets are non-add entries
2 Of which $43.0 million in FY 2018, $57.5 million in FY 2019, and $70 million in FY 2020 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
[Top]
Major Changes in the Fiscal Year 2020 President’s Budget Request
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity details and these highlights will not sum to the total change for FY 2020 President’s Budget request for NIMH. The FY 2020 President’s Budget request is $1,630.4 million, a decrease of $239.9 million compared to the FY 2019 Enacted level.
Research Project Grants (-$164.8 million; total $1,124.8 million)
Non-competing Research Project Grants funding has increased by $57.0 million. Competing Research Project Grants has decreased by 401 grants or $206.0 million. This reduction is distributed across all programmatic areas and basic, translational or clinical research.
Research and Development Contracts (-$17.9 million; total $67.5 million)
This budget activity has decreased by $17.9 million and will continue to fund research studies conducted by extramural universities and institutions.
Intramural Research Programs (-$23.9 million; total $170.8 million)
This budget activity has decreased by $23.9 million and will continue to fund innovative research studies conducted by the Institute’s intramural scientists.
Research Management and Support (-$8.8 million; total $79.4 million)
This budget activity has decreased by $8.8 million and will continue to support the oversight and management of scientific programs critical to fulfilling the Institute’s mission.
[Top]
Summary of Changes
| FY 2019 Enacted | $1,870,296 | |||
| FY 2020 President's Budget | $1,630,422 | |||
| Net change | -$239,874 | |||
| CHANGES | FY 2020 President's Budget | Change from FY2019 Enacted | ||
| FTEs | Budget Authority | FTEs | Budget Authority | |
| A. Built-in | ||||
| 1. Intramural Research: | ||||
| a. Annualization of January 2019 pay increase & benefits | $66,440 | $54 | ||
| b. January FY 2020 pay increase & benefits | 66,440 | 163 | ||
| c. Paid days adjustment | 66,440 | 251 | ||
| d. Differences attributable to change in FTE | 66,440 | 0 | ||
| e. Payment for centrally furnished services | 31,953 | 0 | ||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 72,401 | 1,838 | ||
| Subtotal | $2,307 | |||
| 2. Research Management and Support: | ||||
| a. Annualization of January 2019 pay increase & benefits | $40,560 | $35 | ||
| b. January FY 2020 pay increase & benefits | 40,560 | 106 | ||
| c. Paid days adjustment | 40,560 | 153 | ||
| d. Differences attributable to change in FTE. | 40,560 | 0 | ||
| e. Payment for centrally furnished services | 6,876 | -362 | ||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs | 31,979 | 774 | ||
| Subtotal | $707 | |||
| Subtotal, Built-in | $3,014 | |||
[Top]
| CHANGES | FY 2020 President's Budget | Change from FY 2019 Enacted | ||
| No. | Amount | No. | Amount | |
| B. Program: | ||||
| 1. Research Project Grants: | ||||
| a. Noncompeting | 1,560 | $881,375 | 42 | $50,434 |
| b. Competing | 302 | 193,600 | -401 | -205,990 |
| c. SBIR/STTR | 105 | 49,788 | -17 | -9,213 |
| Subtotal, RPGs | 1,967 | $1,124,763 | -376 | -$164,769 |
| 2. Research Centers | 25 | $54,658 | -7 | -$14,529 |
| 3. Other Research | 399 | 95,216 | -17 | -10,006 |
| 4. Research Training | 713 | 38,125 | 0 | 0 |
| 5. Research and development contracts | 142 | 67,453 | -38 | -17,865 |
| Subtotal, Extramural | $1,380,214 | -$207,169 | ||
| FTEs | FTEs | |||
| 6. Intramural Research | 296 | $170,793 | 0 | -$26,188 |
| 7. Research Management and Support | 267 | 79,415 | 0 | -9,531 |
| 8. Construction | 0 | 0 | ||
| 9. Buildings and Facilities | 0 | 0 | ||
| Subtotal, Program | 563 | $1,630,422 | 0 | -$242,888 |
| Total Changes | -$239,874 | |||
[Top]
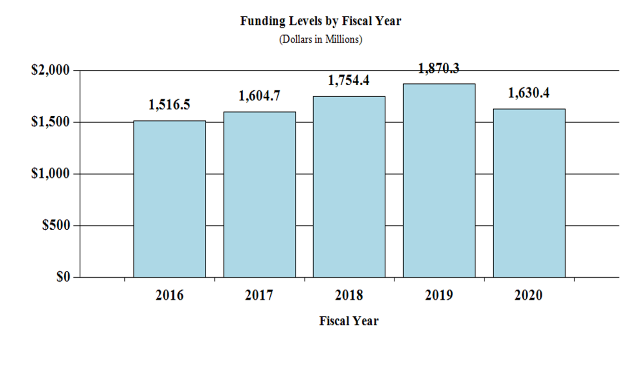
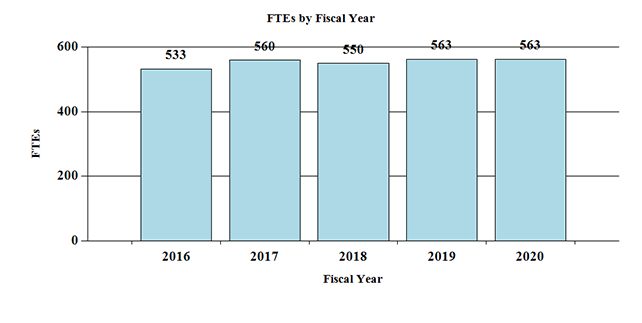
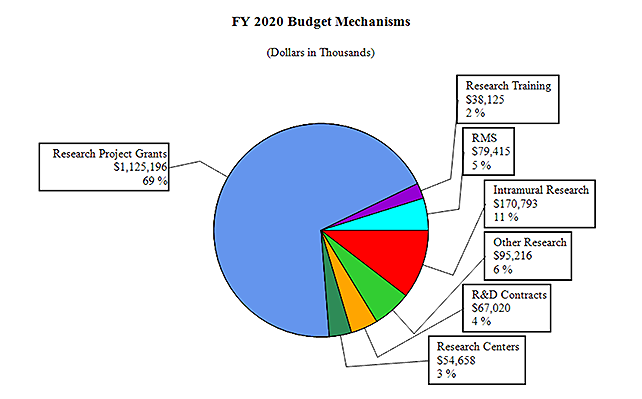
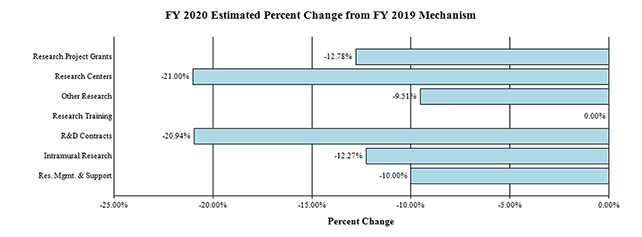
Fiscal Year 2020 Budget Graphs
History of Budget Authority and FTEs:
Distribution by Mechanism:
Change by Selected Mechanism:
[Top]
Budget Authority by Activity
| FY 2018 Final | FY 2019 Enacted | FY 2020 President’s Budget | FY 2020 +/- FY2019 | |||||
| Extramural Research | FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount |
| Detail | ||||||||
| Neuroscience & Basic Behavioral Science | $731,327 | $789,387 | $687,147 | -$102,240 | ||||
| Services & Intervention Research | 148,730 | 158,153 | 137,669 | -20,484 | ||||
| Translational Research | 403,400 | 429,006 | 373,442 | -55,564 | ||||
| AIDS Research | 159,739 | 162,616 | 139,980 | -22,636 | ||||
| Office of the Director | 45,349 | 48,222 | 41,976 | -6,246 | ||||
| Subtotal, Extramural | $1,488,544 | $1,587,383 | $1,380,214 | -$207,169 | ||||
| Intramural Research | 287 | $181,946 | 296 | $194,674 | 296 | $170,793 | 0 | -$23,881 |
| Research Management & Support | 263 | $83,944 | 267 | $88,239 | 267 | $79,415 | 0 | -$8,824 |
| TOTAL | 550 | $1,754,434 | 563 | $1,870,296 | 563 | $1,630,422 | 0 | -$239,874 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Authorizing Legislation
| PHS Act/ Other Citation | U.S. Code Citation | 2019 Amount Authorized | FY 2019 Enacted | 2020 Amount Authorized | FY 2020 President’s Budget | |||
| Research and Investigation | Section 301 | 42§241 | Indefinite | $1,870,296,000 | Indefinite | $1,630,422,000 | ||
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total Budget Authority | $1,870,296,000 | $1,630,422,000 | ||||||
[Top]
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2011 | $1,540,345,000 | $1,537,942,000 | $1,489,372,000 | |
| Rescission | $13,078,800 | |||
| 2012 | $1,517,006,000 | $1,517,006,000 | $1,460,671,000 | $1,483,068,000 |
| Rescission | $2,802,999 | |||
| 2013 | $1,479,204,000 | $1,483,687,000 | $1,480,265,001 | |
| Rescission | $2,960,530 | |||
| Sequestration | ($74,299,124) | |||
| 2014 | $1,465,782,000 | $1,456,041,000 | $1,446,172,000 | |
| Rescission | $0 | |||
| 2015 | $1,440,076,000 | 1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017[1] | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,601,931,000 |
| Rescission | $0 | |||
| 2018[2] | $1,244,901,000 | $1,668,461,000 | $1,724,568,000 | $1,754,775,000 |
| Rescission | $0 | |||
| 2019[2] | $1,612,192,000 | $1,790,231,000 | $1,871,250,000 | $1,870,296,000 |
| Rescission | $0 | |||
| 2020[2] | $1,630,422,000 |
1 Budget Estimate to Congress includes mandatory financing.
2 Includes funds derived by transfer from the NIH Innovation Account under the 21st Century Cures Act
[Top]
Justification of Budget Request
National Institute of Mental Health
Authorizing Legislation:
Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2018 Actual | FY 2019 Enacted | FY 2020 President’s Budget | FY 2020 +/- FY 2019 | |
| BA | $1,754,434,000 | $1,870,296,000 | $1,630,422,000 | -$239,874,000 |
| FTE | 550 | 563 | 563 | 0 |
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
[Top]
Director’s Overview
The National Institute of Mental Health (NIMH) is the lead federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure. The Institute supports basic, translational, clinical, and services research, including research with potential to improve clinical care over the short, medium, and long-term.
In the United States, an estimated 46.6 million adults suffer from a mental illness, which may be significantly impairing and life-threatening.1 Mental and substance abuse disorders are the third leading cause of disability in the United States, accounting for 12.7 percent of all years lived with disability.2 One of the most tragic outcomes of untreated mental illness is suicide. Suicide accounts for the loss of nearly 45,000 American lives each year; it is the second leading cause of death in youth and young adults aged 10-34, and the tenth leading cause of death overall.3
Transformational Tools and Technologies: To support the development of new tools and technologies to revolutionize our understanding of the brain, NIMH and the National Institute of Neurological Disorders and Stroke co-lead the NIH Brain Research through Advancing Innovative Neurotechnologies (BRAIN) Initiative.4Early research from the BRAIN Initiative focused on producing more comprehensive and dynamic maps of the brain, deepening our understanding of how circuit activity produces an array of complex behaviors, and laying the foundation for understanding how brain circuitry is disrupted in brain disorders, including mental illnesses.5 As the BRAIN Initiative moves forward, NIH is engaging a BRAIN 2.0 Working Group of the Advisory Committee to the Director to assess progress to date and to identify emerging opportunities. NIMH is currently leading the BRAIN Initiative Cell Census Network (BICCN) to provide researchers with a comprehensive reference of the diverse cell types in multiple species. The BICCN recently released its first large data set of over 1.3 million individual cells from the mouse brain and completed molecular profiling on 800,000 human brain cells.
NIMH also supports research on the development of tools and technologies to improve identification of individuals at risk for suicide. Because most suicide decedents have accessed health care services in the 12 months preceding death, health care systems can play a vital role in identifying individuals at risk and preventing suicide attempts.6 NIMH-funded researchers have demonstrated that brief screening tools improve providers’ ability to identify, in health care settings, adults and youth at risk for suicidal behavior.7,8,9 One of these tools, the four-item Ask Suicide-Screening Questions (ASQ) screening tool, helps nurses and physicians identify youth at risk for suicide. The ASQ is now being used in emergency departments, inpatient units, and outpatient primary care clinics around the country. Efforts are also underway to develop computerized suicide risk detection algorithms based on electronic health record data. The Mental Health Research Network (MHRN), a collaborative effort of NIMH, private sector health maintenance organizations (HMOs), and the NIH Common Fund, has integrated the electronic health records for 13 million patients with mental illnesses across 13 health system research centers for a population-based approach to research. Activities of the MHRN include developing and validating a risk algorithm to inform providers about patient risk for suicide following an outpatient visit.10,11
Building on Basic Science: NIMH supports research that aims to understand the basic science that underlies mental illnesses. Advancements in neural circuit technologies, genomics, and drug discovery have allowed us to improve treatments for mental illnesses. NIMH-supported studies in circuit neuroscience have enhanced our understanding of how behavior is produced by neural activity. Through studies that leverage optogenetics, which uses light to alter neural activity, and pharmacogenetics, which uses designer drugs to do the same, researchers have identified neural circuits for learning about threats and rewards in the environment, and for controlling fear.12,13,14,15
NIMH-funded researchers have also identified a large and growing number of genetic differences that are associated with mental illnesses. To further guide the Institute in setting priorities for genomics research, NIMH convened a working group of the National Advisory Mental Health Council.16 The working group recommendations addressed the need for appropriate statistical methods, rigorous significance standards, and well-powered, unbiased studies for gene discovery. The report also highlighted the need to carefully choose and enrich experimental systems to address both common and rare gene variants, and expand efforts beyond current diagnostic classifications. In addition, the working group recommended that studies should aim to capture genetic and phenotypic variation across diverse human populations. This need for diversity drives several NIMH-supported studies, whose findings now provide many examples of statistically rigorous and fully-replicated genetic links to schizophrenia, autism, depression, and other psychiatric disorders. NIMH participation in projects like the Human Heredity and Health in Africa (H3-Africa ) Initiative, is facilitating the study of genomics and epidemiological research in partnership with African scientific institutions.17
Discoveries in neuropharmacology have also helped advance the field toward better treatments. Recently, NIMH-funded scientists deciphered the molecular structure of risperidone – a widely prescribed antipsychotic for schizophrenia, bipolar disorder, and other mental illnesses. This is the first study to elucidate precisely how risperidone binds to its primary molecular target in the human brain. This finding opens the way for the potential design of a new generation of antipsychotic drugs, with fewer side effects.18,19
Exploring the Next Frontier: To truly advance therapeutics, it is imperative to understand the mechanisms underlying mental illnesses. The Research Domain Criteria (RDoC) is NIMH’s framework to investigate the nature of mental health and illness in terms of varying degrees of dysfunctions in general psychological/biological systems.20 While RDoC is currently a top-down, expert-driven approach, there is a critical need for bottom-up, data-driven advances to derive natural domains of behavior. Computational approaches, which allow researchers to describe and test how complex high-level phenomena emerge from interactions at smaller scale levels, will be useful in defining the RDoC domains, connecting them with neurobiology, and testing their clinical utility.21,22 As such, NIMH supports research to validate RDoC constructs in the clinic, and to foster a novel biologically-based computational framework to identify and validate biomarkers and novel treatment, prevention, and recovery targets for mental disorders. For example, NIMH-funded researchers used a mathematical clustering algorithm to identify “biotypes,” different types of brain connectivity maps in people with depression, which may be used to refine diagnosis and guide treatment.23 Further, big data initiatives (e.g., All of Us Research Program24) offer great potential for computational approaches to integrate and continuously refine RDoC into a comprehensive tool that may revolutionize psychiatric research and practice.
As NIMH aims to advance neurotherapeutics to treat mental disorders and the functional domains or symptoms associated with these disorders, the Institute supports research to develop novel neurostimulation and neuromodulation devices25 and interventions.26 Examples of NIMH-funded research advancing neurotherapeutics include investigating noninvasive electrical brain stimulation to improve cognition in schizophrenia,27,28 and testing a computerized intervention targeting cognitive control network deficits in depression.29 These novel interventions aim to improve understanding of underlying brain mechanisms, and also to improve the functioning and outcomes for individuals living with mental illnesses.
Cultivating the Biomedical Research Workforce: To address longstanding challenges faced by researchers trying to embark upon and sustain independent research careers, NIH instituted the Next Generation Researchers Initiative (NGRI) policy.30 In accordance with this policy, NIMH currently funds approximately 80 early stage investigators. One mechanism that NIMH uses to support early investigators is the Biobehavioral Research Awards for Innovative New Scientists (BRAINS). Since 2009, the BRAINS program has helped 79 extraordinary early stage investigators launch innovative research programs with the potential to transform mental health research. BRAINS support the person as well as the project; these awards afford an opportunity for early stage investigators to explore truly novel and potentially groundbreaking approaches, while providing a stable foundation from which to launch their future research programs.
NIMH also recognizes the importance of fostering diversity and talent in its workforce. The BRAIN Initiative, co-led by NIMH, issued funding opportunity announcements to enhance diversity in the neuroscience workforce and maintain a strong cohort of new, talented, independent investigators from diverse backgrounds in BRAIN Initiative research areas.31,32,33 NIMH also continues to support the NIH Blueprint Enhancing Neuroscience Diversity through Undergraduate Research Education Experiences (BP-ENDURE) program. BP-ENDURE offers opportunities in neuroscience research for individuals from underrepresented racial and ethnic groups, individuals with disabilities, and those at economic disadvantage.34
Budget Policy: The FY 2020 President’s Budget request is $1,630.4 million, a decrease of $239.9 million or 12.8 percent compared to the FY 2019 Enacted level.
Program Descriptions
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) provides support for research in the areas of basic neuroscience, genetics, basic behavioral science, research training, resource development, and drug discovery. In cooperation with other NIMH programs and the wider research community, this program ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, could be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance understanding of the basic neurobiology underlying mental illnesses. In Fiscal Year (FY) 2020, DNBBS plans to support research to identify neurophysiological measures in model systems for use as potential assays in treatment development research. In addition, DNBBS will support studies focused on the links between the maturation of brain circuits and behaviors that occur during development, which allow for the emergence of cognitive, affective, and social behaviors that occur later in life.
Program Portrait: Computational Methods to Elucidate the Role of Gene Regulation in Mental Illnesses
Examining genetic risk factors is important for understanding the biology underlying mental illnesses. The development of mental illnesses is influenced by thousands of variations in DNA sequences (i.e., genetic variants), with each variant contributing only small to moderate effects on risk. Understanding the impact of these gene variants is limited by our understanding of the fine-grained molecular and cellular complexity of the brain, and how the brain itself is affected by genetic variation.
While still in development, advances in analysis of single-cell technologies hold promise for mapping the molecular and cellular diversity of the brain at the single-cell level (e.g., BRAIN Initiative Cell Census Network35). Likewise, new ways to measure multiple molecular features that control genes (multi-omics) allow deeper biological understanding from large collections of brain tissues and genetic data (e.g., NIH Genotype-Tissue Expression 36, NIH ENCODE Project 37, NIMH Repository and Genomics Resource38). Computational methods can be used to integrate precise genomic information provided by single-cell approaches with multi-omic information gathered from adult brain tissue samples. NIMH is supporting an initiative that encourages researchers to develop new, or adapt existing, computational and statistical approaches to aggregate, search, and conduct integrative analyses of single-cell and tissue multi-omic datasets from brain samples to achieve new insights into the biology of mental illnesses.39
Budget Policy: The FY 2020 President’s Budget request is $687.1 million, a decrease of $102.2 million or 13.0 percent compared to the FY 2019 Enacted level.
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science to discover the causes, mechanisms, and trajectories of mental illnesses, and that develop effective interventions for individuals across the lifespan. DTR supports research on the characteristics of, and risk factors for, mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and the design and testing of innovative treatments and interventions. As such, DTR-supported research efforts may have intermediate-term impact, and pave the way towards effective ways to treat and prevent mental illness.
One area of high priority for DTR is research to identify biological markers of risk/resilience and targets for intervention. To address this priority, NIMH recently funded a five-year study to understand how early life adversity shapes emotional, cognitive, and brain development.40 This landmark study, which follows mothers and their infants over the first three years of life, characterizes development across multiple levels of analysis, from environmental risk to physiology to neural circuits to behavior. As a result, the study has the potential to define the contributions of modifiable factors (psychosocial adversity, inflammation, and early caregiver support) to the earliest indicators of risk for psychopathology and may pave the way for innovative early interventions. In addition, in collaboration with the NIH Office of the Director, NIMH awarded an administrative supplement to an ongoing longitudinal study of the neurodevelopment of irritability to also include a cohort of children born dependent on opioids.41 Irritability is a shared pathway to many early childhood psychopathologies and has been strongly associated with exposure to various substances. This timely administrative supplement will increase our understanding of how multiple early-life biological, environmental, and social factors confer risk for mental disorders.
Program Portrait: Autism Centers of Excellence (ACE) Program
Since 2007, NIH has supported the Autism Centers of Excellence (ACE) program, an integrative multidisciplinary, coordinated research effort focused on autism spectrum disorder (ASD) causes, trajectories, and interventions. Previously, ACE researchers identified potential subtypes of autism and sex differences in brain structure of children with ASD,42,43,44 and found that early brain changes may help predict ASD among high-risk infants.45,46
To build on these past discoveries, NIH continues to support the ACE program.47 NIMH currently supports the following research grants. Researchers at Yale University are investigating how brain connections in early development, including the prenatal and early postnatal periods, function as early indicators of ASD.48 They also aim to determine if boys and girls with ASD differ in their brain circuity, and plan to evaluate an intervention to improve social functioning in children at high risk for ASD. Researchers at Emory University are examining social interactions in very early infancy to detect the earliest signs of ASD.49 These researchers also aim to identify infant characteristics that predict future treatment response and outcomes. In addition, researchers at George Washington University seek to understand how ASD differs among girls and boys, particularly during the transition from adolescence into adulthood.50 Through collaboration with self-advocates, these researchers aim to uncover information that will help males and females living with ASD better manage the transition to adulthood. Researchers at the University of California Los Angeles are investigating the rare genetic variations contributing to ASD susceptibility in African-Americans, an important population that has not previously been well represented in ASD genetic studies. 51 These researchers also aim to enrich current genetic repositories and improve disparities by facilitating early diagnosis and increasing access to care for this population. In addition, NIMH-funded ACE researchers at Drexel University are evaluating the extent to which early developmental screening lowers the average age of ASD diagnosis and leads to earlier interventions and improved outcomes.52 This research aims to address whether every toddler should be screened for ASD.
Budget Policy: The FY 2020 President’s Budget request is $373.4 million, a decrease of $55.6 million or 13.0 percent compared to the FY 2019 Enacted level.
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental illnesses. DSIR refines and evaluates treatment and preventive interventions for children, adolescents, and adults, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research, including interventions to improve the quality and outcomes of care; organization- and system-level interventions to enhance service delivery; and, strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings. DSIR funds studies that are designed to have near-term impact, targeted at improving care for patients currently suffering from mental illnesses.
To address the alarming rate of suicide among youth and adults, DSIR continues to support research efforts to leverage existing data from basic and clinical research, publicly available social media content, and electronic healthcare records to address questions about suicide predictors and/or outcomes. 53,54,55,56 Some of these projects apply state-of-the-art computational approaches to conduct novel secondary analyses aimed at identifying biological, experiential, and other factors associated with suicide risk, and to ultimately inform targets and timing for intervention. In addition, some DSIR-funded projects use digital health technology which offers unprecedented opportunities to improve our understanding of mental illnesses, track the course of illnesses and recovery, and provide and enhance mental health care. Overall, these projects hold promise for improving the accuracy and timeliness of assessment, facilitating access and delivery of evidence-supported interventions to youth and adults with serious mental illness, and supporting providers in their use of measurement-based, research-informed care.
Program Portrait: Secondary Data Analysis to Examine the Potential Cross-over Effects of Prevention Interventions
A growing body of literature suggests that preventive interventions delivered in childhood improve long-term outcomes related to mental health. Findings indicate that early life interventions that target short-term risk and protective factors can positively impact a broad array of long-term outcomes. Further, early preventive interventions can have unanticipated beneficial effects on outcomes not specifically targeted by the intervention (i.e., cross-over effects). For example, preventive interventions aimed at reducing substance use and emotional problems can prevent suicidal ideation and behaviors. Because these findings are based on a variety of studies using different prevention strategies, it is difficult to draw conclusions about the impact of preventive interventions on a broad scale, and especially for small subgroups and low-base-rate behaviors (i.e., behaviors that occur at a low rate in the general population).
New technological and analytic approaches for harmonizing and integrating datasets increase statistical power, allowing more rigorous assessment of the impact of prevention interventions in general, among specific groups (e.g., sexual minority youth, racial/ethnic minority youth), and for low-base-rate behaviors (e.g., psychosis, suicidal thoughts and behaviors). NIMH is supporting an initiative to encourage harmonization of existing datasets from early life preventive intervention trials to: (1) examine risk and protective factors that impact mental health outcomes in childhood, adolescence, and young adulthood; and, (2) determine whether early life preventive interventions have long-term effects and/or cross-over effects. Harmonized datasets will be submitted to the NIMH Data Archive and will serve as a resource to the research community.57 Using theory-based developmental approaches, this line of research holds promise to: identify targeted preventive interventions for specific subgroups and behaviors; refine preventive interventions to enhance their potency and efficiency; and inform an evidence-base for early life prevention strategies that reduce risk for mental illnesses and suicide.
Program Portrait: Ending Disparities in Mental Health (EDIfy-MH)
NIMH is committed to confronting mental health disparities and understanding how disparities arise, why they persist, and how we might address them. As such, NIMH is directing efforts through a program called Ending Disparities in Mental Health (EDIfy-MH). The goal of this program is to generate research to identify and better understand the genetic, neurobiological, psychosocial, and environmental mechanisms/or factors that underlie mental health disparities. Edify-MH aims to support disparities research in global and domestic settings that addresses the (a) prevalence of mental illnesses, (b) mental illness trajectories, (c) access to preventive and treatment intervention services and (d) quality and outcomes of mental health care.58,59 Domestically, EDIfy-MH encourages research that addresses: racial/ethnic minority groups, sexual and gender minority groups, individuals living in rural areas, socioeconomically disadvantaged persons, or any other subgroup of individuals in the U.S. with documented disparities. On a global level, EDIfy-MH encourages research that addresses: low- and middle- income countries,60 communities in low-resource settings, individuals living in rural areas, socioeconomically disadvantaged persons, and other subgroups of individuals living outside of the U.S. with documented disparities.
Budget Policy: The FY 2020 President’s Budget request is $137.7 million, a decrease of $20.5 million or 13.0 percent compared to the FY 2019 Enacted level.
AIDS Research
The Division of AIDS Research (DAR) supports research and research training that addresses the priority areas outlined in the NIH HIV/AIDS Research Priorities and Guidelines for Determining AIDS Funding. 61 DAR-supported research includes behavioral and social science studies aimed at reducing HIV/AIDS incidence through the development, testing, and implementation of new and improved prevention strategies, improving health outcomes of those living with HIV through improved linkage to care, and adherence to effective treatments. Behavioral and social science research is critical to understanding individual and community acceptance and uptake of prevention and treatment strategies, such that the delivery of these strategies is fully optimized, widely disseminated, and successfully implemented. Moreover, DAR research places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for contracting HIV or negatively impact the health outcomes of those living with HIV.
DAR also supports research to understand, prevent, and treat the neurological dysfunction associated with HIV infection. DAR is participating in cure research by supporting studies to eradicate or silence the HIV virus from biological reservoirs in the central nervous system (CNS). HIV latency within the CNS is critically important to consider in studies of eradication and reactivation. Many drugs designed to eradicate the virus are unable to penetrate the CNS because it acts as a protective reservoir for HIV. This work may also inform methods to prevent or treat the neurological comorbidities of HIV, with targeted research to understand HIV-induced neurological pathology, with emphasis on long-term antiretroviral therapy. Additionally, DAR ensures effective integration of biomedical approaches and multidisciplinary expertise are considered in agency-wide planning efforts, to help achieve an AIDS-free generation.
Budget Policy: The FY 2020 President’s Budget request is $140.0 million, a decrease of $22.6 million or 13.9 percent compared to the FY 2019 Enacted level.
Intramural Research Programs
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research using unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of clinical and basic scientists.
IRP research teams are investigating innovative behavioral treatments and medications for children with severe mood dysregulation or anxiety and are using computational and multimodal neuroimaging approaches to understand adolescent depression. Other IRP scientists are exploring novel medications for treatment-resistant depression in adults, including ketamine and other experimental fast-acting antidepressant medications. Researchers are also working to understand the neurobiological underpinnings of suicide and developing suicide risk screening tools for use in medical settings.
In FY 2018, important scientific advances came out of the IRP. For example, researchers refined a high-resolution imaging method, laminar cerebral blood volume functional magnetic resonance imaging (CBV-fMRI), which allows measurement of human brain activity across cortical layers. Another IRP team further elucidated how the paraventricular nucleus of the thalamus interacts with other brain areas in mediating behavioral responses to stress.62 IRP researchers also showed that the amygdala, a brain region associated with emotional processing, plays a central role in recognizing and guiding eye movement toward faces, important for social behavior.
Budget Policy: The FY 2020 President’s Budget request is $170.8 million, a decrease of $23.9 million or 12.3 percent compared to the FY 2019 Enacted level.
Research Management and Support (RMS)
Research Management and Support (RMS) activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research and training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH programs, regulatory compliance, coordination of global mental health efforts, and liaising with other Federal agencies, Congress, and the public. Through RMS activities, NIMH continues to provide accountability and administrative support for meritorious basic, clinical, and translational research and continues to promote health information dissemination, education, and outreach activities.
Budget Policy: The FY 2020 President’s Budget request is $79.4 million, a decrease of $8.8 million or 10.0 percent compared to the FY 2019 Enacted level.
Budget Authority by Object Class
| FY 2019 Enacted | FY 2020 President's Budget | FY 2020 +/ - FY 2019 | |
| Total compensable workyears: | |||
| Full-time equivalent | 563 | 563 | 0 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $177 | $177 | $1 |
| Average GM/GS grade | 12.7 | 12.7 | 0.0 |
| Average GM/GS salary | $116 | $116 | $0 |
| Average salary, grade established by act of July 1,1944 (42 U.S.C. 207) | $0 | $0 | $0 |
| Average salary of upgraded positions | $135 | $135 | $0 |
| OBJECT CLASSES | FY 2019 Enacted | FY 2020 President's Budget | FY 2020 +/ - FY 2019 |
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | 45,266 | 45,438 | 172 |
| 11.3 Other Than Full-Time Permanent | 23,689 | 23,779 | 90 |
| 11.5 Other Personnel Compensation | 2,094 | 2,102 | 8 |
| 11.7 Military Personnel | 0 | 0 | 0 |
| 11.8 Special Personnel Services Payments | 11,370 | 11,414 | 43 |
| 11.9 Subtotal Personnel Compensation | $82,420 | $82,733 | $313 |
| 12.1 Civilian Personnel Benefits | 23,816 | 24,267 | 450 |
| 12.2 Military Personnel Benefits | 0 | 0 | 0 |
| 13.0 Benefits to Former Personnel | 0 | 0 | 0 |
| Subtotal Pay Costs | $106,237 | $107,000 | $763 |
| 21.0 Travel & Transportation of Persons | 3,012 | 2,861 | -151 |
| 22.0 Transportation of Things | 159 | 151 | -8 |
| 23.1 Rental Payments to GSA | 0 | 0 | 0 |
| 23.2 Rental Payments to Others | 0 | 0 | 0 |
| 23.3 Communications, Utilities & Misc. Charges | 1,013 | 962 | -51 |
| 24.0 Printing & Reproduction | 59 | 56 | -3 |
| 25.1 Consulting Services | 11,324 | 11,220 | -104 |
| 25.2 Other Services | 29,084 | 27,667 | -1,417 |
| 25.3 Purchase of goods and services from government accounts | 169,026 | 140,312 | -28,714 |
| 25.4 Operation & Maintenance of Facilities | 4,774 | 4,773 | -1 |
| 25.5 R&D Contracts | 25,127 | 5,237 | -19,890 |
| 25.6 Medical Care | 136 | 135 | -1 |
| 25.7 Operation & Maintenance of Equipment | 2,730 | 2,593 | -136 |
| 25.8 Subsistence & Support of Persons | 39 | 37 | -2 |
| 25.0 Subtotal Other Contractual Services | $242,239 | $191,974 | -$50,265 |
| 26.0 Supplies & Materials | 6,020 | 5,719 | -301 |
| 31.0 Equipment | 9,493 | 9,018 | -475 |
| 32.0 Land and Structures | 0 | 0 | 0 |
| 33.0 Investments & Loans | 0 | 0 | 0 |
| 41.0 Grants, Subsidies and Contributions | 1,502,066 | 1,312,681 | -189,385 |
| 42.0 Insurance Claims and Indemnities | 0 | 0 | 0 |
| 43.0 Interest & Dividends | 0 | 0 | 0 |
| 44.0 Refunds | 0 | 0 | 0 |
| Subtotal Non-Pay Costs | $1,764,059 | $1,523,422 | -$240,637 |
| Total Budget Authority by Object Class | $1,870,296 | $1,630,422 | -$239,874 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2019 Enacted | FY 2020 President's Budget | FY 2020 +/ - FY 2019 |
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $45,266 | $45,438 | $172 |
| Other Than Full-Time Permanent (11.3) | 23,689 | 23,779 | 90 |
| Other Personnel Compensation (11.5) | 2,094 | 2,102 | 8 |
| Military Personnel (11.7) | 0 | 0 | 0 |
| Special Personnel Services Payments (11.8) | 11,370 | 11,414 | 43 |
| Subtotal Personnel Compensation (11.9) | $82,420 | $82,733 | $313 |
| Civilian Personnel Benefits (12.1) | $23,816 | $24,267 | $450 |
| Military Personnel Benefits (12.2) | 0 | 0 | 0 |
| Benefits to Former Personnel (13.0) | 0 | 0 | 0 |
| Subtotal Pay Costs | 106,237 | 107,000 | $763 |
| Travel & Transportation of Persons (21.0) | $3,012 | $2,861 | -$151 |
| Transportation of Things (22.0) | 159 | 151 | -8 |
| Rental Payments to Others (23.2) | 0 | 0 | 0 |
| Communications, Utilities & Misc. Charges (23.3) | 1,013 | 962 | -51 |
| Printing & Reproduction (24.0) | 59 | 56 | -3 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | 2,084 | 1,980 | -104 |
| Other Services (25.2) | 29,084 | 27,667 | -1,417 |
| Purchases from government accounts (25.3) | 121,640 | 90,857 | -30,784 |
| Operation & Maintenance of Facilities (25.4) | 4,774 | 4,773 | -1 |
| Operation & Maintenance of Equipment (25.7) | 2,730 | 2,593 | -136 |
| Subsistence & Support of Persons (25.8) | 39 | 37 | -2 |
| Subtotal Other Contractual Services | $160,352 | $127,907 | -$32,445 |
| Supplies & Materials (26.0) | $6,020 | $5,719 | -$301 |
| Subtotal Non-Pay Costs | $170,614 | $137,656 | -$32,958 |
| Total Administrative Costs | $276,850 | $244,656 | -$32,194 |
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2018 Final | FY 2019 Enacted | FY 2020 President's Budget | ||||||
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of AIDS Research | |||||||||
| Direct: | 13 | - | 13 | 13 | - | 13 | 13 | - | 13 |
| Reimbursable: | - | - | - | - | - | - | - | ||
| Total: | 13 | - | 13 | 13 | - | 13 | 13 | - | 13 |
| Division of Extramural Activities | |||||||||
| Direct: | 42 | - | 42 | 43 | - | 43 | 43 | - | 43 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 42 | - | 42 | 43 | - | 43 | 43 | - | 43 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 279 | - | 279 | 288 | - | 288 | 288 | - | 288 |
| Reimbursable: | 8 | - | 8 | 8 | - | 8 | 8 | - | 8 |
| Total: | 287 | - | 287 | 296 | - | 296 | 296 | - | 296 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 23 | - | 23 | 23 | - | 23 | 23 | - | 23 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 23 | - | 23 | 23 | - | 23 | 23 | - | 23 |
| Division of Services and Intervention Research | |||||||||
| Direct: | 15 | - | 15 | 15 | - | 15 | 15 | - | 15 |
| Reimbursable: | - | - | - | - | - | - | - | ||
| Total: | 15 | - | 15 | 15 | - | 15 | 15 | - | 15 |
| Division of Translational Research | |||||||||
| Direct: | 25 | - | 25 | 25 | - | 25 | 25 | - | 25 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 25 | - | 25 | 25 | - | 25 | 25 | - | 25 |
| Office of the Director | |||||||||
| Direct: | 136 | - | 136 | 139 | - | 139 | 139 | - | 139 |
| Reimbursable: | 9 | - | 9 | 9 | - | 9 | 9 | - | 9 |
| Total: | 145 | - | 145 | 148 | - | 148 | 148 | - | 148 |
| Total | 550 | - | 550 | 563 | - | 563 | 563 | - | 563 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTE's supported by funds from Cooperative Research and Development Agreements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GS Grade |
| 2016 | 12.4 |
| 2017 | 12.6 |
| 2018 | 12.7 |
| 2019 | 12.7 |
| 2020 | 12.7 |
[Top]
Detail of Positions
| Grade | FY 2018 Final |
FY 2019 Enacted |
FY 2020 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | 175,316 | 176,642 | 177,313 |
| GM/GS-15 | 65 | 65 | 65 |
| GM/GS-14 | 78 | 78 | 78 |
| GM/GS-13 | 108 | 121 | 121 |
| GS-12 | 75 | 75 | 75 |
| GS-11 | 39 | 39 | 39 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 15 | 15 | 15 |
| GS-8 | 8 | 8 | 8 |
| GS-7 | 7 | 7 | 7 |
| GS-6 | 1 | 1 | 1 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 2 | 2 | 2 |
| GS-3 | 1 | 1 | 1 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 1 | 1 | 1 |
| Subtotal | 400 | 413 | 413 |
| Grades established by Act of July 1, 1944 (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 0 | 0 | 0 |
| Ungraded | 173 | 173 | 173 |
| Total permanent positions | 402 | 415 | 415 |
| Total positions, end of year | 574 | 587 | 587 |
| Total full-time equivalent (FTE) employment, end of year | 550 | 563 | 563 |
| Average ES salary | 175,136 | 176,642 | 177,313 |
| Average GM/GS grade | 12.7 | 12.7 | 12.7 |
| Average GM/GS salary | 115,007 | 115,996 | 116,437 |
| 1Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
1 SAMHSA. (2018). Key substance use and mental health indicators in the United States: Results from the 2017 National Survey on Drug Use and Health (HHS Publication No. SMA 18-5068, NSDUH Series H-53). Retrieved from https://www.samhsa.gov/data/
2 Institute of Health Metrics and Evaluation. http://ghdx.healthdata.org/gbd-results-tool accessed July 2017.
3 CDC, NCIPC. WISQARS: http://www.cdc.gov/injury/wisqars/index.html accessed October 2018.
4 https://braininitiative.nih.gov/
5 http://www.jneurosci.org/content/early/2018/06/19/JNEUROSCI.3174-17.2018
6 https://www.ncbi.nlm.nih.gov/pubmed/24567199
7 https://www.sprc.org/micro-learnings/patientsafetyscreener
8 https://reporter.nih.gov/project-details/8755416
10 https://reporter.nih.gov/project-details/9538844
11 https://www.ncbi.nlm.nih.gov/pubmed/29792051
12 https://www.nature.com/articles/s41593-018-0073-9
13 https://www.nature.com/articles/s41593-017-0009-9
14 http://www.nature.com/articles/nn.4414
15 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4526462/
19 https://www.nature.com/articles/nature25758
20 https://www.nimh.nih.gov/research-priorities/rdoc/index.shtml
22 https://www.nimh.nih.gov/about/director/messages/2017/rdoc-outcomes-to-causes-and-back.shtml
23 https://www.ncbi.nlm.nih.gov/pubmed/27918562
25 https://grants.nih.gov/grants/guide/pa-files/PAR-18-942.html
26 https://grants.nih.gov/grants/guide/rfa-files/rfa-mh-16-406.html
27 https://reporter.nih.gov/project-details/9116564
28 https://reporter.nih.gov/project-details/9544319
29 https://reporter.nih.gov/project-details/9518140
30 https://grants.nih.gov/ngri.htm
31 https://grants.nih.gov/grants/guide/pa-files/PAR-18-814.html
32 https://grants.nih.gov/grants/guide/pa-files/PAR-18-813.html
33 https://www.braininitiative.nih.gov/
34 https://neuroscienceblueprint.nih.gov/bp_nih-supported_training/endure_programs.htm
35 https://www.nih.gov/news-events/news-releases/nih-brain-initiative-launches-cell-census
36 https://commonfund.nih.gov/gtex
37 https://www.genome.gov/10005107/the-encode-project-encyclopedia-of-dna-elements/
38 https://www.nimhgenetics.org/available_data/psychencode/
40 https://reporter.nih.gov/project-details/9518320
41 https://reporter.nih.gov/project-details/9713716
42 https://www.ncbi.nlm.nih.gov/pubmed/22123952
43 https://www.ncbi.nlm.nih.gov/pubmed/27343889
44 https://www.ncbi.nlm.nih.gov/pubmed/27566123
45 https://www.ncbi.nlm.nih.gov/pubmed/28202961
46 https://www.ncbi.nlm.nih.gov/pubmed/28592562
47 https://www.nih.gov/news-events/news-releases/nih-awards-nearly-100-million-autism-centers-excellence-program
48 https://reporter.nih.gov/project-details/9560923
49 https://reporter.nih.gov/project-details/9560901
50 https://reporter.nih.gov/project-details/9560900
51 https://reporter.nih.gov/project-details/9388877
52 https://reporter.nih.gov/project-details/9560919
53 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-18-400.html
54 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-608.html
55 https://grants.nih.gov/grants/guide/rfa-files/RFA-MH-17-612.html
56 https://grants.nih.gov/grants/guide/pa-files/PAR-16-236.html
58 https://nimhd.nih.gov/about/overview/
59 https://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-089.html
60 https://datahelpdesk.worldbank.org/knowledgebase/articles/378834-how-does-the-world-bank-classify-countries
61 https://grants.nih.gov/grants/guide/notice-files/NOT-OD-15-137.html
