Blueprint for Change: Research on Child and Adolescent Mental Health
Report of the National Advisory Mental Health Council’s Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment
Department of Health and Human Services
Public Health Service
National Institutes of Health
National Institute of Mental Health
The National Advisory Mental Health Council Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment conducted these deliberations and prepared this report.
Recommended Citation:
The National Advisory Mental Health Council Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment. “Blueprint for Change: Research on Child and Adolescent Mental Health.” Washington, D.C.: 20001.
Single copies of this report are available through:
The National Institute of Mental Health
Office of Communications and Public Liaison
6001 Executive Boulevard, Room 8184
Rockville, MD 20892-9663
Telephone: 301–443–4315
Contents
- Acknowledgments
- Preface
- Executive Summary and Recommendations
- I. A Look Backward: Child and Adolescent Mental Health Intervention Research
- II. A Look Forward: Current Emphases and Future Prospects for Child and Adolescent Intervention Research
- III. Infrastructure and Training
- IV. Future Directions for Child and Adolescent Mental Health Research
- V. Figures
- VI. Appendices
- VII. References
Acknowledgments
We would like to acknowledge the individuals listed below for their contributions to this report.
A special thank-you to all of the members of the National Advisory Mental Health Council Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment, whose dedication and hard work made this report a reality:
Chair
Mary Jane England, M.D.
Washington Business Group on Health
Members
William Beardslee, M.D.
Harvard Medical School
Marilyn Benoit, M.D.
Howard University Medical School & Hospital and Georgetown University Medical Center
Barbara J. Burns, Ph.D.
Duke University Medical Center
Ron Dahl, M.D.
University of Pittsburgh
Mary L. Durham, Ph.D.
Kaiser Foundation Hospitals
Graham Emslie, M.D.
University of Texas, Southwestern
Medical Center of Dallas
Michael English, J.D.
Center for Mental Health Services
Substance Abuse and Mental Health Services Administration
Robert Findling, M.D.
Case Western Reserve University
Robert Friedman, Ph.D.
University of South Florida
Jay Giedd, M.D.
NIMH Intramural Research Program
Regenia Hicks, Ph.D.
Department of Mental Health
Harris County, Texas
Robert L. Johnson, M.D., F.A.A.P.
New Jersey Medical School
Nadine Kaslow, Ph.D., A.B.P.P.
Emory University School of Medicine
Kelly Kelleher, M.D., M.P.H.
University of Pittsburgh
James Leckman, M.D.
Yale University Medical School
Martha Constantine Paton, Ph.D.
Massachusetts Institute of Technology
Paul M. Plotsky, Ph.D.
Emory University School of Medicine
John Weisz, Ph.D.
University of California Los Angeles
Roy C. Wilson, M.D.
Missouri Department of Mental Health
Mark Wolraich, M.D.
Vanderbilt University School of Medicine
Other Contributors to the Report:
Presenters
Deborah C. Beidel, Ph.D., A.B.P.P.
University of Maryland
Michael Davis, Ph.D.
Emory University School of Medicine
Mary Dozier, Ph.D.
University of Delaware
Peggy Hill, Ph.D.
Kempe Prevention Research Center for Family and Child Health, U. of Colorado, Denver
Isaac Kohane, M.D., Ph.D.
Harvard Medical School
David Olds, Ph.D.
Kempe Prevention Research Center for Family and Child Health, U. of Colorado, Denver
Sonja Schoenwald, Ph.D.
Medical University of South Carolina
NIMH Staff Director for Report
Kimberly Hoagwood, Ph.D., NIMH
Associate Director for Child & Adolescent Research
NIMH Staff for Report
Serene Olin, Ph.D.
Daisy Whittemore
NIMH Staff Contributors
Cheryl Boyce, Ph.D.
Rhonda Boyd, Ph.D.
Linda Brady, Ph.D.
Lisa Colpe, Ph.D., M.P.H.
Steve Foote, Ph.D.
Junius Gonzales, M.D.
Della Hann, Ph.D.
Themis Hibbs, Ph.D.
Ann Hohmann, Ph.D.
Doreen Koretz, Ph.D.
Israel Lederhendler, Ph.D.
Victoria Levin, M.S.W.
Ann Maney, Ph.D.
Douglas Meinecke, Ph.D.
Eve Moscicki, Sc.D., M.P.H.
Grayson Norquist, M.D., M.S.P.H.
Molly Oliveri, Ph.D.
Jane Pearson, Ph.D.
Kevin Quinn, Ph.D.
Heather Ringeisen, Ph.D.
Agnes Rupp, Ph.D.
Karen Shangraw Belinda Sims, Ph.D.
David Sommers
Jane Steinberg, Ph.D.
Ellen Stover, Ph.D.
Farris Tuma, Sc.D.
Ben Vitiello, M.D.
Lois Winsky, Ph.D.
Clarissa Wittenberg
With Special Thanks to NIMH Staff:
Karen May, Pamela Mitchell, and Catherine West
Consultants
Ellen Frank, Ph.D.
University of Pittsburgh School of Medicine
Megan Gunnar, Ph.D.
University of Minnesota
Robin Peth-Pierce, M.P.A.
Health Communications Consultant
Roland Sturm, Ph.D.
RAND Health
Eva M. Szigethy, M.D., Ph.D.
Judge Baker Children’s Center
Preface
May 2001
Dear Dr. Hyman:
On behalf of my council colleagues, Drs. Mary Durham and Roy Wilson, it is my pleasure to present to the National Advisory Mental Health Council (NAMHC) the report of the NAMHC Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment. Our workgroup has been inspired by the historic amount of public attention on children’s mental health. This intense interest is apparent in the number of activities that have been undertaken to illuminate progress and identify problems in this area.
All these efforts, ranging from White House conferences and Surgeon General reports to private foundation publications, have arrived at the same conclusion: Findings from research in neurobiology, genetics, behavioral science, and social science have led to an increased understanding of the complex interactions among genetic and socioenvironmental factors and their contribution to child and adolescent mental disorders. Further, a promising number of scientifically proven preventive interventions and treatments are now available. Yet, children, adolescents, and their families continue to suffer enormous burdens associated with mental illness—burdens that are often intergenerational. The central problem is that these scientifically proven interventions are not routinely available to the children and their families who need them. The interventions often fail to take into account the diverse sociocultural context and settings in which they will be implemented and are consequently not sustainable. At the same time, the majority of treatments and services children and adolescents receive in the community have either not been evaluated to determine their effectiveness or are simply ineffective. The gap between research and practice continues to widen; part of closing the gap entails investigating the best methods for deploying evidenced-based approaches in real-world settings.
Our ability to create a promising future for the country depends, in part, on our ability to ensure that all children have the opportunity to meet their full potential and live healthy, productive lives. Meeting this challenge will require the work of many people. The research community must partner with families, providers, policymakers, and Federal agencies providing children’s services, as well as other stakeholders, to create a knowledge base on interventions and services that is usable, disseminated, and sustained in the diverse communities where children and their families live. Equally important to this effort is the need to develop the capacity of the field. A new generation of truly interdisciplinary researchers must be trained to strengthen the science base on child and adolescent mental health research and bridge the gaps within and across research, practice, and policy.
We appreciate the opportunity to provide this report. Together with key stakeholders, and with your help, we hope to chart a new course for the future of child and adolescent mental health research.
Sincerely,
Mary Jane England, M.D., Chair, NAMHC Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment
Executive Summary and Recommendations
In the United States today, one in 10 children and adolescents suffers from mental illness severe enough to result in significant functional impairment. Children and adolescents with mental disorders are at much greater risk for dropping out of school and suffering long-term impairments. Recent evidence compiled by the World Health Organization (WHO) indicates that by the year 2020, childhood neuropsychiatric disorders will rise by over 50 percent internationally to become one of the five most common causes of morbidity, mortality, and disability among children. These childhood mental disorders impose enormous burdens and can have intergenerational consequences. They reduce the quality of children’s lives and diminish their productivity later in life. No other illnesses damage so many children so seriously.
In light of the pressing needs of children and adolescents with mental illness, the NAMHC recommended to NIMH Director Steven Hyman, M.D., that a Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment be established. Dr. Hyman charged this group with reviewing research and training, specifically (1) assessing the status of the NIMH portfolio and identifying research opportunities in the development, testing, and deployment of treatment, service, and preventive interventions for children and adolescents in the context of families and communities; (2) assessing the human resource needs in recruiting, training, and retaining child mental health researchers; and (3) making recommendations for strategically targeting research activities and infrastructure support to stimulate intervention development, testing, and deployment of research-based interventions across the child and adolescent portfolio. This report is the result of their work over the past year.
Ten years ago, after the Institute of Medicine released the report “Research on Children and Adolescents with Mental, Behavioral and Developmental Disorders” (IOM, 1989), the NIMH issued a “National Plan for Research on Child and Adolescent Mental Disorders,” which helped shape the current research agenda. As a result of this national plan, research in the field of child and adolescent mental health has expanded dramatically. Much has been learned about the identification and treatment of mental illness in children. But many issues remain unresolved. Stigma continues to be a significant barrier to mental health treatment for children and their families, despite public education efforts. Scientifically proven treatments, services, and other interventions do exist for some conditions but are often not completely effective. Most of the treatments and services that children and adolescents typically receive have not been evaluated to determine their efficacy across developmental periods. Even when clinical trials have included children and adolescents, the treatments have rarely been studied for their effectiveness in the diverse populations and treatment settings that exist in this country.
Finally, those interventions that have been adequately tested have not been disseminated to the children and their families who need them, nor to the providers who can deliver them. Services for children are often fragmented, and many of the traditional service models do not meet the needs of today’s children and families. In sum, there is a shortage of evidence-based treatment, and much of the evidence that does exist is not being used. As a result, the burden of mental illness among children and adolescents is not decreasing.
In the past few years, this burden has not gone unnoticed. There has been heightened activity in this area, launched by the issuance of the landmark document “Mental Health: A Report of the Surgeon General” (U.S. Public Health Service, 1999), which included a chapter focused on the mental health needs of children. This seminal report marked a turning point in the public focus on mental health by clearly documenting the pressing public health need for effective mental health services and highlighting the scientific advances that now offer hope for individuals with mental illness. An offshoot of that effort, “A Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda” (2000), provided a blueprint for children’s mental health research, practice, and policy. In addition, “The Surgeon General’s Call to Action to Prevent Suicide” (1999) provided a plan to increase awareness and prevent suicide in the United States. Several other reports contributed to this escalating national dialogue, including “Youth Violence: A Report of the Surgeon General” (U.S. Public Health Service, 2001), which reviewed the scientific literature on the cause and prevention of youth violence; “A Good Beginning” (Child Mental Health Foundations and Agencies Network, 2000), a monograph on the importance of children’s socioemotional school readiness; and “From Neurons to Neighborhoods: The Science of Early Childhood Development” (National Research Council and Institute of Medicine, 2000).
This intense national interest in children’s mental health has arisen, in part, from the rapidity of research advances in neurosciences, genetics, behavioral sciences, and social sciences. Progress in developmental neuroscience and genetics, for example, is beginning to illuminate how the brain functions at the molecular, cellular, and neural systems levels. Similar advances have been made in the basic behavioral sciences and in clinical treatment and prevention research targeted at specific childhood disorders. Some of the key findings that will help guide future research are listed below; for an overview of advances in the specific research areas, see Section II.B., Key Scientific Areas of Research.
A Decade of Progress: Key Findings in Neuroscience, Behavioral, Prevention, and Treatment and Services Research
- The impact of genes on behavior is complex; multiple genetic and nongenetic factors interact to produce cognitive, emotional, and behavioral phenotypes. Genes and the environment interact throughout development in ways that are not simply additive; for example, genes influence the nongenetic aspects of development (covariance).
- A child’s environment, both in and out of the womb, plays a large role in shaping brain development and subsequent behavior. Studies of the caregiving environment suggest that extreme environments (such as abuse and neglect) may affect brain cell survival, neuron density, and neurochemical aspects of brain development, as well as behavioral reactivity to stress in childhood and adulthood. Methods to understand the more subtle effects of the environment on synapses and circuits are likely to become available in the near future.
- Research has demonstrated the remarkable plasticity of the brain and, in certain neural systems, the ability of the environment to influence neural circuitry during childhood.
- Researchers have found that difficulties with attentional self-regulation can contribute to behavioral problems and difficulties in school; research tracing normal development and individual differences in these regulatory controls has important implications for advancing understanding of the causes of a variety of childhood disorders in which regulatory deficits are implicated (e.g., attention deficit hyperactivity disorder [ADHD], mood and anxiety disorders).
- Progress has been made on the identification of developmental models that describe how cumulative risk factors contribute to adjustment problems and mental disorders, including conduct problems, substance abuse, high-risk sexual behavior, and depression. Risk factor studies have identified some potent and malleable targets.
- New methodological designs and statistical techniques have been developed to strengthen prevention trials (which are complex by their very nature) and have provided a conceptual basis for designing and evaluating prevention programs.
- Effective treatments, both psychosocial and psychopharmacological, have been developed to improve outcomes for some children and adolescents.
- Research has now documented that psychosocial interventions and services may also enhance the impact of pharmacological treatment.
- Advances in medication treatment are especially promising for several child and adolescent disorders, including ADHD, obsessive-compulsive disorder (OCD), other anxiety disorders (generalized anxiety, separation anxiety, and social phobia), and adolescent depression.
- Major studies are currently underway to test the benefits of psychotherapy, medication, and combined treatment for selected major mental disorders affecting youth.
- Medication management and combined treatments (medication plus behavior therapy) for children with ADHD have been found to be effective in targeting core ADHD symptoms. Combined treatments are effective in improving non-ADHD symptoms (e.g., disruptive behaviors and anxiety symptoms) and functional outcomes (e.g., academic achievement, parent-child relations, and social skills).
- Multisystemic therapy (MST), a treatment approach that addresses both the individual child and the child’s context, is another promising intervention. Multiple trials have indicated beneficial effects of MST for youth with conduct problems. Positive outcomes include decreasing externalizing symptoms and improving family functioning and school attendance.
- Research has also identified treatments that are potentially ineffective or, worse yet, harmful. Some forms of institutional care do not lead to lasting improvements after the child is returned to the community. Some services provided to delinquent juveniles are also ineffective (e.g., boot camps and residential programs); peer-group-based interventions have been found to actually increase behavior problems among high-risk adolescents.
- Research on mental health economics has provided more accurate data on expenditures for mental health services in specialty mental health and general health sectors; 1998 annual expenditures were $11.75 billion, or about $173 per child. This is nearly a threefold increase from the 1986 estimate of $3.5 billion (not accounting for inflation).
- New utilization data indicate that there is an increase in the rate of outpatient mental health service use since the 1980’s; however, only 5 percent to 7 percent of children receive some specialty mental health services, in contrast to an estimated 20 percent with a diagnosable mental disorder.
The Challenges: Developing Effective Prevention Programs, Treatments, and Services
In a field as complex as children’s mental health, developing effective solutions requires coordinated efforts within and across multiple disciplines. The research advances highlighted above, coupled with growing knowledge about clinical interventions and services afford an opportunity for interdisciplinary exchange and integration of knowledge across a range of specialized research areas. However, several issues complicate efforts to undertake interdisciplinary work in the field of child and adolescent mental health.
Development
Children’s rapid growth and development greatly amplifies the complexity of interdisciplinary research. Integrating this developmental perspective is critical to advancing research on child and adolescent mental illness, prevention, treatment, and services. Childhood is characterized by change, transition, and reorganization; understanding the reciprocal influences between children and their environments throughout the developmental trajectory is critical.
Social Context
Another issue that impedes progress is the fact that few of the evidence-based interventions have taken into account the child’s social context. For example, the social context has not been studied in sufficient detail to know whether interventions can be generalized across populations, settings, or communities. The majority of studies on child and adolescent mental health interventions have not attended to differences in race, ethnicity, culture, socioeconomic status, community/neighborhood context, and wider systemic issues. Attending to these factors is critical, particularly for children and families living in poverty. Inattention to these issues becomes most apparent when stakeholders, including families, providers, payers, and community leaders, ask about the relevance of research findings for their communities or populations. While knowledge about the efficacy of treatments is increasing at a rapid rate, the effectiveness and transportability of these treatments to diverse populations and settings are less clear.
Disciplinary Insularity
Another challenge is the insularity of the many disciplines involved in clinical and research training. This insularity threatens to impede progress at precisely the time when rich opportunities for interdisciplinary work exist. For example, the following disciplines are likely to have some component of training relevant to the mission of this report: Psychiatry, pediatrics, developmental and behavioral pediatrics, adolescent medicine, nursing, epidemiology, developmental neuroscience, cognitive and behavioral neuroscience, social work, clinical psychology, developmental psychology, and developmental psychopathology. Other fields that can contribute significantly include public health, anthropology, and economics. Because of the rigors and traditions within each area, it can be extremely difficult to create training programs that cross these boundaries.
Clinical care providers (e.g., pediatricians, family medicine physicians, pediatric nurses, psychiatric nurses, social workers, and others) are also critical to this partnership. The insularity of disciplines that presents research barriers also affects the adoption of research findings in practice settings; it is unlikely that treatment practices developed in one discipline will find their way into other professional disciplines. The fragmentation of systems serving children with mental health needs further complicates interdisciplinary efforts. Thus, clinical providers in primary care are unlikely to adopt mental health screening or early intervention methods developed in child psychology or psychiatry, even though such knowledge may be critical to child mental health promotion and early intervention efforts.
Compounding the problem of insularity is the decline over the past 10 years in the number of new investigators seeking research careers to study child and adolescent mental health. Reports from associations representing child and adolescent physicians suggest that dwindling numbers are choosing to enter research careers. To strengthen the science base on child and adolescent mental health, the research-training infrastructure must be enhanced to support a cadre of investigators who can conduct interdisciplinary research to bridge the gaps among research, practice, and policy.
Overcoming the Obstacles: Establishing Linkages
Despite these obstacles, the prospects for gaining a deeper understanding of the complexities of child and adolescent mental illnesses—what causes them, what interventions are effective, and how to get these interventions to those who need them—are better now than at any time in the past. This report enters the ongoing national conversation and proposes the use of new models for integrating basic research with intervention development and service delivery. It also underscores the importance of using a developmental framework to guide research in child and adolescent intervention development and deployment. Two critical action steps must be taken to move ahead:
- Linkages must be made among neuroscience, genetics, epidemiology, behavioral science, and social sciences, and the resulting interdisciplinary knowledge must be translated into effective new interventions.
- Scientifically proven interventions must be disseminated to the clinics, schools, and other places where children, adolescents, and their parents can easily access them. This means that the science base must be made usable. To do so will require partnerships among scientists, families, providers, and other stakeholders.
While many of these issues have been discussed in other recent reports, among the most important contributions of this report are the strategies it provides to overcome the obstacles outlined above and the direct application of these strategies to child and adolescent populations. This report suggests ways to integrate previously isolated scientific disciplines, with the goals of both creating an interdisciplinary and well-trained cadre of child and adolescent researchers and strengthening the currency of mental health science. This report also provides strategies for linking basic science findings to the development of new interventions and ensuring that they are positioned within the context of the communities in which they will ultimately be delivered. Doing so requires the utilization of a new model of intervention development, wherein factors influencing the ultimate dissemination of the intervention are considered from the start.
Priority Area 1: Basic Science and the Development of New Interventions
The linkages among neuroscience, genetics, epidemiology, behavioral science, and social sciences provide opportunities for increasing our understanding of etiology, attributable risk, and protective processes (their relative potency, sequencing, timing, and mechanisms). Such knowledge is critical for the creation of developmentally sensitive diagnostic approaches and theoretically grounded interventions. One critical piece of knowledge needed is an understanding of the etiology of mental illnesses, which can lead to better identification of “high-risk” groups as the target for these early interventions, as well as “high-risk” or vulnerable intervals in development. Despite our appreciation of developmental perspectives, many evidence-based interventions for children and adolescents continue to represent downward extensions of adult models, with limited consideration of basic knowledge about how causal mechanisms or processes operate or may vary across developmental or sociocultural contexts. Conceptual approaches and developmental theories are needed to guide intervention and dissemination efforts. Information from developmental neuroscience, behavioral science, and epidemiology should be used to formulate competing and testable hypotheses about those developmental processes that lead to mental disorders. At the same time, knowledge gleaned from intervention testing and dissemination research must inform basic research theory and development.
Priority Area 2: Intervention Development, Moving From Efficacy to Effectiveness
The current model of treatment development (typically followed in biomedical science studies) stipulates that such development begin in laboratory settings; that highly specific sample selection criteria be used; that refinement, manualization or algorithm development, and delivery be carried out by research staff (as opposed to practicing clinicians); and that aspects of the service setting where it is ultimately destined to land be ignored. This model creates an illusion that science-based treatments are not meant to be used or usable. This report suggests that a different model of intervention development be followed. This new model requires two strands of research activity: The first strand necessitates a closer linkage between basic science and clinical realities (as described in Priority Area 1); the second strand requires that a focus on the endpoint and its context—the final resting place for treatment or service delivery—be folded into the design, development, refinement, and implementation of the intervention from the beginning. Furthermore, such interventions should be developmentally sensitive and take into account family and cultural contexts. Finally, in order to explain why treatments work, it will be important to identify core ingredients of the intervention, including the mechanisms that led to therapeutic change and the processes that influenced outcomes.
Priority Area 3: Intervention Deployment, Moving From Effectiveness to Dissemination
For evidence-based interventions to be used in clinical practice, knowledge about effective dissemination strategies is needed. The application of the traditional biomedical model of intervention development, described above, does not necessarily lead to interventions that are adaptable, applicable, or relevant to real-world clinical practices. To ensure that the current evidence base is used appropriately, a new genre of scientific effort is needed to better understand factors that influence the transportability, sustainability, and usability of interventions for real-world conditions. Many promising preventive and treatment interventions have not paid enough attention to factors that influence family engagement in services, for example, nor to the broader socioecological contexts and systemic issues that influence access to and use of such services. Such research is critical if the current evidence base on effective interventions is to be brought to scale, sustained in service settings, and made accessible to the children and families in need.
Interwoven among these priorities is the critical need to support interdisciplinary training. To ensure that the next generation of scientists is prepared to integrate the rapid advances in multiple disciplines, interdisciplinary training must be made an integral part of future child and adolescent mental health research.
The Future of Child and Adolescent Mental Health Intervention Research
The development and dissemination of new, research-based mental health interventions for children and adolescents will require that scientists create partnerships with community leaders, families, providers, and other stakeholders. Thoughtful scientific partnerships will also need to be forged across different scientific disciplines if the power and promise of basic neuroscience and behavioral science is to be realized through improvements in clinical care. Significant challenges exist: The ethical complexities underlying new research advances will necessitate careful application of oftentimes elusive principles. Such complexities must be thoughtfully resolved. Furthermore, the rapid pace of technological advances will make it possible to move services away from traditional settings and into innovative venues, such as the Web, chat rooms, or other nonclinic settings. But new technology brings new scientific and practical challenges, and these, too, will require careful deliberation.
This report describes a 10-year plan for advancing research on child and adolescent mental health interventions. This report, framed within a public health perspective and supported by taxpayer dollars, will have merit only insofar as it leads to improvements in the quality of care children and adolescents receive, and thus improvements in the quality of the lives they lead. The toll that preventable, untreated, or poorly treated mental illness takes on children, adolescents, and their families is profound and unacceptable. In the past 10 years a vast amount of knowledge has been garnered about the prevention, identification, treatment of, and services for mental illnesses in children and adolescents. This knowledge can and should be used to improve care. But in the next decade, we must be more exacting. The next generation of child and adolescent mental health science will require a transformation of form, function, and purpose if a true public health model is to be realized and sustained.
Recommendations
To mark this new generation of research, the next section describes the workgroup’s recommendations in three broad areas. The first is the area of interdisciplinary research development on child and adolescent interventions. Recommendations in this section are designed to create interdisciplinary research networks and establish a forum for the creative exchange of collaborative research projects to foster new approaches to common problems. The focus of these networks should be on targeted problems, the solution to which may lie outside the scope of a single discipline. The second area is focused on developing new training initiatives to build a cadre of high-caliber scientists to tackle future problems in child and adolescent mental health. Interdisciplinary research training is needed to provide multiple perspectives on intractable problems. Because we recognize that the viability of such interdisciplinary efforts depends, in part, on continuing advances in specific scientific disciplines, the third set of recommendations is targeted toward advancing programs of research in particular areas. Implementation of all three sets of recommendations may have to be staged and focused to accomplish the goal of disciplined growth.
I. Interdisciplinary Research Development in Child and Adolescent Mental Health
A. Child and Adolescent Interdisciplinary Research Networks (CAIRNs)
We recommend that NIMH create support for the implementation of Child and Adolescent Interdisciplinary Research Networks (CAIRNs) to strengthen and accelerate research on intervention development and deployment. The goals of this initiative are to create a series of interdisciplinary research networks that include research-training support and to encourage collaborative research among scientists from different institutions and disciplines. The primary purpose of the CAIRNs will be to introduce new approaches to common problems and support collaborative and integrative research activities across scientific fields.
We recommend that three types of networks be developed, congruent with the research agenda and mission of NIMH: (1) Developmental Basic Science and Clinical Intervention Networks, (2) Treatments and Services Practice Networks, and (3) Implementing Evidence-based Practice Networks. These three sets of networks are targeted at different sets of research problems in the field of child and adolescent mental disorders. The networks should be set up flexibly to encourage interdisciplinary and integrative activities on shared research goals. The aim of the networks is to provide a framework to foster the development of integrative research teams and to provide flexibility for addressing complex scientific questions.
1. Developmental Basic Science and Clinical Intervention Networks (DBCIs)
These networks would focus on linking developmental processes to basic neuroscience or behavioral science, with an explicit focus on creating new assessment models and interventions. These networks will concentrate on underdeveloped areas that hold promise for understanding developmentally sensitive transition points in children’s lives. An overarching goal will be to map extant knowledge about the functioning of the brain against current behavioral indices within a developmental context. The purpose is not to encourage observational studies of risk factors but rather to develop testable models for enhancing etiologic understanding of disorders, to improve assessment strategies, and to develop new treatment models. DBCI networks could address the following research topics:
- Early environment factors (prenatal and postnatal) that influence the development of neural systems involved in attention, impulsivity, and disruptive behavior
- Behavioral and neurobiological deficits in autistic spectrum disorders (e.g., social cognition as it relates to brain activity and the development of behavioral and pharmacologic interventions for improvement of autistic symptoms)
- Neural bases of habitual or repetitive behaviors
- Effects of stress on brain and behavior development as it relates to the regulation and dysregulation of mood and emotions
- Extinction of fear and regulation of anxiety
- Interactions among temperament, mood, emotion, and cognition (e.g., attentional processing) and their implications for behavioral and learning difficulties
2. Treatments and Services Practice Networks (TSPs)
To encourage interdisciplinary research on the development of new treatments, Treatments and Services Practice Networks (TSPs) should be created. These networks could provide support to facilitate the development of culturally sensitive treatments that are feasible, cost-effective, and readily disseminated. These networks could combine basic science expertise with clinical and services expertise to answer questions related to improving treatment efficacy, effectiveness, and delivery within routine practice. These networks should reflect family, youth, and practitioner input on questions of interests and outcomes. Such networks could include (a) treatment development in partnership with practice communities to create new interventions within service settings, (b) the expansion of treatment trials into routine practice settings, or the (c) expansion of the Research Units on Pediatric Psychopharmacology (RUPPs). TSPs could address the following research topics:
- Development of treatment algorithms for clinical decision-making
- Development of triage guidelines to tailor severity of clinical problems to dosage, intensity, or types of treatments or services
- Development of new psychosocial treatments for delivery within primary care, school-based health clinic, or other community practice settings
- Development of psychosocial treatments that attend to the social-ecological environment of the child and his/her family
3. Implementing Evidence-based Practice Networks (IEPs)
These networks would focus on linking evidence-based interventions to dissemination, financing, and policy research. The Implementing Evidence-based Practice Networks (IEPs) would examine the application of dissemination and quality improvement strategies for implementing the scientific knowledge base on evidence-based practices for children and adolescents. While the TSPs are designed to develop new treatments and services through connections among basic scientists and providers, the IEPs would focus on studying how empirically supported interventions that already exist (or will exist) can be effectively deployed, sustained, and implemented in diverse communities, with particular attention to cost-effectiveness and quality. The translation would focus on moving efficacy-based findings into a range of practice settings and specifically on encouraging interdisciplinary studies among health economists, behavioral, services and clinical scientists. Critical to this translation is the role of youth and families in defining implementation strategies. The following issues might be the focus of such networks:
- Use or adaptation of empirically tested treatments in community clinic settings where usual care has not previously included such treatments
- Application of evidence-based assessment tools or preventive interventions with young children
- Use of evidence-based practice in primary care and in school-based health clinics
- Use of depression screening and evidence-based treatment for depression in a variety of settings
- Implementation of parenting education in primary care settings
- Studies of factors influencing how practitioners and families manage youth disorders and the use of evidence-based treatments
B. Overall Structure and Characteristics of Networks
- We recommend that all three of these networks include research infrastructure support to enable trainees and junior faculty to obtain training and mentorship in the networks. As feasible, these could be integrated with existing mechanisms. Additional training recommendations are described below in Section II, Interdisciplinary Research Training in Child and Adolescent Mental Health.
- We recommend that the proposals submitted in response to the initiative on CAIRNs be reviewed in-house at NIMH and not through the Center for Scientific Review (CSR). Regardless of the location of the review, program staff should work in conjunction with Scientific Review Administrators (SRAs) to inform Institutional Review Groups (IRGs) about these areas of emphasis.
- Although the three types of networks are focused on different sets of research problems, we recommend that the directors of all the networks meet annually to share research advances, to strengthen training opportunities among the networks, and to plan for expansion or refinement of their interdisciplinary studies. Trainees should be invited to these annual meetings.
- We recommend that NIMH consider co-sponsorship from other Federal agencies in developing and funding these CAIRNs, where appropriate.
II. Interdisciplinary Research Training in Child and Adolescent Mental Health
A. Capacity Building
- We recommend that NIMH develop a payback program whereby individuals who pursue careers in child and adolescent research may apply for loan forgiveness.
- We recommend that NIMH develop additional mechanisms to support mentoring for new research scientists in child and adolescent mental health. This program may include funding for sabbatical leaves or teaching/mentoring time, provided in the form of supplements to grants. Funding for teaching/mentoring time is critical because there are so few clinical investigators, all with multiple demands on their time.
- To build the research capacity needed to take advantage of the promise of interdisciplinary research, we recommend that NIMH issue a new initiative for the creation of Child and Adolescent Interdisciplinary Training Institutes (CITIs). Basic requirements would include training or exposure in at least the following scientific areas: basic behavioral and neuroscience, epidemiology, prevention, intervention development, services research, and health economics. Training seminars, summer institutes, and intensive coursework on methodology, statistics, and the range of service settings where mental health services are typically delivered (e.g., schools, primary care, community clinics) would be required. To initiate CITIs, we recommend that NIMH establish one or two pilot educational research experiences in interdisciplinary and developmental research with the explicit focus of encouraging child and adolescent studies. The overall purpose would be to work out pragmatic and feasibility issues in detail in at least one or two universities on how to effectively integrate basic and clinical training for clinically oriented investigators. Successful pilot programs would serve as models for further interdisciplinary training programs. We also recommend that the directors of the CITIs meet annually to discuss training initiatives and new programs and to modify educational objectives as needed.
- We recommend that a special announcement be issued for child and adolescent research supplements. Modeled along the lines of minority supplements, they would be used to encourage investigators in other fields (e.g., adult mental health, primary care, education, neurology) to receive training in child and adolescent mental health and thus increase the numbers of investigators with expertise in child mental health research.
- We recommend that NIMH develop a national mentorship program to increase the number of racial/ethnic minorities among NIMH-funded trainees who can address the unique needs of minority children. This mentorship program could include the NIMH Intramural Research faculty. Such an effort is critical in light of changing demographics; minority children are increasingly represented among those with significant mental health needs.
B. Partnerships To Facilitate Research Training
To enhance child and adolescent research training activities, NIMH should explore opportunities to partner with other Federal agencies. Potential partners include the Maternal and Child Health Bureau (MCHB) and the Agency for Healthcare Research and Quality (AHRQ), Health Research and Services Administration (HRSA); the Center for Mental Health Services (CMHS) and the Center for Substance Abuse and Prevention (CSAP), Substance Abuse and Mental Health Services Administration (SAMHSA). For example, NIMH should consider MCHB’s Leadership in Education in Neuro-developmental Disabilities (LEND) programs as an avenue for including more of a mental health perspective.
III. Recommendations for Program Development in Specific Research Areas
A. Neuroscience
- We recommend that databases of rodent and human brain maps be established and supported. We particularly emphasize that these databases need to have a developmental dimension.
- We recommend that cross-institute initiatives be fostered to establish genomic databases.
- We recommend funding program projects to bring together investigators from a variety of disciplines to examine the developmental effects of well-recognized conditions (e.g., stress and the hypothalamic-pituitary-adrenal axis [HPA] system).
- We recommend that technological and procedural advances be supported that (a) allow scanning of very young normal children, (b) enable the development of non-invasive imaging procedures that can be used on awake behaving primates, and (c) encourage the development of functional magnetic resonance imaging (MRI) which can image potentially powerful rodent models of genetic disease.
- Integrative approaches to studies of brain development and function are needed. Examples include (a) combining techniques of neuroimaging with simultaneous physiological monitoring and/or emotional testing, hormonal measurements, and so on; (b) electrophysiology at both the single-cell and multiunit levels to study molecular and circuit regulation in animal models of behavioral dysfunction; and (c) mutant animal models that allow researchers to study epigenetic determinants of brain development (e.g., constitutively manipulated mice may reveal compensatory developmental changes relevant to behavior).
- A major gap exists in the availability of data relating developmental trajectories across multiple levels of description, from genetic processes to behavioral competencies. Data are needed in the following areas:
- Cross-species differences and correspondences in neural and behavioral development, the impact of differing genetic backgrounds, and the validity of various phenotyping procedures in animals as behavioral markers of psychopathological outcomes.
- Gender differences and the putative actions of gonadal steroids, changes in neurocircuitry with puberty, and their relationship to cognitive, behavioral, and emotional regulation during adolescence.
B. Behavioral Science
- Research is needed on how different components of cognition (e.g., attention, language, memory, social) develop in normative and clinical groups of children in order to shape intervention and preventive strategies. This research can increase our understanding of how children with cognitive deficits associated with mental illness may benefit from intervention efforts and perhaps develop new or compensatory skills. Such studies have implications for the prevention or development of more severe impairments or comorbid conditions.
- We recommend detailed empirical study of the specific psychological and behavioral functions that are impaired in childhood mental disorders. Critical domains include memory, attention, emotional processing, emotional expression, social cognitive capacities, and several dimensions of child temperament. Specifying the nature of disorders in terms of these domains will not only improve nosology, but it will also be critical in making connections to neural substrates and in identifying genetic and experiential factors in etiology. As a result, such an effort will pave the way for the design and implementation of increasingly well-targeted modes of preventive and treatment intervention.
- We recommend research focused on developmental, behavioral, and social regulators of emotions at key transition periods, such as birth and puberty, and social transitions, such as daycare and elementary school.
- We recommend the development of science-based interventions that link the psychophysiological deficits associated with mental disorders (e.g., attention, information processing) with specific functional problems, with the aim of formulating more effective and targeted intervention strategies.
- We recommend that NIMH support the development of measurements of functioning that are both culturally sensitive and multidimensional. New tools and approaches that combine qualitative and quantitative methods are needed to understand issues associated with children from diverse cultures and subcultures. In addition, measurements are needed that complement traditional symptom-based diagnostic systems and serve as outcome indicators in intervention, services, and risk processes research.
- We recommend developing measures and interventions through ethnography. The diagnostic conundrums that plague childhood nosology and the pervasive concern about labeling young children suggest that rigorous ethnographic or other qualitative methods for describing mental illness may be particularly useful in developing interventions that are sensitive to a variety of living environments, communities, and cultural contexts.
- We recommend new behavioral research to identify how providers and families manage children’s disorders and why they do or do not engage in the most effective practices. Behavioral science has significant promise to reveal why treatments are not more widely disseminated, what factors underlie complex health behaviors, and the types of decision-making strategies that guide current practice.
C. Prevention
- We recommend that attention be paid to smaller, focused, and intensive longitudinal studies, informed by basic research.
- Given the extensive number of data sets examining risk and protective factors, we recommend that a workshop be convened to identify opportunities for reanalysis of existing data sets. Examples of questions for such studies would include areas of attributable risk, predictors of resilience, interaction of different types/levels of risks across time, how impairment is affected by context, and the impact of contextual and cultural variables on functioning over time.
- A new emphasis is needed on prevention effectiveness trials, prevention services, and cost-effectiveness of preventive strategies. Studies that focus on service contexts that facilitate or impede the sustainability of preventive interventions are especially needed.
- Prevention research trials, by their nature, require longitudinal follow-up and the use of fairly sophisticated efforts to determine the effects of the interventions. Support for methodology development, especially the analysis of longitudinal data where the phenomena wax and wane, is needed via program announcements or conferences.
- Research on relapse prevention, desistance, and naturally occurring prevention is greatly needed.
D. Psychosocial Intervention
- We strongly urge that treatment studies move beyond assessing outcomes to focus more attention on the mechanisms or processes that influence those outcomes. These mechanisms may involve basic processes at different levels (e.g., level of neurotransmitters or stress hormones, information processing, learning, motivation, therapeutic alliance) and may be mediated by therapeutic approaches (e.g., practicing new behaviors, habituating to external events). Understanding the mediators and moderators of outcomes will be important in identifying the ingredients required for therapeutic change.
- We further recommend that treatment outcome studies assess outcomes beyond child symptom reduction to include functioning across various domains (e.g., school functioning, social interactions, family interactions, adaptive cognitions) to provide a more comprehensive picture of the benefits of psychosocial interventions.
- We recommend that NIMH promote a scientific agenda on the generalizability of psychosocial treatments by targeting funds toward the development or adaptation of psychosocial treatments that are implementable in real-world settings (e.g., schools and primary care), including the transportability of treatments with minority populations. Attention to the impact of development, culture, and context on the effectiveness of psychosocial treatments must be a priority. Such efforts will require the development of new methodologies to address the issue of increased heterogeneity in effectiveness trials, treatment fidelity (flexible vs. rigid adherence to treatment protocols), a clear definition of “treatment as usual,” and the use of appropriate comparison groups.
- We recommend that the psychosocial treatment program target the critical research gaps listed below:
- Comorbidity (e.g., substance abuse and depression, anxiety and depression, medical and psychiatric disorders)
- Potentially life-threatening conditions (e.g., eating disorders, suicide), bipolar disorders, anxiety spectrum disorders, autism, neglect, physical and sexual abuse, early-onset schizophrenia
- Gateway conditions of disorders (e.g., oppositional defiant disorder [ODD] as a gateway to conduct disorders, trauma as a gateway to post-traumatic stress disorder [PTSD], or ADHD as a gateway to ODD/conduct disorder/substance use) to divert onset of more serious disorders or impairments
- Parental mental illness and its influence on the prevention and treatment of child and adolescent mental disorders
- We recommend that priority be given to treatment modalities beyond cognitive behavioral therapy and behavior therapy (e.g., family therapy, Internet-based interventions), studies comparing psychosocial interventions for the same conditions (e.g., comparing combined treatment involving parent training and parent-child relationship therapy vs. child-focused interventions), and studies that address the issue of sequential psychosocial treatments and/or combined psychosocial and psychopharmacology treatments.
- We recommend that NIMH give funding priority to studies of common treatments and services available in the community (e.g., wraparound, treatment foster care, residential care, hospitalization), as they may provide a promising avenue for discoveries of new treatment approaches or strategies.
- Because so few studies have assessed the long-term outcomes of interventions (beyond 5 years), and because assessments of the cost-effectiveness as well as clinical and functional outcomes are needed to determine the benefits of treatment and impact on course of illness, we recommend that NIMH encourage long-term follow-up studies of treated and untreated populations.
E. Psychopharmacology
- We recommend expansion of the RUPPs to include the capacity for launching/conducting large simple trials to study issues such as comorbidity, dosing, and safety and efficacy of medication treatments across diverse cultural populations.
- We recommend increased research on the psychopharmacological management of serious mental illness (e.g., early-onset schizophrenia, bipolar disorder, eating disorders, severe depression) and pervasive developmental disorders (including autism and Tourette’s).
- We recommend that NIMH support the study of nonspecific symptoms that are often the targets of psychopharmacology management in children (e.g., aggression and sleep problems), but that have not been measured specifically. Better assessment measures to identify such symptoms need to be developed so that the symptoms can be assessed across disorders, and trials for these symptoms, independent of disorder diagnosis, may be considered.
- Disorder-based efficacy trials for new medications are currently being conducted for acute treatment, particularly for medications under patent protection. However, very few studies to examine long-term safety and efficacy are supported. We recommend that NIMH support such studies.
- We recommend the development of better study paradigms on psychopharmacology effectiveness, including augmentation strategies, multiple medication strategies, and the use of algorithmic treatments. Rational approaches to the management of comorbid disorders, medication side effects, and treatment resistance are needed.
- Studies examining reasons why patients do or do not follow treatment recommendations are needed. Further, studies are needed on the impact of the long-term use of medications, including their impact on psychosocial functioning.
- We recommend supporting basic and clinical neuroscience research on mechanisms underlying brain development and the biochemical and behavioral actions of psychotropic agents in animals and humans to increase understanding of drug actions in the developing brain and individual differences in treatment response (i.e., variability in optimal dose levels). Further, research on brain imaging to identify subtypes of diagnostic categories may have different treatment intervention implications.
- We recommend that the study of both the short- and long-term consequences (negative and positive) of pharmacological interventions associated with acute, recurrent, and chronic exposure to psychotropic agents on the developing brain be a priority for new NIMH initiatives.
F. Combined Interventions and Services
- We recommend the use of grant supplements to current service effectiveness projects to examine factors influencing the adaptability and sustainability of interventions (e.g., different roles of family in the research process, strategies for engaging families, and ways of increasing or maintaining treatment fidelity).
- We encourage careful attention to issues of defining, characterizing, and operationalizing current practice. Currently, researchers largely ignore usual practice because the variability within and across practice settings makes these processes extremely difficult and complex to measure. Yet, understanding intervention approaches developed in the field is important, as such approaches often reflect the needs of children and families and the constraints of personnel, as well as organizational and system limitations. Most of these studies will not be randomized trials because of the nature of routine practice.
- We recommend studies that examine how existing services (e.g., school-based, case management, mentoring, family support), combined treatments, and novel delivery mechanisms (e.g., Internet-based) can be used to augment clinical interventions to meet the significant needs of children with severe mental illness or those with multiple problems more successfully.
- We recommend studies on the impact of family engagement and choice regarding the acceptability of interventions.
- We recommend that a mechanism such as a B/START (Behavioral Science Track Award for Rapid Transition) be used to establish community collaboration prior to implementing research programs.
- We recommend that NIMH develop a national system or a series of regional systems to track the utilization and costs of child mental health services. The systematic tracking of broad indicators of utilization and costs, such as inpatient days, outpatient utilization by insurance status, and socioeconomic characteristics, would allow a more timely recognition of the effects of major changes in the health care system, including increasing or decreasing inequities. As part of these tracking systems, pharmacoeconomic studies are encouraged. Integration of data (service use and costs) from other settings likely to provide a substantial amount of services (e.g., the education, juvenile justice, and child welfare systems) not captured in the existing health databases is essential.
- New technologies will change care dramatically over the next decade. In addition, delivery of care is moving away from clinic-based models and toward models of patient-centered family care delivered in out-of-office settings, including on the Internet, in the home, in the school, in primary care and other settings. Because this trend is likely to continue, we recommend that studies of nontraditional delivery of services be encouraged and supported through program announcements or special funding initiatives.
G. Dissemination Research and System Improvement
- We recommend that investigators be strongly encouraged to conduct dissemination studies in public sector mental health sites, collaborating with other child-serving sectors. Because of the major activities of the Center for Mental Health Services (CMHS) in promoting systems of care through its Comprehensive Community Mental Health Services for Children and Their Families Program, we strongly endorse the NIMH Program Announcement (PA-00-135), “Effectiveness, Practice, and Implementation in CMHS’ Children’s Service Sites.” This program announcement is sensitive to the need to disseminate evidence-based clinical practice to very high-risk youth receiving services in public sector programs. However, to facilitate meaningful research in these public sector sites, a major technical assistance effort will be necessary to bring together investigators and service sites.
- We recommend that priority be given to research on the factors that facilitate or impede the transportability or sustainability of evidence-based treatments. Factors identified may include extra-organizational factors (e.g., stakeholder involvement, triage system), organizational factors, practitioner behavior factors (e.g., attitudes and readiness to change), and family and child characteristics (e.g., attitudes, preferences, or co-occurring disorders) as they are related to dissemination and uptake of effective clinical services. Such factors may guide the development of incentives to optimize the use and sustainability of evidence-based treatments. Such research is especially needed in communities or populations where disparities in access to mental health care are prevalent, including minority communities and the uninsured.
- We recommend that NIMH consider the use of Small Business Innovation Research program funds for deployment, method/analysis development, or dissemination research to develop new commercial products and potentially expand the range, function, and effectiveness of therapeutic services.
- We support continued partnerships with other Federal agencies in order to capitalize on their dissemination arms. These agencies include those of the U.S. Department of Health and Human Services (HHS)—CMHS/SAMHSA, AHRQ/HRSA, MCHB/HRSA, the Administration for Children and Families, and other NIH Institutes—the Office of Special Education and Rehabilitative Services, Department of Education; and the Office of Juvenile Justice and Delinquency Prevention, Department of Justice, to carry forward research advances in both policy and practice arenas.
- A highly visible national dissemination effort is needed. We recommend the creation of a Dissemination Center. The research focus of this center would include dissemination and sustainability studies, with a special focus on understanding the validity of evidence-based treatments for minority populations. In order to conduct these studies, theoretical and empirical literature on organizational and practice change will need to be critically and creatively addressed, and different approaches to diffusion will need to be tested. Initial work by the center would be to identify experts in the change process from other fields and to utilize them in adopting or adapting the complex provision of mental health care services for targeted children and families.
IV. NIMH Oversight of Recommendations: Monitoring Progress
A. Ethical Issues
- Because of the difficult ethical issues surrounding studies of child and adolescent mental health and the paucity of scientific studies on informed consent, confidentiality, and risk assessment with which to guide investigators, we recommend that priority be given to these issues through workshops, program announcements, and special funding initiatives.
B. Governance and Monitoring of Recommendations
- We recommend that the Associate Director for Child and Adolescent Mental Health Research at NIMH report annually to the National Advisory Mental Health Council (NAMHC) about the implementation of these recommendations. In particular, a report should be provided on changes in the scope of and funding for child and adolescent research.
- We recommend that special consideration be given to elevating funding priorities for child and adolescent grants that reflect the interdisciplinary linkages underscored and highlighted in this report. The objective of these initiatives is to create bridges among differing research traditions, and to do so well will require sustained support.
C. Administrative Oversight Within NIMH
- Because the NIMH Child and Adolescent Research Consortium (CARC) has been highly successful in setting research priorities that cross the divisional structure at NIMH and in encouraging creative initiatives to foster children’s mental health, we recommend that the NIMH CARC be retained and fully supported.
- To increase administrative capacity within NIMH, we recommend that consideration be given to retaining individual expert consultants, as needed, to provide advice to the NIMH director about research directions and priorities in child and adolescent mental health.
I. A Look Backward:
Child and Adolescent Mental Health Intervention Research
A. Historical Context
The first English book on pediatrics is considered to be “The Boke of Chyldren” by Thomas Phaire, published in 1544. Phaire included a lengthy list of “perilous diseases” of children, including, among other illnesses, “apostume of the brayne” (most likely meningitis), bad dreams, and colic. According to Neal Postman in “The Disappearance of Childhood” (1994), Phaire’s book heralded the notion of childhood itself, marking one of the first occasions when childhood as a concept was distinguished as a period of development separate from adulthood.
The concept of childhood mental illnesses, however, did not arise until the late 19th century, and they were typically not seen as unique to children or distinguishable from adult manifestations of mental illnesses until the early part of the 20th century. William Healy established the first child guidance clinic in the United States in 1909. Healy advocated for both the “team approach” and the “child’s own story” in treatment and research (Snodgrass, 1984). The first English-language text on child psychiatry was published in 1935 (Kanner, 1935; Sanua, 1990). Autism and ADHD (then known as hyperkinesis) were recognized as childhood disorders in the 1940’s and childhood depression in the 1950’s. In the 1970’s, during a WHO seminar on the classification of mental disorders for the International Classification of Diseases (ICD), the coding scheme for clinical syndromes in child psychiatry was first suggested. This first multiaxial scheme for children was developed and evaluated in 1975 (Rutter, Shaffer, & Shepherd, 1975) and formed the basis for subsequent classification and refinement in the Diagnostic and Statistical Manual of Mental Disorders (DSM) of the American Psychiatric Association. The United States was required by international treaty to use the ICD for maintaining statistics, and so the DSM for the past three decades has used criteria similar to those used in the ICD.
The DSM is generally deemed to be an authoritative compendium of diagnostic categories for mental illness. It was not until the third edition of the DSM (American Psychiatric Association, 1980) that child and adolescent mental disorders were assigned a separate and distinct section within that classification system. This edition of the DSM was widely read; by 1990 more than 2,300 scientific articles referred to it in title or abstract (Kirk & Kuchins, 1992). The DSM established boundaries over the domain of psychiatric classification and consequently controlled discourse about mental illness, structured research directions, and established the parameters of knowledge, including theoretical understanding, about mental illness.
The recognition that children and adolescents suffer from mental illnesses is thus a very recent phenomenon. The development of treatments, services, and preventive approaches to risk for these disorders is even more recent. However, in the past two decades, stemming in part from the rapid advances in psychopharmacology, in adaptations of adult psychosocial treatments for use with children, and the advent of community-based rather than institutionally based care, the knowledge base on treatments, services, and prevention programs has greatly expanded. In addition, tremendous progress has occurred in mapping and cloning genes for diseases that follow Mendelian patterns in families. However, the discovery of the genes that influence susceptibility to more complex diseases such as neurobehavioral disorders has proceeded slowly. The lack of one-to-one correspondence between genotype and phenotype, and the etiological complexity of common mental disorders such as ADHD, anxiety disorders, mood disorders, and schizophrenia, present considerable challenges for researchers.
In order to harness the avalanche of genomic information being generated from new and evolving molecular technologies, innovative quantitative methods are being developed to foster genome-wide analyses. With these new methods under development to map genes for complex diseases, the field of genetics shows promise of providing insights into the biological underpinnings of these diseases, which will advance current diagnostic, prevention, and treatment efforts. Such insights are critical to understanding how genes contribute to vulnerability or resistance, affect the severity or course of illness, and interact with environmental factors that modify their expression or course. These advances are especially critical for children with neurobehavioral disorders because early onset of such diseases tends to be associated with a greater genetic load. With the growing research focused on the genetic control of the developing brain structure and system, as well as the powerful technology that continues to evolve and provide access to the developing brain, unprecedented opportunities for understanding the etiology of mental disorders, and hence ways to divert adverse developmental trajectories, have been created.
In the past 10 years, families of children with mental illnesses and consumers have taken a much more active role in treatment delivery and service planning. The importance of attending to and engaging families in every aspect of mental health services has become the sine qua non of treatment and care plans. Not only does such engagement represent the only defensible moral platform from which to consider the needs of families and children, it also represents recognition of the fact that solutions to child and adolescent mental illness require the partnership of professionals, families, scientists, and youth themselves.
Treatments for childhood disorders such as conduct problems, anxiety disorders, adolescent depression, OCD, and ADHD have been the primary targets of recent study. In the past 2 years, five reviews of treatment and service studies have been published, summarizing hundreds of studies, most conducted since 1980 (Burns, Hoagwood, & Mrazek, 1999; Child Mental Health Foundations and Agencies Network, 2000; Journal of the American Academy of Child and Adolescent Psychiatry, 1999; Journal of Clinical Child Psychology, 1998; Weisz & Jensen, 1999). These reviews span a host of interventions, including preventive approaches for behavioral problems that may emerge into full-blown disorders, medication and behavioral treatments for attention deficit disorders, and services for multiproblem children. The availability of a range of treatments, prevention programs, and services for children with functional impairments is thus a new phenomenon. It suggests that the situation for families whose children are at risk, or who have developed mental illness, is not hopeless. A scientifically defensible corpus of treatments, services, and preventive interventions now exists.
Yet, despite this progress, the burden of childhood mental health problems is not lessening. Report after report cite the fact that childhood mental health problems and illnesses are common, are on the rise, and impose serious burdens on children and families alike (Achenbach & Howell, 1993; Burns et al., 1995; Knitzer, 1982; Murray & Lopez, 1996; Roberts, Attkisson, & Rosenblatt, 1998; National Advisory Mental Health Council, 1990; Shaffer et al., 1996; U.S. Public Health Service, 1999). The level of unmet needs for services is as high as ever, despite two decades of treatment development and mental health service delivery (Burns et al., 1995; Sturm, Ringel, Bao, Stein, Kapur, Zhang, & Zeng et al., in press; also, see appendix A). There are probably a number of reasons why the burden has not lightened.
Stigma
The reasons for the continued and pervasive level of unaddressed mental health needs among young people in this country are many. One perpetual impediment has been the existence of attitudinal bias or stigma toward mental illness. Mental illnesses have not been accorded the same level of credibility as other health disabilities, yet there is no scientific justification for this difference. Stigma continues to affect families whose children experience mental illness by creating a culture of suspicion, discrimination, fear of mental health problems, blaming the parents, and very real concerns about treatment confidentiality and restriction of insurance coverage.
Fragmentation of Social Institutions
The social institutions primarily responsible for providing mental health support—schools, mental health clinics, and hospitals—remain fragmented and entrenched in models of service delivery that do not match child and family realities. Specialty mental health treatments still tend to be delivered in offices rather than in homes, schools, or health settings. Children with unrecognized mental health problems are still sent to out-of-home placements, often miles away from their families, rather than being treated in communities. The lack of availability and infrastructure support for treatments, prevention programs, and services is as high as it was in the early 1980’s (U.S. Public Health Service, 2000).
Health Disparities
The disparities between minority children and the majority population in health status and access to care have been a source of significant concern (American Academy of Pediatrics, 1994). Mental disorders appear to have equivalent incidence and prevalence across majority and minority populations. However, they may exert a disproportionate impact on racial and ethnic minority groups (NIMH, 2001). This disproportion is evidenced by uneven access to services, poorer treatment, and worse mental health outcomes among minority populations. According to evidence recently presented at the Surgeon General’s Conference on Children’s Mental Health (U.S. Public Health Service, 2000), this finding holds for both children and adolescents. Among this population, unmet need for specialty mental health care is high, and there are substantial ethnic disparities in access to such care (Wells, unpublished data). Racial, ethnic, and cultural differences influence the expression and identification of the need for services (e.g., caregiver expectations), quality of care (e.g., whether or not children receive medication), referral bias or access to appropriate care (e.g., referral to school services or specialty care settings vs. justice or welfare systems for similar problems), the diagnostic process (e.g., lack of culturally competent providers), and hence subsequent care and poorer health outcomes. Similarly, children whose parents are in chronic poverty or who have experienced severe economic losses are at a greater risk for anxiety, depression, and antisocial behaviors (McLeod & Shanahan, 1996; Samaan, 2000).
Resources
Many treatments and services children and their families receive have not been examined or evaluated. A significant proportion of the mental health dollar for children continues to go to treatments and services that have been shown to be largely ineffective or have not been shown to be effective. The question of how to redirect costly residential, hospital, and outpatient (when not evidence-based) resources into more effective care is both a research and a policy issue. The challenge of implementing science-based treatments and services rests not only on good dissemination but also on the realignment of resources to ensure that children and families in need receive the most appropriate care in a timely manner. This requires the research community to partner with families, providers, and other mental health stakeholders and policymakers to realign current resources to ensure that the science base on treatments and services is usable, implementable, disseminated, and sustained in the communities where children live.
Evidence-based Treatments
In the field of children’s mental health science and service deliver, the term evidence-based refers to a body of knowledge, obtained through carefully implemented scientific methods, about the prevalence, incidence, or risk for mental disordres or about the impact of treatments or services on mental health problems.
It is a shorthand term denoting the quality, robutsness, and validity of the scientific evidence that can be brought to bear on questions of etiology, distribution, or risk for disorders or on outcomes of care for children with mental health problems.
Research Gaps
It is significant to note that the evidence base on the effectiveness of preventive programs and treatments for specifiable disorders and services is growing but uneven. Although there is strong evidence for the treatment of many disorders, for others, particularly eating disorders, PTSD, autism and co-occurring conditions, the evidence is minimal. Despite the existence of a growing body of interventions for children, when questions arise as to the extent to which such interventions will match the unique configurations of particular communities, populations, or real-world clinical practices, the limits of the evidence base become apparent. Meta-analytic work has revealed that the effects of psychosocial treatments are as strong for children as they are for adults (Weisz & Weiss, 1993; Weisz, Weiss, Alicke, & Klotz, 1987; Weisz, Weiss, Han, Granger, & Morton, 1995), yet the vast majority of studies on the effectiveness of psychosocial treatments have been conducted in controlled laboratory settings, rather than in the crucible of real-world practices (Weisz, Donenberg, Han & Weiss, 1995; Weisz, Weiss, & Donenberg, 1992). Consequently, the extent to which these evidence-based practices can be transported into the panoply of practice settings is largely unknown.
An additional limitation of the science base on childhood interventions is that for the most part, it is not used. In some cases, a particular treatment has become a standard of care across the country, even though it has produced few positive effects and even negative outcomes for children and adolescents (e.g., the use of group homes or residential treatment centers vs. therapeutic foster care for treating severely delinquent youths). In addition, prevention programs, treatments, and services are not being made accessible quickly enough to children who need help and their families (Burns et al., 1995; Forness & Hoagwood, 1993). Services are not routinely available because of long waiting lists and restrictions in mental health coverage (Friedman, 1992; Wells, unpublished data).
One factor that contributes to the lack of use of evidence-based treatments in naturalistic practice is the pace of their creation: Scientific study of interventions takes time. To properly conduct these studies, a careful sequencing of thought and analysis is required. The current models for scientific progress, however, may be excessively linear and may not be taking advantage of opportunities to develop interventions in the contexts into which they will ultimately be embedded. For example, new models of treatment and service development include attention to features of service contexts (e.g., pediatric health settings, schools, and Head Start programs) that are important to sustaining and perpetuating the quality and fidelity of treatments, as opposed to waiting until the intervention has passed through all phases of scientific testing and development.
Building a clinically relevant and strong base of knowledge about effective interventions for children with mental disorders depends on two factors: One is knowledge about the intervention’s generalizability, impact, and effect on diverse populations; the other is knowledge about the etiologic pathways by which illnesses become manifest. The scientific foundation for knowledge about etiology often arises from basic science or epidemiological studies, which may be able to trace at genetic, molecular, neuronal, or anatomical levels the precursors and pathways to the phenomena we call childhood mental illnesses. Unfortunately, however, as this report will discuss in detail, the opportunities to connect basic neuroscience and behavioral science to the development of new assessment approaches, treatments, or preventions within social contexts have been largely ignored. The rapid pace of discovery in the basic sciences makes this an opportune moment for such translation.
Ethical Issues
Finally, complex issues pervade studies of child and adolescent mental health. The shadow of past scientific misconduct, as well as scientific inattention to the important issues of race, ethnicity, culture, and context, have compromised the ability of science to improve public health for children. In the area of child and adolescent mental health, the ethical issues that are most commonly fraught with dilemma and debate are consent by proxy; balancing risks and benefits, especially for vulnerable populations of children for whom knowledge about risk is very slight (i.e., minority youth, very young children, and children who have been abused or neglected); and the complex role of parents and parent substitutes (such as the State) in granting consent for minors. Other ethical concerns involve ensuring truly informed consent across different populations and systems and attending to racial/ethnic differences in values, attitudes, history, and experiences with science.
B. Recent Activities: The Environment Surrounding Child Mental Health
Over the past several years, a series of national-level activities focused on children’s mental health has taken place. In December 1999, the Office of the Surgeon General released its first-ever report on mental health, with one chapter focused solely on the mental health needs of children (U.S. Public Health Service, 1999). This seminal report marked a critical turning point in the public focus on mental health. Years ago, people with mental illness were doomed to live without prospect for active and productive lives; this report highlighted the scientific advances that now offer hope for people with mental illness and put mental health issues in the forefront of the public health agenda. A public-private White House conference was also held to improve the diagnosis and treatment of children with emotional and behavioral conditions (White House Conference, 2000). This conference was triggered by an article in the Journal of the American Medical Association (Zito, Safer, dosReis, Gardner, Boles, & Lynch, 2000) that reported a dramatic increase in the use of psychotropic medication in preschoolers between 1991 and 1995. The findings from this study raised public concern that very young children, who are in a state of rapid change and growth during their developmental years, are being prescribed potent psychotropic medications even though few data are available on their use. More alarming, the safety and efficacy of these drugs have not been tested in children under the age of 6, and many have not been tested in children under the age of 16. The controversy around psychotropic drug use in very young children raised serious concerns about the appropriate diagnosis and treatment of emotional and behavioral difficulties in children and about the need to take steps to ensure that these children receive appropriate care.
Two other meetings were held to address this issue: The Surgeon General’s Conference on Children’s Mental Health, and the NIMH/Food and Drug Administration meeting on Psychopharmacology for Young Children: Clinical Needs and Research Opportunities. The recommendations from these meetings formed the basis of the “Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda” (U.S. Public Health Service, 2000). This report, an offshoot of the first-ever “Surgeon General’s Report on Mental Health,” highlighted the public health crisis in mental health for children and adolescents and outlined an overarching vision and specific goals to elevate mental health—and the treatment of mental disorders—to a major public health concern. The recommendations bridged the gaps among research, practice, and policy. Specifically, the report called for continued research to develop, disseminate, and implement science-based prevention and treatment services in the field of children’s mental health. In addition, it included other goals pertinent to this report:
- Promote public awareness of children’s mental health issues and reduce stigma associated with mental health
- Improve the assessment of and recognition of mental health needs in children
- Eliminate racial/ethnic and socioeconomic disparities in access to mental health services
- Increase access to and coordination of mental health services
In addition, two significant reports focusing on related issues have been released over the past year. In October 2000, the National Research Council and Institute of Medicine released “From Neurons to Neighborhoods: Science of Early Childhood Interventions.” The report reviewed the explosion of research in neurobiological, behavioral, and social sciences and addressed how the country as a whole could use this knowledge about early childhood development to improve children’s well-being and, in so doing, optimize human capital and ensure the ongoing vitality of the country. In September 2000, the Child Mental Health Foundations and Agencies Network (FAN) released the report “A Good Beginning,” which indicated that social and emotional school readiness is critical for young children’s early school success—and may even set the stage for success later in life (Child Mental Health Foundations and Agencies Network, 2000).
Together, all of these activities highlight our current knowledge base, as well as the enormous gaps among research, practice, and policy. However, this momentum can be harnessed to improve both the evidence base and its use so that service delivery is equitable, just, and effective. Revised models of treatment development are needed to strengthen the evidence base and ensure its uptake.
C. Guiding Principles for the Report
In January 2000, the National Advisory Mental Health Council (NAMHC) Workgroup on Child and Adolescent Mental Health Intervention Development and Deployment was established with the following charge from NIMH Director Steven Hyman, M.D.:
- Assess the status of the NIMH portfolio and identify research opportunities in the development, testing, and deployment of treatments, services, and preventive interventions for children and adolescents in the context of families and communities
- Assess the human resource needs in recruiting, training, and retaining child mental health researchers
- Make recommendations for strategically targeting research activities and infrastructure support to stimulate intervention development, testing, and deployment of research-based interventions across the child and adolescent portfolio
Previous Council reports, including “Translating Behavioral Science into Action” (NAMHC Behavioral Science Workgroup, 2000), have addressed the problem of the lack of connectedness between basic behavioral science and services. Other reports, such as “Bridging Science to Service,” have dealt with the problem of connecting science to service delivery (NAMHC Clinical Treatment and Services Research Workgroup, 1999). Those reports have yielded many useful recommendations, some of which are repeated in this report. However, the applicability of those reports to child mental health issues is complex because of some unique aspects of children, their development, and their contexts, which are valuable to consider. In response to these challenges, the workgroup has framed the following guiding principles, which undergird the thought, interpretation, and recommendations of this report:
- Developmental processes are core to understanding child mental illness prevention, treatment, and services. Childhood is characterized by rapid change, transition, and reorganization, and understanding the reciprocal influences between children and their environments throughout their developmental trajectory is critical.
- Context is critical in understanding childhood mental illnesses. The etiology and course of mental illnesses, including the processes mediating and moderating the expression of symptoms, cannot be understood without reference to the various contexts in which a child lives (e.g., family, peer group, school, community) and sociocultural ecology. The most effective management of childhood mental illnesses and preventive strategies must take into account this context and address the needs of children and their families throughout the child’s development.
- Empirical science must underlie both practice and policy. To provide the most effective interventions possible for the prevention and treatment of childhood mental illnesses, the science base must be linked to practice and used to direct policy, so as to reduce the disparities and gaps in access to effective interventions.
- Interdisciplinary research is key to advancing the understanding of children’s mental health. The rapid advances in various disciplines of science highlight exciting opportunities for integrating a broad knowledge base to advance etiologic understanding of child and adolescent mental health.
- Children’s mental disorders are often chronic. Consequently, evidence-based treatments, prevention programs, and services must be positioned permanently in communities to provide care, over time, to children and their families.
- Equity in care for children’s mental health is essential. Compelling scientific evidence on the critical importance of children’s mental health for learning and development indicates the need for the health system to address children’s mental health in the same way that it addresses physical health.
D. Conceptual Models for the Report
Two broad conceptual models, shown in Figures 1 and 2, also guide the development of this report. The first model addresses the relationship between basic science and child mental health services. The second model describes a developmental framework linking neuroscience, behavioral science, and intervention across the life span. In this section, we describe each model and its relevance to the themes of the report.
Cyclical Feedback Model
A primary goal of this report is to describe, illustrate, and encourage the application of a model for the links between basic science and the provision of mental health services to children and adolescents. This model, depicted in Figure 1, envisions a cyclical sequence of processes. The sequence we envision is never expected to reach a terminus at which all the answers are known and all service interventions are perfected. Instead, any report on the state of the field, at any time, will be a snapshot of a moving target; the body of scientific evidence and the collection of specific “best interventions” will change continually. For this reason, we do not attempt here to provide an exhaustive list of the most important findings of basic science or the best-supported interventions. Instead, our goal—in the model and throughout the report—is to describe a model, or strategy, for building knowledge and building interventions by maintaining a strong linkage between science and practice. Implicit in the model, and throughout this report, is our view that best practice in mental health requires a close connection to the state of the science and that best science requires ongoing feedback from real-world experience.
Figure 1 begins with Basic Research and Theory. This box encompasses basic science with both human and infrahuman species in such fields as learning, development, and neurobiology. In the model, concepts and findings in these fields are used to stimulate Research on Intervention Development and Refinement. Such research may include psychosocial treatments, medications, combined psychosocial-pharmacological interventions, and prevention programs targeting mental health.
Note that the arrow between basic research and research on intervention development is bidirectional, reflecting our view that basic research may both inform and be informed by intervention development research. This bidirectional influence characterizes all pairs of elements or steps in the model, reflecting our view that the connections between science and practice are neither unidirectional nor linear.
Research on intervention development and refinement typically leads to Research on Intervention Testing. Within this box, we envision a continuum of methods, ranging from carefully controlled university experiments with recruited symptomatic youth to randomized trials with clinically referred youth treated in service settings by practicing clinicians. Where a particular study falls along the continuum will be dictated in part by the level of development of the intervention and the goals of the researcher. However, one conclusion emerging from our discussions is that there has been too little research to date on developing and testing interventions in the clinical settings for which they are ultimately intended; this situation has weakened prospects for effective dissemination.
Another element of the model is the Review and Synthesis of Research Findings to Identify Interventions that Work. Here we refer to efforts by reviewers to apply rules of evidence to the clinical trials literature so as to identify specific, empirically supported or evidence-based interventions. Relevant procedures may include systematic literature reviews, meta-analyses, and efforts by various committees and task forces to code studies for their methodological adequacy and gauge the level of support they provide for various interventions. It is not our purpose to produce a comprehensive list of such interventions, but we refer interested readers to a relevant report on child psychosocial treatments that began the process of compiling a list (Lonigan, Elbert, & Johnson, 1998).
A fifth process highlighted in the model is Intervention Deployment. Included here are efforts to take evidence-based interventions into the field and encourage their use by providers, paired with efforts to understand the process, the outcome, and factors that may influence whether the interventions are adopted, whether they are used appropriately, and whether they are beneficial. Thoughtful research addressing these questions about deployment, and what makes it succeed or fail, will certainly require input from providers, community partners, parents and other caregivers, and the children and adolescents the interventions are intended to help. As the diagram suggests, the model holds that information gained via research on deployment should be used to inform each of the other four processes described in the model: Basic Research and Theory, Research on Intervention Development and Refinement, Research on Intervention Testing, and Review and Synthesis of Research Findings to Identify Interventions that Work.
Figure 1
A Model for Effective Deployment and Translation of Science Into Practice
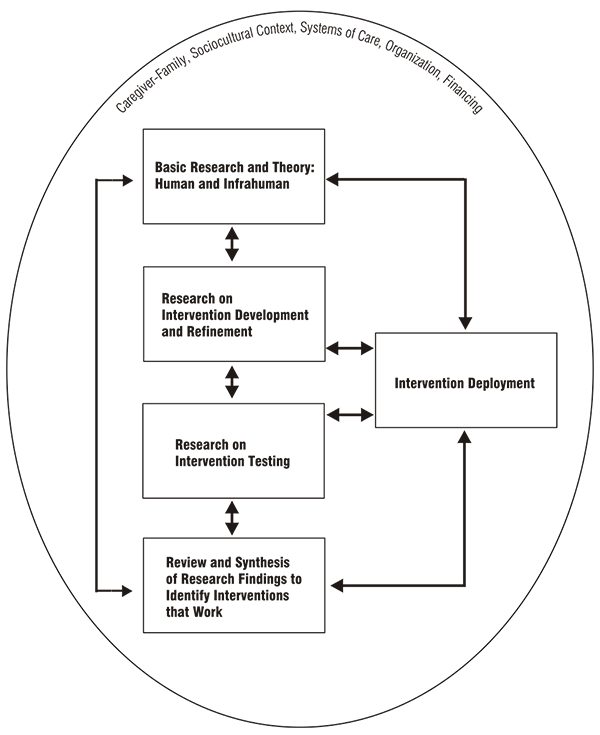
Finally, we consider the multidirectionality and multisequentiality of the model. The spatial layout of the model may suggest a unidirectional sequence in which basic research and theory leads to research on development and refinement of a specific intervention, then to intervention testing. This is followed by review and synthesis that identifies the intervention as empirically supported in multiple studies, at which point the intervention is deployed in service settings. Although this sequence may unfold in some cases, we do not see such a linear progression as essential to progress in the field, and we suspect that it may be unduly limiting. For example, a strong argument can be made that, for some interventions, deployment and outcome assessment in service settings should be a part of intervention development and testing so that problems in treatment delivery in real-world settings may be identified and solved early in the evolution of the intervention. The general point is that the model shown in Figure 1 depicts processes that are needed to keep science and practice linked, but the order of these processes may be quite varied from one intervention to another, and there may be considerable blending of these processes as interventions are envisioned, developed, tested, and disseminated.
Critical to this cyclic feedback model is the involvement of youth, family, providers, and community input at every level of the process to ensure the credibility of the interventions developed. Further, policymakers responsible for the organization and financing of children’s service systems should be involved if the interventions are ultimately to be relevant to the needs of these systems.
Developmental Framework: Linking Basic Science to Interventions
The second conceptual model guiding this report is depicted in Figure 2. As the figure illustrates, a developmental perspective is essential to the task of linking basic neuroscience, behavioral science, and opportunities for intervention. The figure shows a developmental trajectory across stages beginning with conception and gestation, passing through childhood and adolescence, and progressing into adulthood. Across this trajectory, developmental competencies (e.g., physical skills, cognitive abilities, emotional and behavioral regulation) take shape. The growth of these competencies is not a smooth course involving uniform increments, but rather a series of spurts and plateaus. This “bumpy” course of maturation is reflected in the irregular growth curve shown above the developmental stages.
The darkened circles along the timeline represent the interplay of biological and behavioral development at multiple points in development. In the preschool years, for example, biological changes such as myelination, dendritic and axonal arborization, neurogenesis, synaptic stabilization, and sculpting of neural circuits are associated with behavioral changes such as improved regulation of attention and affect, impulse control, and task focus. These changes set the stage for subsequent learning in school settings and for new kinds of social relationships involving empathy and cooperation. These points of biological-behavioral interface represented by the darkened circles along the curve are particularly important to the developmental model and to this report. They illustrate what we believe are exciting opportunities for cross-pollination among neuroscientists, behavioral scientists, and intervention researchers. Enriched collaboration among these disciplines could stimulate a new generation of biobehavioral developmental theory and research and, in turn, new models of prevention and treatment.
Figure 2
Developmental Framework: Linking Neuroscience, Behavioral Science, and Intervention
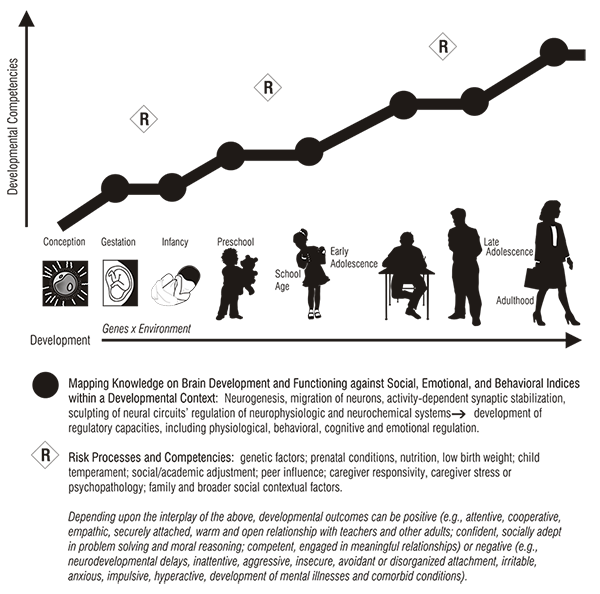
New models of prevention and treatment are needed for diverse forms of risk processes and competencies. We offer a few illustrations in Figure 2, indicated by the letter R. Of course, each form of risk process can be seen as one end of a continuum, at the other end of which is a particular form of competence. A range of developmental outcomes may accrue from the various risk processes and competencies. As an example, low birth weight, irritable temperament in infancy coupled with caregiver stress, attentional deficits, and poor frustration tolerance at school age may confer negative outcomes such as ADHD, learning disabilities, and associated difficulties in peer relations. By contrast, similar early risk processes and neurobehavioral vulnerabilities may be mediated by responsive/sensitive caregiving, enhancing the infant’s frustration tolerance so that by school age, the child is able to persevere on tasks, cooperate with peers and teachers, and become confident and socially adept even in the face of challenges.
A central idea is that at each point in development, biological, behavioral, and environmental processes carry potential risks and potential opportunities for the development of new adaptive skills. An overarching goal of this report is to identify strategies for enriching our understanding of these developmental processes and their interplay, and to foster the development and deployment of interventions that can reduce risk and maximize adaptive skills. Throughout this report, we provide a few examples of evidence-based interventions (Science Cases in Point) to explain aspects of the conceptual models and developmental framework. A clinical case study of childhood-onset depression (see appendix B) is used to illustrate how knowledge generated from interdisciplinary research can be meaningfully brought to bear on clinical practice.
II. A Look Forward:
Current Emphases and Future Prospects for Child and Adolescent Intervention Research
A. Costs, Financing Policy, and Services Utilization: National Estimates
Shifting evidence-based interventions into real-world settings will likely be an expensive endeavor. Before estimating the costs of this effort, the current resource context must first be understood. That is:
How much money is being spent for the provision of specialty mental health services for children and what kinds of services are provided in the United States today?
These funding amounts do not need to remain fixed, even if that were feasible. Instead, what is needed is a starting place to assess the relationship between mental health dollars expended and the number of youth served. A complete estimate is not likely to be attainable, owing to missing information about costs (both direct and indirect) and services provided in other critical child-serving sectors (i.e., education, child welfare, and juvenile justice systems). Treatment dollars and service use in those sectors are significant, given very high rates of need in youth involved with child welfare (up to 50 percent) and juvenile justice (up to 80 percent) systems. Many of the youth in those sectors are high-end or high-cost service users, and the research base for treating this critical subpopulation is more limited than for youth with single disorders. Additional questions that arise out of the relationship between resources and the services provided include:
- What are the characteristics of treated youth—age, ethnicity, and insurance status?
- How much care do they receive?
- In what settings is care provided?
Such information can offer a gauge for considering policies governing fiscal and clinical practices relative to unmet need, including access to care and appropriate provision of care. The service utilization data constitute a measure of access, and that rate, when contrasted with epidemiological estimates of mental health need, creates a measure of unmet need. More challenging is the creation of the link between data on current services use and the appropriateness of care (or the practice of evidence-based treatment), since this link relies on treatment and services research not reviewed here but available in “Mental Health: A Report of the Surgeon General” (U.S. Public Health Service, 1999). Nonetheless, cost and utilization information about the resources used for interventions that lack evidence (i.e., much of the outpatient and most of the institutional care provided) opens the door to consider strategies (policy, training, research) for directing existing resources toward interventions that can more effectively benefit children, families, and society.
In this section, recent national estimates of the direct costs of children’s mental health services and service-use patterns for child mental health services are presented.
Costs of Mental Health Services
Sturm and colleagues (in press; also, see appendix A) have produced the first national estimate since the 1980’s of child mental health expenditures in the specialty mental health and general health sectors. Utilizing the most recent sources of national, regional, and/or State data (including those that are population- or insurance-based), they estimated the annual expenditure at around $11.75 billion. This is nearly a threefold increase from the 1986 estimate of $3.5 billion (not accounting for inflation); this increase may be somewhat less after accounting for inflation, but because the 1986 estimate lacked information about (1) children ages 0–11, (2) primary care/mental health services, (3) psychotropic medications, and (4) private practice, this new estimate is likely to be more complete and accurate. Key findings from this report include the following:
- Based on three national surveys fielded between 1996 and 1998, between 5 percent and 7 percent of children used any mental health specialty services in a year. This average rate is similar to the rate among adults, but it obscures the major differences across age groups. Only 1 to 2 percent of preschoolers used any services; the average rates increased in older children—6 to 8 percent of children ages 6 to 11, and 8 to 9 percent of adolescents ages 12 to 17.
- There is substantial variation in mental health service use by type of insurance, ranging from 8.4 percent for Medicaid enrollees to 4.0 percent for the uninsured. The intensity of outpatient care (number of visits) differs similarly. Specialty mental health estimates per 1,000 children per year range from 1,300 visits for Medicaid, 462 visits for private insurance, 391 visits for other types of insurance, and 366 visits for the uninsured.
- Mental health utilization varies across racial/ethnic groups. Among white, black, Hispanic, and other youth, Hispanics are the least likely of all groups to access specialty care (5 percent), even though they and black children have the highest rates of need (10.5 percent), according to measures in the National Health Interview Survey (NHIS). Approximately 7 percent of the families with a child with need (based on NHIS measures) claimed financial barriers as the reason for not getting any mental health care.
- More than half of all outpatient specialty mental health services for children with private insurance are provided out-of-plan. The education sector likely provides a substantial portion of these services.
- Regarding inpatient mental health care, between 0.2 percent and 0.3 percent of children ages 1 to 17 use inpatient mental health services in community hospitals. This rate is much lower than the 0.6 percent rate for adults. Across all insurance types, adults and adolescents have more inpatient days per 1,000 population than do young children. Among the privately insured and the uninsured, adolescents have higher inpatient service use than adults. In contrast, among the publicly insured, inpatient days per 1,000 population are significantly higher for adults than for adolescents.
- Annually, 4.3 percent of children receive psychotropic medication, and utilization is concentrated among older children, with 5 percent of children ages 6 to 11 and 5.6 percent of adolescents on psychotropic medication; only 0.7 percent of children ages 1 to 5 used any such medication.
- Total 1998 treatment expenditures for children are estimated to be approximately $11.75 billion, or about $173 per child. Adolescents ages 12 to 17 account for 59 percent of the total, and also have the highest expenditure per child at $291; children ages 6 to 11 account for 34 percent of the total at $165 per child, and children ages 1 to 5 account for 7 percent of the total at $39 per child.
- Across service expenditures, outpatient services account for 57 percent ($6.7 billion), inpatient services for 33 percent ($3.9 billion), psychotropic medications for 9 percent ($1.1 billion), and other services for 1 percent ($0.1 billion) of the total.
- Across children’s insurance status, children with private insurance account for 47 percent ($5.5 billion), Medicaid enrollees for 24 percent ($2.8 billion), children with other public insurance for 3 percent ($0.4 billion), and the uninsured for 5 percent ($0.6 billion) of the total. State/local expenditures (21 percent or $2.5 billion) could not be allocated by child insurance status.
- Total 1998 expenditures on psychotropic medications for children are estimated to be $1.1 billion. The largest proportion of expenditures was for stimulants, which accounted for slightly over 40 percent of the total. Antidepressants made the second largest contribution to these costs, accounting for 33 percent of the total.
Observations about these data are both encouraging and discouraging. On the positive side, there is an increase in the rate of outpatient mental health service use since the 1980’s. This rate is still, however, well below the estimated need for care; only 5 to 7 percent of children receive some specialty mental health services, in contrast to an estimated 20 percent with a diagnosable mental disorder (U.S. Public Health Service, 1999). There has been a significant decrease in the proportion of mental health dollars spent on institutional care since the last national estimate of costs and service use (Burns, 1991), but the rate of hospital use has changed little since 1986. The reduction in the percentage of institutional care costs is largely attributable to reductions in length of stay, second to discounting inpatient rates, and third to other factors such as the rise in outpatient treatment.
The finding here is that of a reduced proportion of the mental health dollar being spent on institutional care. In absolute value, the cost of institutional care has actually doubled (not adjusted for inflation) since the 1986 estimate (Burns, 1991). Despite the decrease in this proportion, the fact that one-third, or $3.9 billion, is used for institutional care (and this does not include residential care reimbursed by child welfare or education, or detention in juvenile justice) raises a serious question about the availability of evidence-based community alternatives to hospital care. The question of how to redirect both hospital and outpatient resources (when not evidence-based) into more effective care is both a research and policy issue. Further, studies to identify the necessary and appropriate use of inpatient care are needed, as are studies to examine the relationship between the availability of comprehensive community-based services and the use of inpatient treatment. Stronger evidence of cost-effectiveness of community-based interventions could also be of use to policymakers considering changes in reimbursement and treatment strategies.
Access to any type of mental health service appears to be a problem for the multiple groups identified above. Medicaid coverage is clearly instrumental in creating access to services; of note is that uninsured youth receive care at half the rate of their Medicaid counterparts. Preschool-age children rarely receive any care, and racial disparities in service use persist despite higher rates of need. The preceding access issues require attention to understand their origins (e.g., lack of culturally competent and developmentally appropriate services, stigma, or lack of insurance coverage) and to identify strategies for overcoming them. The variation in the number of specialty mental health visits based on type of insurance raises an appropriateness of care question. Although the adequacy of care cannot be fully determined without more information about the specific type and amount of care per treated child, it is clear that uninsured and privately insured youth are at a disadvantage compared with Medicaid-insured youth.
B. Key Scientific Areas of Research
To illustrate the potential of the science base for improving mental health care for children, adolescents, and their families, this section systematically highlights progress from key scientific areas, including basic neuroscience, behavioral science, prevention, treatments, and services. Each subsection delineates opportunities for crossing the boundaries to link knowledge bases, identifies obstacles that present research challenges, and outlines specific recommendations for knowledge development within each area that can facilitate interdisciplinary efforts to solve targeted problems in child and adolescent mental health.
1. Basic Neuroscience
Progress
Basic developmental neuroscience research involves examining childhood alterations in molecular, cellular, and integrative brain functions that are responsible for the development and/or expression of complex mental disorders. The major goal of such research is to translate and integrate findings from basic neuroscience into clinical investigations in order to develop and test specific hypotheses about the neurobiological substrates and etiologies of complex mental disorders. Such investigations include early-life neural antecedents of disorders that are expressed later in life, neural substrates of disorders that appear during childhood, neural circuitry activity, and genomic manipulations.
In the prolonged dialogue about the crisis in children’s mental health, it is easy to identify the pressing need for the societal prevention, identification, and development of interventions. The deficiencies in the latter are frequently so staggering that even the brightest scenarios for solutions from basic neuroscience research seem likely to make only small contributions toward the alleviation of the problems. However, research into the environmental and genetic interactions that bring about brain and behavioral development must run in parallel with psychological and sociological solutions to the problems faced by children in our society if lasting solutions to these problems are to be achieved. Knowledge pertaining to the natural history and organic nature of mental illness and to its etiology during childhood will be fundamentally important in establishing credible milestones of improvement as a result of behavioral intervention. Such knowledge is also vitally important for accurately diagnosing mental illness and developing early interventions. In addition, the identification of the biological bases of emotional and cognitive dysfunction should help to alleviate the social stigma associated with poor mental health. This stigma curbs societal efforts to provide both adequate child-care and medical coverage, and also keeps families from seeking professional help even when medical coverage is available.
After nearly four decades of research into the cellular and molecular bases of brain development, there is one unassailable conclusion: The developing child’s environment, both in utero and ex utero, plays a large role in shaping his or her brain circuitry and subsequent behavioral performance. Poor nutrition, physical or emotional abuse, neglect that produces prolonged stress, substance abuse, and environments that do not evoke active participation have been shown to produce detrimental effects on brain cell survival, neuron density, brain vascularization, and the normal development of brain circuitry. For many of these risk factors, there are strong data supporting behavioral correlates of these anatomical and physiological changes. It is very reasonable to expect that even if, having survived some of these insults, a child matures into a competent adult, there is a high probability that he or she will suffer some emotional or cognitive handicap that prevents optimal function. This is a waste of human resources.
It also has been demonstrated that the early plasticity of brain circuitry can play a positive role in optimizing the brain for the environment in which it develops. This has been most dramatically illustrated in functional imaging studies of individuals born with sensory deficits and therefore forced to use other modalities for the basic skills of reading or speaking. Brain regions not normally utilized in such skills are incorporated into new brain circuits. However, this adaptation occurs only if the unusual modalities are utilized for these purposes during early childhood. Such findings suggest that a mechanistic understanding, or even a behavioral, time-line keyed map of functional human brain development could help educators and clinicians to develop far more efficient strategies for using brain plasticity to facilitate learning or to aid in recovery from disease or trauma.
A growing number of linkage studies of families with emotional disorders and breeding studies of animals also make it clear that the genetic makeup of an individual will play a role in the behavioral and cognitive outcome of nongenetic effects on brain development. Genetic manipulation is one of many potential techniques for creating animal models of mental illness, and such work has revealed critically important information about disease processes at the cellular and molecular levels. Unfortunately, in almost all instances, the way the genetic program of brain development interacts with epigenetic or environmental factors is not understood. Despite the explosion in neuroscience research within the past decade, we are still far from understanding the brain loci that are altered or involved when behaviors involving perception, projection, learning, memory, and emotion are performed, even in adults. We are even further from understanding how these areas change or evolve as children’s cognitive abilities develop.
Some animal research has begun to illuminate the interplay between genes and environmental factors. Francis and colleagues (1999) at McGill University have found that normal variations in maternal care predict patterns of maternal care displayed by the adult offspring. In the rat, variations in maternal care (measured as frequency and duration of licking and grooming behaviors) appear to influence the development of behavioral and endocrine responses to stress in the offspring. Remarkably, they found that if the pups born to low licking and grooming mothers were cross-fostered by high licking and grooming mothers, these pups grew up to be high licking and grooming mothers. The opposite was also true: The pups born to high licking and grooming mothers when cross-fostered by low licking and grooming mothers grew up to be low licking and grooming mothers. The results of cross-fostering studies reported here provide evidence for (1) a causal relationship between maternal behavior and stress reactivity in the offspring and (2) the transmission of such individual differences in maternal behavior from one generation of females to the next. Moreover, an environmental manipulation imposed during early development that alters maternal behavior can then affect the pattern of transmission in subsequent generations. It is important to note that the low licking mothers and pups showed heightened stress responsivity as adults and were more anxious and fearful of novel environments. Taken together, these findings indicate that variations in maternal care can serve as the basis for a nongenomic behavioral transmission of individual differences in stress reactivity across generations. The next phase of this research is seeking to identify critical behavioral and neurochemical changes associated with the effects of early environment on later susceptibility to adverse effects of stress. These studies are relevant to understanding predisposing factors contributing to the development of anxiety and depression in humans.
This line of research is directly in line with Field’s work on tactile stimulation. She found that infants of withdrawn, depressed mothers show dysregulation as early as the neonatal period (unresponsive behavior, low activity level, indeterminate sleep, low vagal tone, right frontal electroencephalogram [EEG] activation, elevated norepinephrine, and low dopamine levels). Infants of mothers who remain depressed for 1 year after birth have a distinct profile of behavioral, physiologic, and biochemical dysregulation. Their mothers also have a distinct profile that can be used to target those in need of intervention (Field, 1998). These interventions may include mood induction, massage therapy, interaction coaching, and natural buffers such as nondepressed fathers and caregivers. The next phase of this research will work on identifying infants of depressed mothers who are most at risk, as well as suggesting specific interventions for the depressed mother-infant dyads with a different profile.
This line of work is also consistent with Hammen’s and Kendler’s work on depression, which shows the relevance of stressful life events on the development and recurrence of depression (Hammen, Henry & Daley, 2000; Kendler et al., 1995; Kendler, Karkowski, & Prescott, 1999; Kendler, Kessler, Neale, Heath, & Eaves, 1993; Kendler, Thornton, & Gardner, 2000; Kessler, 1997). For example, Hammen and colleagues (2000) tested a stress-sensitization version of a diathesis-stress approach to depression. In a 2-year longitudinal follow-up design, exposure to stressful life events was examined in young women in the transition to adulthood. The authors hypothesized that those who had experienced one or more significant childhood adversities would have a lower threshold for developing a depressive reaction to stressors. Results indicated that women with exposure to one or more childhood adversities—such as family violence, parent psychopathology, or alcoholism—were more likely to become depressed following less total stress than women without such adversity. The results could not be accounted for by chronic stress or prior depression. Both biological and psychological sensitization mechanisms may be speculated to play a role, but the actual mechanisms of stress sensitization remain to be explored.
Crossing the Boundaries
Future neuroscience research is focusing on the etiologic role of genes and key environmental factors to understand how genes and the environment interact to produce illness, and to clarify how these risk factors differentially affect gender, stage of development, and cultural/ethnic groups. Insight will be gained into the role of genetic and environmental factors in the etiology of comorbidity. In addition, the development of multivariate genetic models, which include specified environmental risk factors, will provide realistic etiologic models that incorporate all major risk-factor domains. To do this, models of pathogenesis are needed that can be refined and tested both in the laboratory and in the community.
NIMH has already begun to support some efforts to facilitate the translation of basic science knowledge. Several innovative networks have been brought together through a translational research initiative. One such network is investigating the links between glucocorticoid and early experiences in rodents and its potential for helping to explicate disorders related to early adverse conditions in humans. The network comprises animal researchers, developmental psychologists, psychiatrists, and mental health services researchers who have met over the past 2 years to examine the relation between stress and the hypothalamic-pituitary-adrenal axis (HPA). After a thorough discussion of ideas, the group identified potential linkages and is now developing feasible research studies that take advantage of the advances at the interface of basic animal models, neuroscience, and services research to begin to clarify how behavioral and biological factors may interact in the etiology, course, and amelioration of psychopathology.
Obstacles and Gaps
Broadly speaking, there are four reasons why progress in this area is slow. First, there is still relatively little innovative interaction between clinical research and basic neuroscience research focused on animal models. For example, a review of the NIMH research portfolio shows many studies dealing with the genetics, physiological correlates, environmental determinants, and occasionally gender differences of psychological disorders such as depression, borderline personality disorder, anxiety disorder, tic disorders, schizophrenia, and autism. All of these disorders affect children or have their onset in adolescence. However, studies are needed using certain animal models of behaviors that have some of the correlates of the human condition in order to study the cellular and circuit basis of the dysfunction. This cross-disciplinary work, or translational research, may ultimately provide more accurate explication of brain dysfuntions that lead to mental illness.
Even in tractable animal models, such as the rodent, where the vast majority of cellular and genetic approaches to brain development are possible, relatively few investigators are using interdisciplinary approaches to study the mechanisms through which activity on an altered hormonal milieu regulates the development of brain synapses and circuits. In addition, there are relatively few good normative data on the development of children’s brains (neuroimaging, emotional regulation, EEG asymmetry, sensory process event-related potentials) and even fewer that tie brain development to controlled studies of behavioral development. With the ability to use imaging in children comes the opportunity to study the development of a number of relevant aspects of cognition (e.g., attention, memory, affect regulation, and inhibitory control). These all have tie-ins, directly or indirectly, to behaviors or disease-based “misbehaviors.”
The slow progress in this area is highlighted by gaps in the current portfolio. For example, most work on activity-dependent brain development has been closely tied to the sensory periphery, whereas work on the epigenetic determinants of limbic system development has been relatively neglected. Even with work on the mature brain, studies correlating the performance of affect-associated tasks with electrophysiological recordings in awake behaving primates are exceptionally scarce. Yet, such work will be key to linking humans and tractable animal models. In addition, despite the great advances in mouse genetics, there has been relatively little development of behavioral tasks or neurological assays that help to decipher the circuit defects in these animals. There have been very few studies seeking to understand how the brain alters its normal development to adjust for these defects. Given all the activity in genetic linkage studies of human dysfunctions, whose goal is to find the genes responsible for dysfunction, it is exceptionally important to develop approaches using genetically altered mice to determine how brain development and behavior adjust to these primary lesions.
Recommendations for Basic Neuroscience Research
- We recommend that databases of rodent and human brain maps be established and supported. We particularly emphasize that these databases need to have a developmental dimension.
- We recommend that cross-Institute initiatives be fostered to establish genomic databases.
- We recommend funding program projects to bring together investigators from a variety of disciplines to examine the developmental effects of well-recognized conditions (e.g., stress and the HPA system).
- We recommend that technological and procedural advances should be supported that (a) allow scanning of very young normal children, (b) enable the development of noninvasive imaging that can be used on awake behaving primates, and (c) encourage the development of functional magnetic resonance imaging (MRI), which can image potentially powerful rodent models of genetic disease.
- Integrative approaches to studies of brain development and function are needed. Examples include (a) combining techniques of neuroimaging with simultaneous physiological monitoring and/or emotional testing, hormonal measurements, and so on; (b) electrophysiology at both the single-cell and multiunit levels to study molecular and circuit regulation in animals models of behavioral dysfunction; and (c) mutant animal models that allow researchers to study epigenetic determinants of brain development (e.g., constitutively manipulated mice may reveal compensatory developmental changes relevant to behavior).
- A major gap exists in the availability of data relating developmental trajectories across multiple levels of description, from genetic processes to behavioral competencies. Data are needed in the following areas:
- Cross-species differences and correspondences in neural and behavioral development, the impact of differing genetic backgrounds, and the validity of various phenotyping procedures in animals as behavioral markers of psychopathological outcomes.
- Gender differences and the putative actions of gonadal steroids, changes in neurocircuitry with puberty, and their relationship to cognitive, behavioral, and emotional regulation during adolescence.
2. Behavioral Science
Progress
Over the past 5 years, the NAMHC has developed two reports on basic behavioral science research. The first report, “Basic Behavioral Science Research for Mental Health” (NAMHC, 1995), highlighted past achievements and outlined the future trajectory of basic behavioral science within NIMH. The second report, “Translating Behavioral Science into Action” (NAMHC’s Behavioral Science Workgroup, 2000), focused on ways to enhance the potential contributions of behavioral science and how the critical insights offered by such research might be used to develop intervention and deployment research.
An extensive body of behavioral science research has identified the specificity and variability of basic behavioral processes in normal populations and has developed a range of methodologies and technologies for such research. Applying these sophisticated measurement technologies to clinical populations may lead to refined diagnosis and more precisely identified points of intervention. Illustrated here is research progress on normative processes that have implications for child and adolescent mental disorders.
Significant advances have been made in our understanding of the cognitive capacities of children, particularly those of infants and young children. For example, in mapping the structure of infant memory, very young infants’ memory capacities have been found to be independent of verbal ability and not to involve conscious awareness (Rovee-Collier, 1997). Further, the general organization of memory in young infants is the same as that in adults, where memory development primarily involves the acquisition of new information rather than an entirely new structure for organizing information. This work provides a foundation for designing new tests for developmental disorders that can be administered early in life when interventions are likely to be most effective.
An emerging body of evidence on the interrelation among temperament, mood, emotions, and cognition has implications for the etiology and course of illness. A good example of such research is the study of infant temperament, which is defined as the constitutionally based patterns of sociability, activity, physiological reactivity, emotionality, and self-regulation that can be identified very early in development. Temperament is influenced over time by heredity, maturational processes, and experience, and provides a substrate for individual personality. Basic knowledge on infant temperament has been augmented by research on how social and psychobiological substrates of affect may contribute to individual differences. For example, a number of projects in the current NIMH portfolio focus on measures of temperament and emotion and examine the links between them and early social factors, individual child characteristics, and physiological measures. Research examining the early development of attentional systems and how this development relates to the control of action and emotion has implications for improving the understanding of developmental problems in attention regulation. For example, studies are examining ways in which the executive attention network linked to frontal lobe development plays a role in the development of higher cognitive capacities and in the self-regulation of emotional states and action (Rothbart, MH43361). Because attentional self-regulation can contribute to behavioral problems and difficulties in school, research tracing the normal development of and individual differences in these controls has implications for advancing etiologic understanding of a variety of childhood disorders in which regulatory deficits are implicated (e.g., ADHD, mood and anxiety disorders). This work needs to be extended to include clinical populations, both to test the generalizability of the basic findings and to clarify how, and in which dimension, children with certain illnesses or symptoms express these regulatory functions in different ways. It will also increase the understanding of how behaviors, symptoms, and disabilities actually cluster across disorders.
Science Case in Point: Sleep Regulation and Pubertal Maturation
Studies of sleep/wake regulation exemplify the opportunities afforded by combining knowledge about biologic maturation (puberty), behavioral changes, and social influences such that the findings have implications for social policy. The fundamental issue is that many adolescents obtain insuffcient amounts of sleep at a time in development (pubertal maturation) when the biological need for sleep increases. Insufficient sleep can contribute to serious emotional and behavioral health consequences that include short-term as well as possible long-term effects. Progress in understanding the causes of sleep deprivation (and ultimately strategies for early intervention) has been informed significantly by research examining interactions between biologic systems, behavioral patterns, and social and cultural influences within a developmental perspective. Scientific progress includes these main points, made below:
At a time in development (pubertal maturation) when the physiological need for sleep increases, many adolescents are obtaining less sleep on school nights, largely as a result of late bedtimes combined with early school start times (Carskadon, 1999). The shift to later bedtime in early adolescence is, at least in part, related to maturational changes near puberty that cause a shift in the circadian system (biological clock) resulting in a biologically based tendency to stay up later and sleep in later (a shift from a more “lark” pattern to an “owl” pattern during pubertal development)(Carskadon et al., 1993). These biological tendencies (activated by pubertal maturation) interact strongly with behavioral/social factors in several important ways, including (1) less parental control over bedtime, (2) access to highly arousing stimuli (TV, movies, video games) and social interactions (telephone and Internet) late at night, (3) peer influences toward later bedtime, (4) access to stimulating substances (e.g., caffeine, nicotine), and (5) stress, anxiety, and worries that interfere with falling asleep. In combination, these factors lead to sleep-onset times that occur at late hours (Carskadon et al., 1993). Thus, the strong tendency for adolescents to adopt very late schedules (bedtime and wake time) results in a shift of the circadian system, which adapts more quickly to phase delays than to phase advances (thus it is very difficult for adolescents to shift back to the early bedtimes and rise times for school) (Carskadon, 1999). Despite an average bedtime between 11 p.m. and midnight, most high school students must wake up between 6 and 6:30 a.m. on school days. It is not infrequent for high school students to obtain less than 6 hours of sleep on school nights at a time in development when they typically require 8 to 9.5 hours of sleep per night (Carskadon, 1999). Individual differences in anxiety, biologic clock, sleep needs, and social context can greatly amplify the affective and behavioral consequences of insufficient sleep and erratic sleep/wake schedules (Dahl, 1999).
The short- and long-term consequences of insufficient sleep at this point in development are not fully understood. Preliminary data clearly indicate a negative impact on school performance and learning, as well as decrements in mood and self-regulatory abilities. More specifically, sleep deprivation is associated with irritability, poor concentration, and emotional lability, all of which create additional stress in the lives of many adolescents. Sleep deprivation can also increase stimulant use during the day (e.g., caffeine or nicotine), as well as extensive catch-up sleep on the weekends by sleeping in very late in the morning (which further interferes with the slowly adapting circadian systems, resulting in jet-lag like symptoms when the adolescent tries to shift back to an early wake-up time for school days). Sleep deprivation, mood disturbance, and impaired concentration and self-regulatory skills can spiral into more severe symptoms of impairment in school and social functioning, which further erodes mood (Dahl, 1999).
Some policy-level decisions are already being enacted to address aspects of these problems; one such policy is adopting later start times for high schools. Prelimary results from a controlled study of Minnesota school districts that have adopted later start times have been encouraging, with improved grades and mood ratings in the first year after these changes were made (Wahlstrom et al., 1999). Larger studies are currently in progress. Educational programs for adolescents are also being developed (similar to the nutrition education programs enacted in the past 20 years). However, large-scale policy changes and early clinical interventions focused on sleep and circadian aspects of adolescent health will require a great deal more interdisciplinary developmental research to better understand these complex issues.
Advances in the area of basic behavioral research involve our understanding of contextual influences on the development of personality or behavioral traits. Contextual issues play a critical role in the development, onset, and maintenance of mental illness in children. For example, studies have demonstrated that children with difficult temperaments may push the caregiver away, and with the caregiver less available, the child may develop soothing strategies that do not involve the caregiver. Nevertheless, mothers of such infants can be taught to effectively regulate the infant’s distress. Mothers who were trained to soothe their distress-prone infants and taught how to play with them were able to foster more positive affect and greater involvement of their children with them, with resulting benefits for their children in terms of attachment and sophistication of play (Van den Boom, 1994; 1995).
To better understand the social processes involved in mother-child transmission of affect, Fogel (Fogel, MH57669) is examining the development of emotion and attention in the context of a dyadic (mother-infant) relationship. Using a process design called relational-historical approach, this study is documenting the process by which individual differences in patterns of attention and emotion arise developmentally in infants’ social relationships with mothers. This study will include the observation of normally developing mother-infant dyads across key developmental transitions in the first 2 years of life, and also a larger group of dyads at risk for developmental disorders, who will then be followed longitudinally. One of the goals of this study is to understand the dynamic processes that regulate developmental change and the origins of individual differences in attention-emotion couplings. Such research is a step forward in exploring how the interaction of socialization and maturation of infants’ motor and cognitive abilities affects their ability to regulate their emotions.
Another example of the influence of contextual factors relates to the widely documented gender difference in depression, which begins to appear during adolescence. Biological as well as social and personality factors have been implicated. A recent, large-scale NIMH study simultaneously explored the social and personality differences that could account for the gender difference (Nolen-Hoeksema, Larson, & Grayson, 1999). Findings suggest that social factors (e.g., sexual abuse, lower income, inequities in distribution of work), child care, and personality factors (e.g., lower levels of mastery and a greater tendency to ruminate when depressed) were found to mediate the effects of gender. When these variables were controlled, gender difference in depression became minimal. These findings suggest that the increased incidence of depression among adolescent girls is likely due to factors that socialize them to be more emotionally expressive and to adopt internalizing coping strategies. Gender socialization processes prior to adolescence that may increase girls’ vulnerability to adolescent transitions (from elementary school to junior high) and thereby contribute to gender differences in depression have been identified. For example, girls are more likely to engage in self-evaluative mechanisms, which heighten vulnerability to depressive and anxiety symptoms. Further, mothers were found to exert greater control and decreased autonomy-granting over girls than boys (Pomerantz & Ruble, 1998). Social psychological theory suggests that this type of control is likely to undermine a sense of mastery and self-reliance that is crucial for coping with failures and disruptions, such as those experienced during school transitions. Such findings have implications for understanding the processes by which parental control influences girls’ perception of mastery and self-evaluation. Further, they have implications for developing interventions that could help decrease vulnerability to depressive symptoms.
Crossing the Boundaries
As previously noted, our understanding of the relative contributions of biological and environmental/contextual factors to the development of mental disorders is not complete. Recent expansion of knowledge in basic science, in conjunction with advances in behavioral science, can advance our etiologic understanding of mental illness, and hence have potential for prevention and treatment. We highlight below some of the opportunities for crossing the boundaries between behavioral science, basic neuroscience research, and intervention research.
Genetics and Behavior. The growing base of research on the genetic control of the developing brain structure and system, coupled with the ever-evolving, powerful technology that provides access to the developing brain, offers an unprecedented opportunity for understanding the etiology of mental disorders and, hence, ways to divert adverse developmental trajectories. The understanding of how these brain areas evolve as children’s cognitive abilities develop and transact with both genetic and epigenetic factors and influence the course of mental illness is an important research area. This area of research is complicated by the fact that mental disorders do not stem from errors in single genes. Furthermore, genes and the environment interact in complex ways over the developmental course of a mental illness. One vital task is to complete careful behavioral and biological descriptions of the behavioral phenotypes of specific subsets of mental disorders, including how they are expressed. Behavioral technologies from psychometrics and behavioral genetics are critical to the study of the sources of genetic and environmental variation and vital to dissecting and understanding the range of hypothesized phenotypes.
Managing Mental Illness. Because limited information is available about the short- and long-term safety and efficacy of psychoactive agents on the developing brain, the use of behavioral strategies is often the first line of intervention approach in the management of symptoms in children. Even when psychoactive agents are prescribed, there is evidence for including a behavioral component as part of the treatment protocol (MTA Cooperative Group, 1999a; 1999b). The examination of the long-term functional impact of such behavioral interventions is needed to further our understanding of disorder management.
Further, the impact of childhood-onset mental disorders has significant social implications for family members, as well as for school adjustment. The symptoms of mental disorders interfere with the development of social skills, and the social ostracization that is so often associated with mental illness further deprives children of precious opportunities to practice and develop needed skills to interact and cope with their social environment. Behavioral methods are needed that examine school-based interventions to help such children develop the requisite social skills for successful, if not non-traumatizing, peer relationships.
Brain Plasticity and Behavior. Adult behavioral treatment outcomes have found functional brain changes that are associated with positive behavioral outcomes (Baxter et al., 1992). For example, patients with OCD were found to demonstrate normalized position emission tomography in relevant brain regions after treatment with effective behavior modification. These changes were also associated with successful drug therapy (Schwartz et al., 1996). These findings have important implications for children and adolescents, in whom the tremendous malleability of the developing brain suggests even greater potential for identifying important behavioral time lines to target interventions and for understanding what level of intervention is needed to affect change and facilitate recovery.
Biobehavioral Development and Mental Disorders. Behavioral science offers a rich description of risk factors associated with the onset of mental disorders, and the behavioral course of some child mental disorders has been described (e.g., conduct disorder, autism, depression). Focusing on some well-defined areas of risk factor research may offer opportunities for translating this knowledge into developmental neuroscience research. An example of these opportunities is the risk factor research establishing that offspring of mothers who give birth earlier in life are more likely to exhibit externalizing behavior problems during childhood and adolescence (Hann & Borek, in press). Following early (prenatal through 30 months of age) in-home intervention programs, the mothers were found to be less impaired by substance use and less likely to neglect or abuse their offspring. In addition, the offspring of such young high-risk mothers had reduced rates of arrest, substance abuse, and number of sexual partners (Olds et al., 1986; Olds et al., 1997). It should be possible to use animal models to manipulate maternal age, fostering conditions (including cross-fostering condition with older mothers), maternal stress during pregnancy, and nicotine exposure to examine subsequent impulsivity, motor activity, and susceptibility to self-administration of drugs in their offspring. Variations in maternal care can also be examined. The use of transgenic and knockout mice to manipulate the genetic makeup of the animals would add a further refinement. It might be worth examining basal cortisol levels and various autonomic indices in these animals as well, given the associations observed in humans between these variables and disruptive and antisocial behaviors.
Obstacles and Gaps
Although efforts at translating behavioral science into action have been initiated through some collaborative work, the many research opportunities that intersect the areas of basic behavioral and intervention science are hampered by a lack of communication across disciplines, across levels of inquiry, across departments and schools, sometimes across NIMH organizational lines, and across researchers, providers, and consumers. Within the area of behavioral science, some of the specific challenges include the following:
- Developing scientifically valid and reliable measurements and methods. Traditional, category-focused diagnostic systems based on adult mental illness have not translated well for studying child disorders. There are few validated diagnostic categories in very young children. The threshold and boundaries for some disorders in children continue to be hotly debated (e.g., bipolar disorder). Further, the high degree of diagnostic overlap among disorders raises questions about nosology. Developing measurement systems that blend symptom-based indicators with process-based indicators would allow for a richer understanding of the individual child and his/her context, thereby allowing a better scientific understanding of the complex interplay of process and symptom and the development of finer-grained intervention approaches. This is particularly important in children, in whom diagnostic classification alone may be difficult or complicated and of limited use in developing or guiding interventions.
- Measuring function. Assessment of functioning has lagged considerably behind the assessment of clinical symptoms in mental illness. The serious economic and societal burden of childhood and adolescent mental illness requires the development of tools that can aid researchers, policymakers, and other mental health stakeholders in accurately assessing the form and frequency of functional impairments and projecting future health care needs and costs. Functional assessments are also particularly salient for children, as manifestations of symptoms are often complicated by the rapid developmental processes characteristic of childhood, and do not always fit into categorical classifications of mental disorders. Consequently, it is more useful and valid to study mental health and illness in children in terms of functional or adaptive abilities rather than solely relying on the traditional categorical approach, which has limited utility, especially in young children.
Theoretical perspectives and limited tools are available in the behavioral sciences for examining issues related to functioning, including peer influence, emotion regulation, cognition, and self-concept. Research in the area of functioning needs to take advantage of available resources by linking to behavioral theory and methods. For example, some research has documented specific cognitive and psychophysiological deficits associated with mental disorders (e.g., attention, information processing), but there is little understanding of how these deficits are related to specific functional problems or how such problems may be addressed by rehabilitative approaches. Consequently, many rehabilitative interventions are not grounded in research, and there is wide variation in how well these interventions help specific individuals with specific deficits. Some ongoing mental health research that focuses on or includes functioning is beginning to make these links, but most research to date does not.
- Contextual influences. There is some evidence that social, cultural, psychological, and market factors influence children’s vulnerability to risk, experience and reporting of symptoms, course of illness, the diagnostic process, access to quality care, responses to interventions, and health outcomes (Takeuchi, Uehara & Maramba, 1999; Vera, Alegria, Freeman, Robles, Pescosolido & Pena, 1998). The main and interactive effects of such context variables, individually and in combination, need to be identified and assessed to aid in designing and/or developing interventions appropriate to the needs and circumstances of children suffering from mental disorders and their families. Yet, these social and cultural contexts are not well configured into current paradigms of research. At the individual level, knowledge of how social and cultural contexts influence individual risk for mental illness and how such characteristics affect behavioral responses to intervention can inform the development and design of new interventions. Further, behavioral research can help identify strategies to better understand the role of providers as service ombudsmen for the child and family. Behavioral strategies are needed to help providers from different systems (e.g., schools, primary care) engage youth and families and to understand the factors that influence treatment acceptability. At the sociocultural level, knowledge of how ethnicity, culture, language, socioeconomic class, family and social networks, and neighborhood or community affect risk, diagnosis, and intervention is critical. At the organizational level, knowledge of how policies, incentive structures, and cultures at all levels of health/mental health organizations and institutions affect the behavior of those providing care and of those receiving it, including the outcomes of care, is needed. Given the country’s cultural diversity, a better understanding of how these contextual factors affect the mental health services system is needed. New approaches are needed to deliver culturally appropriate care to the disenfranchised and the destitute, for whom mainstream approaches are often too expensive, foreign, and centralized.
Recommendations for Behavioral Research
Current gaps in our knowledge highlight how basic behavioral science research is critical and can increase our understanding of risk, prevention, treatment, rehabilitation, and the organization, delivery, and use of mental health services. Below, research opportunities for linking basic research to clinical applications are listed:
- Research is needed on how different components of cognition (e.g., attention, language, memory, social) develop in normative and clinical groups of children in order to shape intervention and preventive strategies. This research can increase our understanding of how children with cognitive deficits associated with mental illness may benefit from intervention efforts and develop new or compensatory skills. Such studies have implications for the prevention or development of more severe impairments or comorbid conditions.
- We recommend detailed empirical study of the specific psychological and behavioral functions that are impaired in childhood mental disorders. Critical domains include memory, attention, emotional processing, emotional expression, social cognitive capacities, and several dimensions of child temperament. Specifying the nature of disorder in terms of these domains will not only improve nosology, but it will also be critical in making connections to neural substrates and in identifying genetic and experiential factors in etiology. As a result, such an effort will pave the way for the design and implementation of increasingly well-targeted modes of preventive and treatment intervention.
- We recommend research focused on developmental, behavioral, and social regulators of emotions at key transition periods, such as birth and puberty, and social transitions, such as daycare and elementary school.
- We recommend the development of science-based interventions that link the psycho-physiological deficits associated with mental disorders (e.g., attention, information processing) with specific functional problems, with the aim of formulating more effective and targeted intervention strategies.
- We recommend that NIMH support the development of measurements of functioning that are both culturally sensitive and multidimensional. New tools and approaches that combine qualitative and quantitative methods are needed to understand issues associated with children from diverse cultures and subcultures. In addition, measurements are needed that complement traditional symptom-based diagnostic systems and serve as outcome indicators in intervention, services, and risk processes research.
- We recommend developing measures and interventions through ethnography. The diagnostic conundrums that plague childhood nosology and the pervasive concern about labeling young children suggest that rigorous ethnographic or other qualitative methods for describing mental illness may be particularly useful in developing interventions that are sensitive to a variety of living environments, communities, and cultural contexts.
- We recommend new behavioral research to identify how providers and families manage children’s disorders and why they do or do not engage in the most effective practices. Behavioral science has significant promise to reveal why treatments are not more widely disseminated, what factors underlie complex health behaviors, and the types of decision-making strategies that guide current practice.
3. Prevention
Progress
Basic science for prevention is the study of both normal development and the development of psychopathology at the molecular, individual, community, and large-scale programmatic levels (i.e., State or Federal policy). Such study is critical to the development of preventive interventions. Preventive interventions offer opportunities to test fundamental mechanisms about either the causation of the disease or, alternatively, the avoidance of poor outcomes in the face of risk. One fundamental test of whether a mechanism is truly understood is whether preventive interventions can alter the expression of disorder.
While prevention has not historically been regarded as an essential part of research, particularly within mental health, three recent developments have substantially changed that perspective. First, there are now a number of longitudinal and developmental investigations that provide vital information about development and, in particular, the identification of sensitive periods, the balance between risk and protective factors, and vulnerabilities (both genetic and environmental). Findings from these studies provide the necessary scientific basis from which to mount preventive intervention efforts. Second, preventive intervention investigations are somewhat more difficult than cross-sectional analyses, or even short-term randomized trials, because they require the demonstration that effects are sustained over several years. Recently, both methodological designs and statistical analytic techniques have been devised to provide the conceptual bases for designing and evaluating prevention programs. Third, a number of prevention trials have proved successful, either significantly reducing risk factors for disorders or changing the course of the illness in its early state. As for clinical treatment studies, the next frontier is the testing of prevention designs in effectiveness trials. Some preventive intervention strategies, such as nurse home-visitation programs and multisystemic family therapy, are already in the effectiveness testing stage, while others, such as prevention interventions for depression, are in the efficacy testing stage.
The subject of prevention research has been reviewed in several major reports. In 1996, “A Plan for Prevention Research for the National Institute of Mental Health” (NIMH Advisory Mental Health Council Prevention Research Steering Committee and the Institute of Medicine Committee on Prevention of Mental Disorders, 1996) summarized two previous reports: “The Prevention of Mental Disorders: A National Research Agenda” (NIMH Advisory Mental Health Council Prevention Research Steering Committee, 1993) and “Reducing the Risks for Mental Disorders: Frontiers for Preventive Intervention Research” (Mrazek & Haggerty, 1994). In 1998, “Priorities for Prevention Research at National Institute of Mental Health” (National Advisory Mental Health Council Workgroup on Mental Disorders Prevention Research, 1998) was developed to review the NIMH research portfolio on the prevention of mental disorders, identify research gaps and opportunities, and indicate priorities for future research. The commonalities among these reports were recognized, and there was a strong endorsement of the need for (1) continued exploration of the interface between potentially modifiable biological and psychosocial risk and protective factors, (2) outcome-prevention research focused on risk reduction, and (3) broader collaboration among scientific disciplines and the dissemination of existing approaches.
Crossing the Boundaries
The most recent report on prevention research, “Priorities for Prevention Research” (NAMHC Workgroup on Mental Disorders Prevention Research, 1998), recommended several steps to advance the science of prevention research. The report recommended broadening the definition of prevention factors to focus more fully on basic biological, psychosocial, and social-cultural risk factors. The report also suggested that the prevention of relapse, co-occurring illnesses, disability, and the consequences of severe mental illness be considered within the prevention rubric. Further, the report emphasized the critical importance of integrating knowledge across disciplines, as well as integrating prevention research across all phases of research, including preintervention, intervention, and services research.
Opportunities for integrating prevention research into intervention research are delineated by Pearson and Koretz (in press). First, prevention trial designs can offer strategies for treatment research design. Prevention trials are embedded in defined populations (Kellam, Koretz, & Moscicki, 1999) and allow for the analysis of mediators and moderators of the effects of intervention (e.g., recruitment, retention, level of intervention received). As treatment research moves toward a public health model with greater emphasis on effectiveness, service delivery, and dissemination, the use of epidemiologically based trial designs, in which target populations are defined on the basis of samples representative of the populations seeking treatment or services, will be critical. Such designs will allow less biased ways to understand challenging treatment research issues, such as treatment refusal, dropout, and relapse.
Second, sophisticated analytic models have been developed to deal with longitudinal data in prevention research, which allow for multiple assessments across time, taking into account baseline trajectories (Brown & Liao, 1999; Curran & Muthen, 1999). These analytic models will be particularly useful to child intervention researchers who are interested in understanding the long-term effects of intervention in the context of developmental processes and their impact on the course of the disorder. Further, epidemiologically-based samples have the advantage of avoiding referral biases inherent in most traditional clinical trials. Such analytic models have also delineated approaches to delivering interventions to appropriate individuals in a “unified” manner so that multiple components of certain interventions could either be staged sequentially or delivered simultaneously (Brown & Liao, 1999).
Third, prevention trials embedded in existing communities and institutions (e.g., school-based prevention efforts) can offer insights into approaches for collaborating with various systems (e.g., Harachi et al., 1996). Such collaborative relationships are essential if intervention researchers are to develop effective treatments that can ultimately be transported, used, and sustained in communities. Such prevention trials require collaboration among community representatives and researchers to identify common goals, and are typically based on multilevel intervention strategies that have been shown to be effective for early, proximal risk factors (e.g., intervention with first graders [Ialongo et al., 1999]) and difficult-to-treat populations (e.g., juvenile delinquents [Henggeler et al., 1996; 1999]). Such multilevel approaches can be useful as treatment research moves beyond interventions for targeting single disorders and considers combined treatments and services to address more heterogeneous groups of children.
Fourth, in addition to categorizing prevention efforts according to levels of risk (universal, selected, and indicated [Gordon, 1983; 1987]), recent recommendations to broaden prevention efforts to include comorbidity, disability (primary, secondary, and tertiary prevention), and relapse prevention (NAMHC Workgroup on Mental Disorders Prevention Research, 1998) have implications for future treatment intervention efforts. Such efforts include research to understand how to reduce the incidence of co-occurring psychiatric disorders (e.g., depression with anxiety) or psychiatric conditions with medical disorders (e.g., depression with asthma), decrease the onset of more severe impairments or disorders (e.g., conduct disorder with ADHD), and reduce relapse of future episodes (e.g., depression) through appropriate management of stress or adverse experiences.
Ultimately, preventive intervention trials offer one of the best scientific tests for understanding the mechanisms of causation of disease or the emergence into health. The recognition and examination of multiple influences on developmental plasticity is key for future scientific advances in the study of preventive interventions for children.
Obstacles and Gaps
To date, prevention programs, for the most part, have focused on efficacy studies, and each addresses a specific developmental epoch, with little continuity across the life span. Current strategies tend to focus on individual-level processes, rather than on the broader context of school, family, and community. There is a need for population-based cohort studies, studies of high-risk individuals, and studies of high-risk families. The NIMH research portfolio must be realigned to reflect the public health significance of the disorders targeted, with an emphasis on different cultural perspectives and a focus on the differing ways individuals from diverse backgrounds respond to similar stressors.
Limited attention has been devoted to effectiveness studies, with little attempt to coordinate different researchers working on the same problem, such as the prevention of depression. Specifically, there is a lack of preventive services research. Gaps include a lack of focus on the prevention of anxiety and depression across the life span, opportunities for the prevention of ADHD, and new approaches to prevention intervention research. One critical research area includes broadening disorders in populations targeted for prevention research, with a greater focus on comorbidity and developing a preventive services research program.
Prevention research trials, by their nature, require longitudinal follow-up and fairly sophisticated effects from interventions. The translation of this sophisticated methodology used in efficacy studies to large effectiveness trials and programmatic efforts has yet to take place. Furthermore, historically, those who have focused on severe mental illness in adults have tended not to focus on early-life interventions that may, in general, increase the resources and readiness of a child and family to cope with whatever comes, but that are not directly linked to later outcomes. This is partially because those doing early interventions have not looked primarily at mental health outcomes. The need must be recognized for intervention programs across the life span—not just for support in the few years before the onset of major mental illness in early adulthood.
The translation from efficacy to effectiveness is not an easy one. As one example, there is new evidence from the work of David Olds and colleagues (1999) that nurse home visitation delivered in the first 2 years of an infant’s life to a first-time adolescent mother can make quite a significant difference, even 15 years later, in terms of health outcomes for the infant and mother (see Science Case in Point). However, there are also many nurse home-visitation programs that do not yield similar results. In fact, after Olds’ initial research in Elmira, New York, there was an attempt to replicate the program using paraprofessionals. The results were less dramatic (Olds et al., 1999). This finding emphasizes the fact that mental health outcomes such as substance abuse or physical abuse of children can, in fact, be affected by interventions early in life when they are delivered with attention to the fidelity of the implementation. It also emphasizes that the translation to large effectiveness trials is a difficult and arduous task that requires sustained programmatic focus and support if prevention research is ultimately to have an impact on public health. As illustrated later in the case study on childhood-onset depression (appendix B), the recent efficacy data about the prevention of depression, although modest in scope, offer considerable promise. Little work has been done to provide models about how to take such programs to scale, particularly with awareness of cultural and community influences.
To return to the fundamental scientific principle: Prevention trials offer one of the best ways of testing the mechanisms of action in moving toward either psychopathology or health, so prevention research is a legitimate and necessary part of any fundamental, longitudinal, developmental, child-based, scientific investigation.
Recommendations for Prevention Research
- We recommend that attention be paid to smaller, focused, and intensive longitudinal studies, informed by basic research.
- Given the extensive number of data sets examining risk and protective factors, we recommend that a workshop be convened to identify opportunities for reanalysis of existing data sets. Examples of questions for such studies would include areas of attributable risk, predictors of resilience, interaction of different types/levels of risks across time, how impairment is affected by context, and the impact of contextual and cultural variables on functioning over time.
- A new emphasis is needed on prevention effectiveness trials, prevention services, and cost-effectiveness of preventive strategies. Studies that focus on service contexts that facilitate or impede the sustainability of preventive interventions are especially needed.
- Prevention research trials, by their nature, require longitudinal follow-up and the use of fairly sophisticated efforts to determine the effects of the interventions. Support for methodology development, especially the analysis of longitudinal data where the phenomena wax and wane, is needed via program announcements or conferences.
- Research on relapse prevention, desistance, and naturally occurring prevention is greatly needed.
4. Psychosocial Interventions
Progress
Reviews of the past 25 years of clinical trials of child psychosocial interventions have consistently pointed to beneficial effects of treatment over no treatment (Casey & Berman, 1985; Kazdin et al., 1990; Weisz et al., 1987; 1995). Further, the effects of these treatments are quite strong and comparable to those found in adult psychotherapy (Lambert & Bergin, 1994; Smith & Glass, 1977). Outcome studies continue to emerge, with ongoing improvements in the quality of design and method (Durlak et al., 1995). In the past decade alone, an estimated 500 controlled treatment outcome studies of psychotherapy for children and adolescents have been conducted (Kazdin, 2000a). Recent reviews of psychosocial interventions have been published, with some efforts made to identify specific empirically supported psychosocial interventions for children (Burns, Hoagwood, & Mrazek, 1999; Journal of Clinical Child Psychology, 1998; Weisz & Jensen, 1999). Criteria for assessing what constitutes an evidence base have been offered. Kazdin (1999, 2000a) described critical domains that constitute such criteria: A theory to relate a hypothesized mechanism to the clinical problem, basic research to assess the validity of the mechanisms, preliminary outcome evidence to demonstrate that a therapeutic approach changes the relevant outcomes, and process-outcome connections that display the relationships between process change and clinical outcomes.
Guidelines for clinical practice have been developed to take into account this body of empirical evidence (American Academy of Child and Adolescent Psychiatry, 1998). More specific operational criteria have been proposed by a task force of the American Psychological Association (APA) to identify well-established and probably efficacious treatments (Lonigan, Elbert, & Johnson, 1998). The criteria for “well-established” therapies require at least two scientifically defensible group-design studies conducted by different investigative teams, or more than nine single-case design studies, treatment manuals,1 and strong experimental designs. Therapies designated as “probably efficacious” generally require at least two studies demonstrating the intervention to be more effective than a no-treatment control group, or several single-case design studies demonstrating their impact, as well as manuals that prescribe therapy.
Efforts to distinguish what does and does not work are very important, as treatments vary in their level of efficacy, may be ineffective, or, worse yet, may be harmful. Through such efforts, approximately two dozen specific treatments have been identified as efficacious for various conditions in children, including ADHD, anxiety disorders, oppositional-defiant disorder, conduct disorder, and depression (Chambless et al., 1998; Lonigan, Elbert, & Johnson, 1998). Some examples of these treatments include reinforced practice and participant modeling for fears and phobias; behavioral parent training and classroom behavior modification for ADHD; cognitive behavioral therapy for anxiety and depression; interpersonal therapy for depression; and anger-control training, problem-solving skills training, multisystemic therapy, delinquency prevention, and parent-child interaction treatment for conduct problems.
Science Case in Point: Preventive Intervention Nurse Home-Visitation Models
The theoretical model of David Olds’ nurse home-visitation program exemplifies a comprehensive approach to intervening with high-risk families to prevent negative consequences to infants. This program, grounded in epidemiology and theories of child development and behavioral change, emphasizes the importance of (1) reducing children’s neurodevelopmental impairment (including emotion and behavioral dysregulation and cognitive impairment) through the improvement of prenatal health-related behaviors, (2) reducing the dysfunctional care of the child, which compromises health and development, and (3) increasing the economic self-sufficiency of the parents by helping them plan future pregnancies, find work, and eventually, decrease reliance on welfare. The development and testing of this model was further complemented by a cumulative sequence of field trials, with replication of findings in diverse populations, and current efforts to scale up the program across the country.
During a home visitation, nurses make an effort to help mothers and other family members improve their health behaviors and the care of the child and enrich the parent’s personal development. They provide child development information, parenting education, parental social support, parent leadership training, screening, and referrals for a period of 30 months. Evidence for standardization of treatment includes detailed record-keeping forms, visit-by-visit protocols, case reviews, and extensive staff training. Essentially the same program (refined over the years) was tested in three sites to ascertain the generalizability of findings: a small semirural county in Elmira, New York (n=400), and two urban areas serving minority families in Memphis, Tennessee (n=1138) and Denver, Colorado (n=735), where the trial is still underway. This program of research is characterized by strong sample retention and measurement of outcomes; many outcomes were collected on institutionally archived data, such as medical, criminal, Aid to Families with Dependent Children program (now called the Temporary Assistance to Needy Families program), and child abuse records. Multiple informants of child behavior problems (parent and teacher) were used at older ages, although these sources did not always corroborate the findings of reductions in child-reported arrests at 15 years with corresponding reductions in delinquent acts.
Results have been published from the Elmira and Memphis trials (Olds et al., 1999). In both trials, families received a little over 50 percent of the scheduled visits. Evaluation results have been reported most fully from the Elmira site. As with many preventive interventions, the outcomes of this study were not limited to the risks for mental health or behavioral outcomes examined in this review. Researchers found reduced incidences of child abuse and neglect in the intervention vs. the control group when the children were 2 and 15 years of age (Olds et al., 1986; Olds et al., 1997). When children were 15 years of age, mothers in the intervention group were also reported to be less impaired by drug and alcohol use over the 15-year period following the birth of the first child compared with mothers in the control group (Olds et al., 1997). Moreover, the 15-year-old children had over 50 percent fewer arrests, 69 percent fewer convictions for the original crime or probation violations, 28 percent less use of cigarettes, 56 percent less use of alcohol, and 63 percent fewer sexual partners (Olds et al., 1998). Many corroborating effects were found in related aspects of maternal and child functioning. Many of the early beneficial effects found in Elmira were reproduced in the Memphis replication, although the treatment versus control differences generally were not as large as those in Elmira. Based on the two completed trials, this program was found to benefit the neediest families (low-income, unmarried women), with little benefit for the broader population (Olds et al., 1999).
Economic analyses by the RAND Corporation (Karoly et al., 1998) have shown that the investment in the service is recovered with dividends by the fourth year of the child’s life when it is focused on low-income families (Olds et al., 1993), with an estimated four dollars saved for every dollar invested (Karoly et al., 1998). Based on the high-quality study design and program implementation, positive short- and long-term effects and replication, this intervention is deemed appropriate for dissemination. The program is currently being replicated in nonresearch settings, and evaluations are being conducted to determine the extent to which the program is being conducted with fidelity to the model tested in the randomized trials.
In the past 5 years, there has been a concerted effort by the clinical treatment research field to move beyond small-scale efficacy trials to broader-based effectiveness studies (Hoagwood, Jensen, Petti, & Burns, 1996). This emphasis on the translation from efficacy to effectiveness has resulted in an increase in studies that focus on more heterogeneous populations, more “real-world” settings (e.g., pediatricians’ offices), and a wider range of outcomes with which to investigate the applicability of the treatment under consideration. Further, effectiveness studies are increasingly attending to the use of treatment manuals to codify procedures (Kazdin, 2000b), issues of treatment fidelity (e.g., Schoenwald, Brown & Henggeler, 2000c), and assessment and maintenance of therapeutic change (e.g., through an after-care program that monitors children and families and provides periodic treatment sessions, as needed, to maintain treatment gains, prevent relapse, and reduce the need for and use of additional services following treatment (Kazdin, MH59029). Some efforts are also underway to adapt, develop, and test treatment approaches with specific cultural groups (e.g., Rossello & Bernal, 1999).
More recent efforts at NIMH to encourage an expanded treatment research agenda with a public health focus have cautioned against the dichotomy between efficacy and effectivenesstreatment designs. In efforts to broaden the scope of clinical research studies, the terms efficacy and effectiveness have become buzzwords, resulting in inconsistent use of terminology. As a result, effectiveness research may mean many different things. Rather than focusing on the strengths and weaknesses of each type of design, the next frontier of treatment research calls for new and innovative methods, including mixed-modality approaches (e.g., combined treatments—see Section B.6. Combined Interventions and Services Effectiveness), paradigms that include both experimental and observational work, and hybrid treatment study designs that combine the careful controls of efficacy trials and the flexibility of effectiveness paradigms (Miklowitz & Clarkin, 1999; Norquist, Lebowitz, & Hyman, 1999).
The significant progress in this area indicates that clinical psychosocial treatments have much to offer. They offer the prospect of enhancing the quality of children’s development and reducing the risk for short- and long-term impairment. They also offer the potential to provide alternatives or complements to pharmacological interventions that parents and children may view more positively. In a related vein, psychosocial interventions may also enhance the impact of pharmacological treatment. As interdisciplinary research in child mental health progresses, documented brain changes that occur in children in response to psychosocial interventions may inform our understanding of underlying neurobiological mechanisms and biobehavioral processes.
Crossing the Boundaries
If the impressive advances in child and adolescent psychosocial treatment research are to be effectively applied and used in service settings, such progress must be accompanied by a systematic plan to guide treatment development, future progress, and evaluation. The question of “what treatment, by whom, is most effective for this individual with that specific problem, under which set of circumstances” may not be applicable owing to the number of therapeutic techniques under use, the number of child disorders, and the wide range of factors that can influence treatment outcome—all of which may vary depending on when treatment is applied in the course of development (Kazdin, 2000a). To make significant advances in the field of child and adolescent psychosocial research, Kazdin (2000a) proposed a research plan that is consistent with the goals of this report. Broadly, this plan emphasizes the need to (1) connect treatment development with what we know from basic science (including developmental psychopathology), (2) understand the mechanisms or processes by which therapeutic change occurs and factors that influence the change, (3) broaden the range of questions (beyond treatment techniques and global conceptual approaches), and (4) expand the range of outcome criteria to evaluate treatment effectiveness (including differential outcomes by subtypes that may or may not be linked to DSM diagnoses). Weisz (2000) further argued for the need to move beyond serial efficacy studies to achieve this research agenda. To ensure that research for treatments will be used in clinical practice, Weisz proposed a Clinic-based Treatment Development Model in which the development and testing of treatments are moved at an early stage into clinical practice to ensure a more complete understanding of the processes and mechanisms of therapeutic change.
These conceptual contributions are critical; this report highlights the urgent need for these and other critical linkages to be made in order to focus the field of child and adolescent mental health intervention research. To date, most psychosocial interventions developed have largely ignored the tremendous amount of knowledge in basic science. For example, a recent review of the NIMH portfolio on ADHD revealed that literature on the development of executive functions and regulation of attention and impulse control exists within the basic science. Yet virtually none of this research has been connected to the development of interventions for children diagnosed with ADHD. With some exceptions, most current treatment paradigms (e.g., cognitive behavioral therapy [CBT]) for children have been modeled after adult studies, with limited attention to developmental or contextual issues or solid theoretical conceptualization of the disorder based on developmental psychopathology, basic neuroscience, or behavioral science theory. The rapidly evolving knowledge from basic science should be harnessed more systematically to guide intervention development. Yet etiologic understanding does not guarantee an effective treatment (Kazdin, 2000a). While basic research continues to increase understanding of etiologies that can guide treatment development, effective treatments can be identified. Such treatment outcome studies can, in turn, inform basic research. The knowledge of the processes and mechanisms by which such treatments lead to therapeutic change can help basic researchers identify potential variables that may be involved in the etiology, maintenance, and recurrence of child and adolescent disorders.
Another critical linkage involves harnessing knowledge from the services and dissemination research areas (see this report, Section II.B., 6. and 7.). Services and dissemination research offers crucial information on the factors critical to successful transportation of interventions—information that can be integrated into treatment development, right from the start, to ensure that interventions can be used and sustained. At the same time, psychosocial intervention outcome studies can also inform services and dissemination research by providing clues about the facets of treatments that are critical to ensure beneficial outcomes, delineating the conditions and parameters under which interventions are most likely to succeed and identifying the processes and principles by which treatments may be augmented to enhance their success across diverse populations and settings.
Obstacles and Gaps
Despite the sheer quantity of studies in psychosocial outcome research for children and adolescents, the direction of research in this area has been criticized for a neglect of theory, a lack of distinction between theories of onset of dysfunction and therapeutic change, and the lack of progression of knowledge from description to explanation and from risk factors to causal agents (Kazdin, 1999). Although some empirically supported treatments can be shown to reliably produce change, the processes by which such change occurs are not well understood. The complex relations among multiple, dynamic, and (often) confounding influences and clinical outcomes pose significant conceptual challenges for understanding the nature of clinical disorders and therapeutic change. These challenges are further complicated by constraints of current statistical models, which limit assessments of these complex relationships (e.g., assessing multiple constructs at multiple levels at multiple points across the developmental trajectory).
Another challenge in psychosocial intervention research relates to the development of interventions that are generalizable. With a few exceptions, the majority of treatment development research has been focused on single, specific disorders and tested on nonclinically referred children. The applicability of scientifically proven treatments to diverse populations and settings is frequently challenged. At the same time, a meta-analysis summarizing the limited literature on treatment effects in clinical practice (as opposed to research settings) found almost no difference between treatment and no-treatment conditions (Weisz et al., 1995). Thus, whether conclusions drawn from treatment research developed in research settings can be applied to clinical practice remains an open question (Weisz, Weiss, & Donenberg, 1992).
As noted earlier, task forces have been brought together by different professional associations and private foundations to develop guidelines and criteria for evidence-based interventions. Despite increased attention to empirically supported treatments, there is not yet clear consensus about what constitutes evidence-based treatments. For example, the thoughtful criteria developed by the APA task force have not been widely adopted, in part because of several limitations. The criteria were based on multiple subjective judgments, and there was no common outcome metric across the studies (Weisz & Hawley, 1998). In addition, many such studies fail to describe effects adequately. Positive results are typically described as significant differences between groups, between pre- and post-tests, or by magnitude of effect. The level to which interventions raise functioning in relation to “normal” or “typical” children is often not known or described. Further, the majority of the interventions identified by the task force as having demonstrated efficacy consist of brief behavioral or cognitive behavioral interventions for specific disorders. This is in marked contrast to the theoretical orientation of many clinicians. The focus of psychosocial intervention research on “pure” forms of intervention is in striking contrast to most clinical practice, where intervention approaches often emphasize processes with wide applicability across disorders rather than specific dysfunctions (e.g., maladaptive family processes and distorted cognitions) and techniques that are eclectic or multimodal in nature (Kazdin, 2000a). The use of treatment manuals that rigidly fix treatments is seldom directly applicable to the problems presented by clinically referred children, who often have more severe, chronic, and comorbid conditions, and who come from less advantageous environments.
The disconnect between treatment research and clinical practice is related to several issues. Treatment research for children has typically involved conducting such studies within controlled and somewhat rarefied environments, such as university laboratories. Studies of conventional treatments delivered in clinics and clinical programs have demonstrated much weaker effects (Weisz et al., 1995). There has been an implicit assumption that once the laboratory studies of the efficacy of treatments have been completed, the results will be usable and relevant outside of these laboratories. But as Weisz and colleagues have noted (Kazdin & Weisz, 1998; Weisz, 2000; Weisz et al., 1993), there are numerous differences between the conditions of most research settings and the conditions in which everyday treatment is delivered. These differences may mean that treatments developed through efficacy trials may need adaptation to fit into many clinics and other service settings. The challenge of addressing the discrepancy between treatments as tested within controlled environments and treatments or services as tested within real-world clinics or community settings has been identified as a major impediment to closing the gap between science and practice (Burns, 1999; Burns, Hoagwood, & Mrazek, 1999; Hoagwood, Hibbs, Brent, & Jensen, 1995; Jensen, Hoagwood, & Petti, 1996; Jensen, Hoagwood, & Trickett, 1999; Kazdin & Weisz, 1998; Weisz et al., 1993). Understanding the mechanisms by which these empirically supported treatments lead to beneficial outcomes, as well as the factors that moderate treatment outcomes, will be critical to increasing their transportability.
Finally, barriers to the use of evidence-based interventions have not been adequately considered in intervention development. For example, economic factors and their feasibility (e.g., treatment cost, training cost, and reimbursement) are often not taken into account in intervention development research. Yet, if providers are not trained or reimbursed for evidence-based treatments, those treatments will not be practiced.
Similarly, if families are unable to accept a certain type of treatment, outcomes will not be successful. In the current health care climate of cost containment, identifying core elements of interventions that potentiate the outcomes of interest is important so that buyers of services can make informed choices to improve triage and increase the efficiency of services. Studies are needed to answer, for example, questions about those components of cognitive-behavior therapies, family therapies, home-visitation programs, or parent management programs that are core to obtaining certain outcomes. Studies are needed that deconstruct or dismantle therapies into elements that eventuate certain positive outcomes and that are practically amenable to being taught to mental health care providers, including teachers, health care paraprofessionals, and others in the field.
Recommendations for Psychosocial Interventions
- We strongly urge that treatment studies move beyond assessing outcomes to focus more attention on the mechanisms or processes that influence those outcomes. These mechanisms may involve basic processes at different levels (e.g., level of neurotransmitters or stress hormones, information processing, learning, motivation, therapeutic alliance) and may be mediated by therapeutic approaches (e.g., practicing new behaviors, habituating to external events). Understanding the mediators and moderators of outcomes will be important in identifying the ingredients required for therapeutic change.
- We further recommend that treatment outcome studies assess outcomes beyond child symptom reduction to include functioning across various domains (e.g., school functioning, social interactions, family interactions, adaptive cognitions) to provide a more comprehensive picture of the benefits of psychosocial interventions.
- We recommend that NIMH promote a scientific agenda on the generalizability of psychosocial treatments by targeting funds toward the development or adaptation of psychosocial treatments that are implementable in real-world settings (e.g., schools and primary care), including the transportability of treatments with minority populations. Attention to the impact of development, culture, and context on the effectiveness of psychosocial treatments must be a priority. Such efforts will require the development of new methodologies to address the issue of increased heterogeneity in effectiveness trials, treatment fidelity (flexible vs. rigid adherence to treatment protocols), a clear definition of “treatment as usual,” and the use of appropriate comparison groups.
- We recommend that the psychosocial treatment program target the critical research gaps listed below:
- Comorbidity (e.g., substance abuse and depression, anxiety and depression, medical and psychiatric disorders)
- Potentially life-threatening conditions (e.g., eating disorders, suicide), bipolar disorders, anxiety spectrum disorders, autism, neglect, physical and sexual abuse, early-onset schizophrenia
- Gateway conditions of disorders (e.g., oppositional defiant disorder [ODD] as a gateway to conduct disorders, trauma as a gateway to post-traumatic stress disorder [PTSD], or ADHD as a gateway to ODD/conduct disorder/substance use) to divert onset of more serious disorders or impairments
- Parental mental illness and its influence on the prevention and treatment of child and adolescent mental disorders
- We recommend that priority be given to treatment modalities beyond cognitive behavioral therapy and behavior therapy (e.g., family therapy, Internet-based interventions), studies comparing psychosocial interventions for the same conditions (e.g., comparing combined treatment involving parent training and parent-child relationship therapy vs. child-focused interventions), and studies that address the issue of sequential psychosocial treatments and/or combined psychosocial and psychopharmacology treatments.
- We recommend that NIMH give funding priority to studies of common treatments and services available in the community (e.g., wraparound, treatment foster care, residential care, hospitalization), as they may provide a promising avenue for discoveries of new treatment approaches or strategies.
- Because so few studies have assessed the long-term outcomes of interventions (beyond 5 years), and because assessments of the cost-effectiveness as well as clinical and functional outcomes are needed to determine the benefits of treatment and impact on course of illness, we recommend that NIMH encourage long-term follow-up studies of treated and untreated populations.
5. Psychopharmacology
Progress
As in other areas of child research, the changes in clinical practice in child and adolescent psychiatry have far outpaced the emergence of research data. Compared with those for adults, relatively few psychotropic drugs have been approved specifically for the treatment of pediatric childhood disorders. The small number of approved indications in pediatric psychopharmacology is problematic because clinical decisions are not guided by a scientific knowledge base for the majority of childhood psychiatric disturbances and symptoms.
Since the early 1990’s, substantial progress has been made in conducting high-quality scientific studies on the role and benefits of medications for the treatment of childhood mental disorders. Consequently, a sizable scientific evidence base is becoming available to help providers and parents make informed choices about medication treatment options, whether such medicines are used alone or combined with psychotherapies. One major advance is the newfound appreciation that children can suffer from psychiatric disorders and that some of these disorders can be reliably diagnosed in children. The difference lies in the diagnostic process, in which multiple informants are required. While more work is still required to increase the reliability of assessment instruments for certain syndromes, the field is sufficiently advanced that clinical trials have been launched. Advances in medication treatments are especially promising for several disorders, including ADHD, OCD, and childhood anxiety disorders. In addition, major studies are currently underway to test the benefits of psychotherapeutic, medication, and combined treatments for ADHD in preschoolers, major depression in adolescents, and OCD. Similar sizable trials and substantial efforts are also being conducted in the areas of youth bipolar disorder, autism, and other major mental disorders affecting youth.
Federal and Industry Developments
Two recent initiatives, the 1997 Food and Drug Administration Modernization Act (FDAMA) and the 1998 Pediatric Rule, have been particularly important in stimulating greater interest in developing psychopharmacology for children and adolescents. The FDAMA gives the FDA authority to require that certain studies be done in children for both new drug applications and already-approved drugs that companies plan to develop for new indications in adults. FDAMA is a voluntary program that gives a financial incentive (an additional 6 months of patent exclusivity) for companies to study both new and currently marketed drugs in children. Under FDAMA, nine written requests have been issued for three psychiatric disorders in pediatric patients—major depressive disorder, OCD, and generalized anxiety disorder. Under the Pediatric Rule, studies have been requested for PTSD, social anxiety disorder, mania, and premenstrual dysphoric disorder. Other conditions that are currently under consideration for issuing written requests and requiring studies under the Pediatric Rule include schizophrenia, panic disorder, conduct disorder, and ADHD (for children under 6 years of age) (Laughren, 2000).
The increased research activity in child and adolescent populations by the pharmaceutical industry can be further enhanced in several ways. Dissemination of study data in peer-reviewed journals is not always a priority in these studies. Therefore, valuable information is not always shared with the scientific community and providers. Prompt dissemination of study results, even negative studies, should be encouraged. Improved cooperation among investigators, clinicians, parents, patients, and government agencies (scientific and regulatory) may allow for large studies to have more “depth” than simply safety and efficacy.
Methodological Advances
Drug Metabolism Studies. Until recently, very few drug metabolism studies were performed in children. There is a growing appreciation that dose-ranging, pharmacokinetic studies can be effectively implemented to develop rational medication dosing strategies for children. Single-dose studies do not examine with adequate rigor how medications are processed in the body. Consequently, investigators are examining drug metabolism to dose psychotropic agents in children more accurately and safely. Further research is needed into the determinants of clinical response (pharmacodynamics), tolerability, and between-patient variability in optimal dose levels.
Protocol Development. Some “standard” protocols to test the efficacy of psychotropic drugs over the short term have been developed for a few disorders, including ADHD, depression, and OCD. In addition, the Research Units on Pediatric Psychopharmacology (RUPP) centers have implemented methods for the study of anxiety and autistic disorders. Currently, accepted protocols do not exist for bipolar disorder, schizophrenia, PTSD, and certain other conditions. With the exception of the MTA study, consensus about effectiveness studies needs to be developed. Long-term safety studies tracking large cohorts of patients should be a priority, considering the number of children and adolescents receiving psychotropic medications and the chronic, recurrent, and disabling nature of many psychiatric disorders. In addition, studies of comorbid disorders and combination pharmacotherapy are needed in light of the number of children receiving concomitant medication treatments.
Advances by Condition
Much is now known about how to treat many of the mental illnesses that befall children and adolescents. Of all of the childhood-onset psychiatric disorders, ADHD is the most widely studied, with a plethora of literature on the short-term effects of medications on ADHD now available. Recently, results were released from the MTA study, an effectiveness trial that considered the roles of state-of-the-art pharmacotherapy, psychosocial interventions, and their combination (MTA Cooperative Group, 1999a, 1999b; see also Science Case in Point). Currently, a six-site NIMH study (Preschoolers with ADHD Treatment Study [PATS]) is assessing the safety and efficacy of methylphenidate in young children.
Despite the high prevalence and frequency of their use, no antidepressants are currently labeled for use in childhood depressive disorders. Several efficacy and safety studies are now underway. An NIMH-funded study (Treatment of Resistant Depression in Adolescents [TORDIA]) will test the effects of pharmacological and combined pharmacological and psychotherapeutic treatment strategies for adolescents who have failed to respond to an adequate course of selective serotonin reuptake inhibitors (SSRI’s). The TORDIA study should help determine the utility of psychotherapy and pharmacotherapy (SSRI) alone and in combination. Controversy continues about the accurate diagnosis of bipolar disorder in young children, although consensus is beginning to emerge (NIMH Research Roundtable on Prepubertal Bipolar Disorder, in press). Difficulties in diagnoses have resulted in limited psychopharmacological trials. However, several small, open-label trials have been conducted, although many include heterogeneous groups of children, which may confound results. In addition, an acute NIMH-sponsored efficacy trial has begun and several maintenance trials are underway to study the efficacy of mood stabilizers for bipolar disorder in children and adolescents. Research on diagnostic assessment, outcome measures, combination therapy studies, long-term safety studies, and maintenance trials are sorely needed. Research determining the short-term efficacy of antidepressants for young patients with anxiety disorders has been conducted largely by the RUPPs. OCD is the best-studied of the anxiety disorders, as evidenced by FDA approval of three psychotropic agents over the past 10 years; further study is needed on the impact of trauma and PTSD.
Few data about effective treatments for schizophrenia and related conditions in children and adolescents are available. With the exception of two small studies (Findling et al., 2000; Kumra et al., 1996), there are no controlled data about the use of new-generation antipsychotics in youths. Only modest amounts of short-term treatment data are available for children and adolescents with autistic disorder/pervasive developmental disorder. An acute and maintenance trial for young people with this condition is currently being undertaken by the RUPPs, and new models have been developed to examine the effectiveness of medications in this population.
Yet, as with other disorders, combination pharmacotherapy and long-term safety studies with large numbers of patients are still lacking. Further studies are needed to assess how these scientifically proven treatments can be successfully transported and sustained in real-world practices. There is a need to better understand the factors contributing to the use or lack of use of efficacious treatments in the real world, including individual, familial, provider/organizational, systemic, and societal factors.
Crossing the Boundaries
To date, most pharmacologic drugs have been studied in open trials. The limitations of available safety data from randomized controlled trials (RCT’s), and the difficulties of mounting sizable trials in children and adolescents, suggest the need to augment our knowledge in other ways. Knowledge from several areas of basic science is particularly relevant. Longitudinal pharmacoepidemiological studies in children are needed to better understand the long-term risks or benefits associated with psychotropics. Experimental data garnered through the development of animal models can be important in examining the developmental impact of both psychotropic drugs and illness during sensitive periods of neurodevelopment. Fundamental research on the mechanisms underlying and influencing brain development, neuronal signaling, synaptic plasticity, signal transduction pathways, and the biochemical and behavioral actions of therapeutic agents in animals and humans have important implications for the understanding of individual differences in treatment response. Knowledge about the mechanisms of action of therapeutic interventions can also have important implications for the development of new medications for treatment of childhood disorders.
Obstacles and Gaps
Pediatric psychopharmacology is no longer in its infancy; it is taking the small, tentative steps of a toddler. Yet, several issues continue to impede progress in this area. The safety of psychotropic drugs is a concern—children are growing and developing and, hence, are perceived to be more vulnerable to drug effects. Current assessment methods are not well developed, and preclinical models to assess possibly subtle developmental effects are inadequate. Moreover, the ascertainment of adverse events is a particular challenge, especially in young children. Optimal approaches for studying the safety of psychotropics in children are needed. Another difficulty relates to diagnosing young children. Debate continues around whether or not diagnoses such as ADHD, major depressive disorder, and other psychiatric diagnoses that are well accepted in older children are meaningful in younger children. An alternative view is that much of the prescribing of psychotropics in preschoolers, especially for conditions other than ADHD, represents treatment of nonspecific symptoms such as aggression or self-injurious behavior. If so, are these nonspecific symptoms reasonable targets for research?
Methodological paradigms of pediatric psychopharmacology are limited and are often modeled after adult studies. Issues of comorbidity, polypharmacy, the effects on neuro-ontology, and the impact of combining medications with behavioral or other nonpsychopharmacological treatments need to be considered in study designs that should both rigorously test medications and carefully consider both the risks and the potential benefits of psychotropic agents. Many psychiatric disorders are chronic, recurrent, and impairing. For example, relapse and recurrence of depression in children is equal to or surpasses that in adults (Emslie et al., 1998). Yet there are no controlled data on the effectiveness of antidepressants in preventing relapse or recurrence. Study designs that look beyond acute treatment to examine the long-term safety and efficacy and the impact of treatment on the natural course of illness are needed. Specific gaps include the lack of adequate clinical trials that examine how best to treat patients with subclinical disorders such as depressive disorder not otherwise specified, dysthymia, or major depression with genetic high risk for bipolar disorder, and youths with comorbid psychiatric or medical conditions (e.g., substance abuse, diabetes, asthma).
Other areas that need development include the use of psychopharmacology to treat substance abuse in teenagers, psychopharmacological management of neglect, physical and sexual abuse, and pervasive developmental disorders. Studies on the psychopharmacological management of nonspecific psychiatric symptoms are also needed. There is a growing recognition that there is a group of children who are physically aggressive who do not suffer from a mood or anxiety disorder. Future work should help to characterize this group and develop and further examine outcome measures to observe the effects of therapies, including medications. Another set of psychiatric symptoms relates to sleep disturbance. Difficulties with sleep may be quite problematic for children and teenagers. Some sleep problems may be due to medical conditions or prescribed agents. Although soporifics are commonly used in these children, few data exist about their use.
Recommendations for Psychopharmacology
- We recommend expansion of the RUPPs to include the capacity for launching/conducting large simple trials to study issues such as comorbidity, dosing, and safety and efficacy of medication treatments across diverse cultural populations.
- We recommend increased research on the psychopharmacological management of serious mental illness (e.g., early-onset schizophrenia, bipolar disorder, eating disorders, severe depression) and pervasive developmental disorders (including autism and Tourette’s).
- We recommend that NIMH support the study of nonspecific symptoms that are often the targets of psychopharmacological management in children (e.g., aggression and sleep problems) but that have not been measured specifically. Better assessment measures to identify such symptoms need to be developed so that the symptoms can be assessed across disorders. Trials for these symptoms, independent of disorder, may be considered.
- Disorder-based efficacy trials for new medications are currently being conducted for acute treatment, particularly for medications under patent protection. However, very few studies that examine long-term safety and efficacy are supported. We recommend that NIMH support such studies.
- We recommend the development of better study paradigms on psychopharmacology effectiveness, including augmentation strategies, multiple medication strategies, and the use of algorithmic treatments. Rational approaches to the management of comorbid disorders, medication side effects, and treatment resistance are needed.
- Studies examining reasons why patients do or do not follow treatment recommendations are needed. Further, studies are needed on the impact of the long-term use of medications, including their impact on psychosocial functioning.
- We recommend supporting basic and clinical neuroscience research on mechanisms underlying brain development and the biochemical and behavioral actions of psychotropic agents in animals and humans to increase understanding of drug actions in the developing brain and individual differences in treatment response (i.e., variability in optimal dose levels). Further, research on brain imaging to identify subtypes of diagnostic categories may have different treatment intervention implications.
- We recommend that the study of both the short- and long-term consequences (negative and positive) of pharmacological interventions associated with acute, recurrent, and chronic exposure to psychotropic agents on the developing brain be a priority for new NIMH initiatives.
Science Case in Point: Multimodal Treatment for ADHD
Significant public concerns about stimulant medication, wide variations in treatment practices, and lack of evidence to guide long-term management of ADHD led to the development of the NIMH Collaborative Multisite Multimodal Treatment Study of Children with ADHD (MTA). This 5-year study of treatment of ADHD and its associated comorbid conditions examined the long-term effectiveness of medication versus behavioral treatment versus combined treatment, and compared these results to routine community care. Using a parallel-groups design, 576 children (7 to 9 years of age) with ADHD were recruited across six sites and randomized to four treatment conditions: Medication alone, psychosocial treatment alone, a combination of the two, and community comparison. This study was designed to provide a large enough sample size to address the multiple questions about treatment strategies for ADHD, namely, to determine what treatments (medication, behavioral treatment, parent training, school-based intervention) would benefit which children (comorbid conditions, gender, family background), in what domain of functioning (cognitive, academic, behavior, social skills, family relations), for how long, and to what extent.
The findings: Medication management and combined treatment were superior to behavioral treatment alone and to routine community care in targeting core ADHD symptoms for up to 14 months. Although medication management yielded the most improvement in core ADHD symptoms, the combined treatment was necessary to produce results consistently superior to routine community care for addressing non-ADHD symptoms (oppositionality/aggression and internalizing symptoms) and functional outcomes (achievement, parent-child relations, and social skills)(MTA Cooperative Group, 1999a; 1999b). Furthermore, the combined treatment allowed children to be successfully treated over the course of the study with lower doses of medication compared to the medication management group.
Overall, these findings held across all six research sites, despite substantial cross-site differences in sample demographics. Therefore, the study’s results appear to be applicable and generalizable to a wide range of children. Despite the scientific evidence and availability of the state-of-the-art treatments utilized in this research protocol, such treatments are not readily available in the real world. Differences in quality and intensity of the treatment regimens between study protocol and real-world treatments account for superior improvements seen in children treated as part of the study. Further studies are needed to assess how these scientifically proven treatments can be transported to and sustained in real-world practices. There is a need to better understand the factors contributing to the use or lack of use of efficacious treatments in the real world, including individual, familial, provider/organizational, systemic, and societal factors.
A couple of surprising findings emerged from this study. First, despite the superiority of medication management on core ADHD symptoms, teachers and parents indicated higher levels of satisfaction with treatments that included the behavioral therapy component. Second, even though routine community treatment usually included medication, treatment effects were inferior to the medication management alone. This discrepancy is related to the quality and intensity of the medication management treatment, including longer and more regular visits, closer monitoring of side effects, more frequent and higher dosing, and regular contact with teachers whose input was used to adjust the child’s treatment. Third, contrary to expectations about the superiority of combined treatment on parenting and family stress, combined treatment did not produce significantly better effects on family stress variables than either medication or behavior management alone. All three MTA treatment protocols did not differ significantly from the community treatment on family stress, although they were more effective in decreasing negative and/or ineffective parenting (Wells et al., 2000). However, combined treatment, and not behavior management alone, was necessary to produce improvement in children’s social skills and reduction in disruptive behaviors in school. This effect was mediated by decreases in negative or ineffective parental discipline (Hinshaw et al., 2000). This finding suggests the need to appreciate the complexity of the interrelationships among the various types of interventions.
6. Combined Interventions and Services Effectiveness
Progress
A 25-year history of clinical trials of psychosocial treatments for a range of child and adolescent disorders has culminated in several landmark meta-analytic studies (Weisz, Weiss, Alicke, & Klotz, 1987; Weisz & Weiss, 1993; Weisz, Weiss, Granger, & Morton, 1995); see Section II.B.4. Psychosocial Interventions, for further discussion. These meta-analyses have concluded that psychosocial treatments for children and adolescents do indeed improve outcomes, and that the mean effect size for these therapies is analogous to those found in similar analyses of adult psychotherapies. In a related vein, several hundred trials of stimulant treatments in pediatric psychopharmacology have been launched in this same time frame (Jensen et al., 1999), and these studies have found that such treatments are safe and efficacious for children with pronounced problems of attention regulation and impulse control. Yet most children who receive care in communities receive a combination of services (see the Clinical Case Study: Childhood-Onset Depression, appendix B, as an example). Those with serious problems often have a variety of needs, some of which are in the mental health sphere and some of which are not. These services may include a variety of behavioral, interpersonal, or group therapies and medications, as well as a broad range of school-, home-, or community-based services targeted toward the child’s ecology.
Only in the past 8 years has careful attention been paid to the relative effectiveness of medication or psychosocial/behavioral treatments singly or in combination, and only for two disorders of childhood and adolescence—ADHD (MTA Cooperative Group, 1999a; 1999b) and adolescent depression (the Treatment of Adolescent Depression Study [TADS]). These studies represent important advances in the science of children’s mental health because they offer the opportunity to compare outcomes associated with different types, levels, intensities, and dosages of treatments. These studies can thus yield important policy-relevant data that can inform treatment planning decisions at local, State, or Federal levels (Burns, 1999).
Beyond specific treatments for specific disorders, a broad array of community-based services exist, which, in the past 15 years, have become increasingly available to families of children or adolescents with serious emotional disturbances. In large part originating from two prominent reports, “Unclaimed Children” (Knitzer, 1982) and the “Systems of Care” monograph (Stroul & Friedman, 1988), concerted Federal attention has been paid to encouraging partnerships among local leaders of mental health, general health, education, child welfare, juvenile justice, and substance abuse agencies, strong family involvement, and a less fragmented and more seamless systems of care (Friedman, 2001). The “systems of care model” developed by Stroul and Friedman (1988) emphasized individualized, comprehensive care in response to the varied and multiple needs of children and families. This model articulated a series of principles that were centered on maintaining children within their communities, coordinating services, involving families centrally in delivery and planning of treatments and services, and ensuring the cultural relevance of services provided.
Yet the research base on the systems of care has lagged behind the policy emphasis on creating such systems of care. The systems of care model was the focus of a series of studies in the early 1990’s that were undertaken to assess the degree to which reform of the system would influence changes in practice and therefore lead to clinical improvements. The initial studies focused on comparing a continuum of care model, called the Fort Bragg Demonstration Project, with usual service delivery models (Bickman, 1996a). A follow-up study, which included random assignment to a system of care model or to usual care, was conducted in Stark County (Bickman et al., 1999). Both studies demonstrated that system coordination alone did improve access to services and satisfaction, and modestly improved functioning. System coordination also reduced the use of hospitalizations or other restrictive forms of care (Bickman et al., 1999; Bickman, 2000; Bickman, 1996b; Lambert & Guthrie, 1996). However, clinical outcomes for children (e.g., symptom reduction) were the same whether children were receiving coordinated services through systems of care or usual services, and the cost was considerably higher for systems of care.
As a result of these findings, scientific emphasis was shifted away from general studies of “systemness” to the clinical effectiveness of services within these systems of care and especially to the types, dosage, and intensity of treatments delivered (Henggeler et al., 1997; Hoagwood, 1997; Weisz, 1997). In particular, the transportability of efficacious clinical treatments into mental health services has become a central focus of new efforts, as has attention to the range of clinical, functional, and service outcomes (Burns, 1999; Hoagwood, Jensen, Petti, & Burns, 1996; Jensen, Hoagwood, & Petti, 1996). Further, greater attention has been paid to the fidelity of implementation of “systems of care” principles at the practice level.
In the past 2 years, several reviews of the evidence base on the effectiveness of specific services have been completed (Burns, Hoagwood, & Mrazek, 1999; Weisz & Jensen, 1999). In general, these reviews have revealed the existence of empirically validated interventions such as intensive case management, therapeutic foster care, home-based therapies, especially multisystemic therapies (MST) and nurse home-visitation models. Studies of intensive case management, therapeutic foster care, and MST demonstrate that there are alternatives to lengthy inpatient treatment that can help maintain a child within his or her community setting. Adequate supervision, therapist training, and institutional program support are essential to successful outcomes from these services (Burns, 1999; Chamberlain & Reid, 1991; Schoenwald et al., 2000a). Given the particularly high financial expenses associated with psychiatric hospitalizations and incarcerations, findings related to the cost savings of these approaches have been especially important in service planning efforts.
In addition to these services, progress has been made in identifying a range of school-based interventions that have been found to be effective. Children identified in school as being in need of mental health services are more likely to actually enter and receive them when the services are offered in school, as opposed to within the community (Catron, Weiss, & Bahr, 1994). Although schools do not primarily focus on the delivery of mental health services, academic-related functional impairments and logistical accessibility make schools a logical and important point of access for interventions and services for children with emotional or behavior problems. Some of the empirically supported treatments for childhood behavior problems have been conducted and found to be effective in school settings. These treatments include targeted classroom-based contingency management to reduce the incidence of disruptive behaviors in children diagnosed with ADHD (Pelham, Wheeler, & Chronis, 1998) and in children diagnosed with other conduct problems (Brestan & Eyberg, 1998), and behavioral consultation with teachers to help accommodate difficult students in the classroom (Fuchs, Fuchs, & Bahr, 1990).
School-based preventive interventions designed to target children at risk for emotional or behavior problems have also been shown to reduce symptoms and increase positive coping strategies; they include cognitive group interventions to modify adolescents’ depressive thinking (Clarke et al., 1995) and social problem-solving skills for elementary school-aged children at risk for depression (Jaycox, Reivich, Gillham, & Seligman, 1994). Finally, there is evidence of school-based preventive interventions that reduce the risk for conduct problems, such as interventions that involve multiple components, targeting classroom, home, and peer environments (Conduct Problems Research Group, 1999; Reid, Eddy, Fetrow, & Stoolmiller, 1999).
Crossing the Boundaries
A series of trials is currently underway to evaluate a range of services. These trials are likely to yield important information in the next few years. They include family psychoeducational and support programs, school-based wraparound services, and clinic-based treatments for depression and anxiety disorders, among others (Burns & Hoagwood, in press).
In addition to the progress that is being made on the impact of treatments and services on child and adolescent functioning, significant advances have been made in understanding factors related to engaging families in treatments. Unless families are motivated and able to access effective services, the evidence base will be unused. Studies have been launched to better understand those factors that influence access, dropping out of care, and engagement (Armbruster & Fallon, 1994; Greenbaum, Dedrick, Friedman, Kutash, Brown, Lardieri, & Pugh, 1998; Kazdin, Holland, & Crowley, 1997; Weisz, Weiss, & Langermeyer, 1987; 1989). Unfortunately, there is increasing evidence that children who are from especially vulnerable populations (e.g., children of single mothers, children living in poverty, minority children) and those with the most serious presenting problems are less likely to stay in treatment past the first session and more likely to discontinue services prematurely (Kazdin & Mazurick, 1994). Models for enhancing a family’s service engagement have demonstrated decreased rates of premature treatment termination when such models are used (Santisteban, et al., 1996; Szapocznik, et al., 1988). A similar engagement intervention has been used among inner-city, primarily minority families to increase attendance at initial mental health service appointments (McKay, McCadam, & Gonzales, 1996; McKay, Stoewe, McCadam, & Gonzales, 1998). These preliminary efforts at increasing engagement are particularly noteworthy given the research that supports the importance of involving children’s caretakers in mental health treatment. For instance, family participation during and following day-treatment hospitalizations (Kutash & Rivera, 1995) and inpatient hospitalizations (Pfeifer & Strzelecki, 1990) has been shown to be essential to obtaining and maintaining positive outcomes. Consequently, continued efforts to increase mental health service engagement and entry are necessary.
Finally, an important body of work is uncovering potentially ineffective treatments. As pointed out by Weisz and Hawley (1998), null or even negative effects can be instructional but, unfortunately, are often not reported. The recent report “Youth Violence: A Report of the Surgeon General” (U.S. Public Health Service, 2001) estimates that many of the services provided to delinquent juveniles have little or no evidence base. Worse yet, a recent study indicated that peer group-based interventions might actually increase behavior problems among high-risk adolescents (Dishion, McCord, & Poulin, 1999). In addition, despite their prevalent use in mental health settings, there is little empirical justification for the use of nonbehavioral psychotherapies to treat disruptive behavior disorders (Weisz, Donenberg, Han, & Weiss, 1995). Finally, common treatments for children with complex emotional and behavior problems are group homes and inpatient hospitalization (Burns, Hoagwood, & Mrazek, 1999). Yet existing research indicates that improvements are not maintained once the child is returned to the community (Kirigin, Braukmann, Atwater, & Wolf, 1982). The lesson to be learned from these examples is that in some cases, it is wrong to assume that some treatment or service is better than nothing at all.
Obstacles and Gaps
While progress in creating an evidence base on combined treatments and services has been rapid in the past 10 years, the need to link clinical treatments more forcefully to service provision is underscored by the fact that most of the services available in most communities have no empirical support behind them (English, in press). Further, the number of children with untreated mental illnesses is as high now as it was 20 years ago (U.S. Public Health Service, 2000).
To address the significant unmet mental health needs of children and their families, the traditional paradigm for creating an evidence base on the clinical safety, efficacy, and utility of treatments must be revisited. The traditional paradigm involves conducting a series of controlled laboratory trials, with dissemination, implementation, and deployment appended at the end of the process. This model, called the Clinic-Based Treatment Development Model, may not be well-suited to ultimate use in clinics or community settings, because many of the real-world factors that researchers consider “nuisance variables”—and therefore rule out or control experimentally—are precisely those variables that need to be understood and addressed if treatments are to work well in real-world practice (Weisz, 2000). These variables, or real-world exigencies (e.g., providers too overwhelmed to learn a new treatment protocol, comorbidity, parent substance abuse or pathology, and life stressors that lead to early terminations or no-shows), may need to be directly addressed within the development, refinement, and testing of treatments and services if these interventions are to be maximally effective.
The critical need for comprehensive and intensive services as alternatives to institutional care is supported by recent evidence documenting the benefits of multiple interventions (Burns, Hoagwood, & Mrazek, 1999). Treatments with strong evidence for youth with severe emotional disorders include MST, intensive case management, and treatment foster care; for a number of other treatments, there is at least one randomized clinical trial (e.g., mentoring, family education and support). The availability of these interventions across the country is minimal, as is experience in these settings with the diagnostic-specific psychosocial and psychopharmacological treatments. Research is needed to determine if these evidence-based interventions are effective in the community, to address how to adapt or modify such interventions as necessary, and to learn how to transport and sustain them in the community. The emphasis on providing such services where children live suggests the need to locate these services in public sector settings such as education, primary care, juvenile justice, and child welfare, as well as in mental health settings.
Recommendations for Combined Interventions, Service Effectiveness, and Transportability
- We recommend the use of grant supplements to current service effectiveness projects to examine factors influencing the adaptability and sustainability of interventions (e.g., different roles of family in the research process, strategies for engaging families, and ways of increasing or maintaining treatment fidelity).
- We encourage careful attention to issues of defining, characterizing, and operationalizing current practice. Currently, researchers largely ignore usual practice because the variability within and across practice settings makes these processes extremely difficult and complex to measure. Yet, understanding intervention approaches developed in the field is important, as such approaches often reflect the needs of children and families and the constraints of personnel, as well as organizational and system limitations. Most of these studies will not be randomized trials because of the nature of routine practice.
- We recommend studies that examine how existing services (e.g., school-based, case management, mentoring, family support), combined treatments, and novel delivery mechanisms (e.g., Internet-based) can be used to augment clinical interventions to meet the significant needs of children with severe mental illness or those with multiple problems more successfully.
- We recommend studies on the impact of family engagement and choice regarding the acceptability of interventions.
- We recommend that a mechanism such as a B/START (Behavioral Science Track Award for Rapid Transition) be used to establish community collaboration prior to implementing research programs.
- We recommend that NIMH develop a national system or a series of regional systems to track the utilization and costs of child mental health services. The systematic tracking of broad indicators of utilization and costs, such as inpatient days, outpatient utilization by insurance status, and socioeconomic characteristics would allow a more timely recognition of the effects of major changes in the health care system, including increasing or decreasing inequities. As part of these tracking systems, pharmacoeconomic studies are encouraged. Integration of data (service use and costs) from other settings likely to provide a substantial amount of services (e.g., the education, juvenile justice, and child welfare systems) not captured in the existing health databases is essential. An increased focus on the role of private insurance in covering mental health services for children could provide important lessons. Traditionally, most of the information about behavioral health care has come from the public system. But privately insured children account for the largest proportion of the population with mental health expenditures. Even so, some of the most costly treatments continue to be paid for with public funds. Finally, this tracking initiative could facilitate the development of a conceptual integration to link policies (e.g., parity) and market forces (e.g., growth of managed care) to service use, processes of care, and outcomes. In the absence of a more complex model based on a national data system, health care debates will be informed by simple descriptive comparisons (e.g., outcomes by financing system) and extrapolations based on isolated studies.
- New technologies will change care dramatically over the next decade. In addition, delivery of care is moving away from clinic-based models and toward models of patient-centered family care delivered in out-of-office settings, including on the Internet, in the home, in the school, in primary care and other settings. Because this trend is likely to continue, we recommend that studies of nontraditional delivery of services be encouraged and supported through program announcements or special funding initiatives.
Science Case in Point: Multisystemic Therapy (MST)
Multiple randomized trials have shown beneficial effects of an intervention approach called multisystemic therapy (MST) with youngsters who show serious antisocial behavior. Most of the youths in these trials have been arrested multiple times prior to treatment, and MST has been shown to markedly reduce rates of subsequent arrest. The approach involves efforts to work with both the individual youngster and several elements of the youngster’s environment, to create conditions in which antisocial behavior will be reduced and prosocial behavior increased. For example, the MST therapist may work with parents on their skills in youth monitoring and discipline, as well as rewarding appropriate behavior. The therapist may also work with teachers and other school staff, and with the family’s neighbors and friends, to create conditions in which youth behavior will be monitored closely and appropriate behavior encouraged and supported. The intervention is heavily focused on environmental change, but also can involve individual work with the youth. The therapist’s time is spent in the settings where the youth and family spend time; therapists do not even have private offices.
MST, as described by Henggeler and colleagues (Henggeler, Schoenwald, Borduin, Rowland,& Cunningham, 1998), was heavily influenced by general systems theory (von Bertalanffy, 1968) and social ecology theory (Bronfenbrenner, 1979) as applied to diverse empirical findings on the causes and correlates of behavioral and mental health problems in youth. The early work on MST involved efforts to apply the basic principles via traditional therapy office visits in an urban setting, but the treatment developers were increasingly frustrated by client attendance problems and limited access to information on their young clients’ environments. To cope, Henggeler and colleagues developed an environmentally focused intervention approach in which the therapists went to the child and family rather than requiring office visits. The resulting approach to intervention, MST, has now been tested and found beneficial in a series of randomized trials (described in Henggeler et al., 1998). Systematic reviews have identified multiple trials showing beneficial effects of MST for youth conduct problems and antisocial behavior (e.g., Brestan & Eyberg, 1998; Kazdin & Weisz, 1998). MST, modified for use with youths presenting with psychiatric emergencies, can also serve as a clinically viable alternative to inpatient psychiatric hospitalization, with positive outcomes including decreasing externalizing symptoms and improving family functioning and school attendance (Schoenwald et al., 2000b). Preliminary evidence of efficacy with families referred for physicial abuse of youth (Brunk, Henggeler, & Whelan, 1987) is being further investigated in a newly funded clinical trial comparing MST with parent-training approaches following substantiated reports of physical abuse (Swenson, MH60663). In general, the clinical trials already completed involve some elements of deployment in that many of the youngsters treated have arrest records, have been referred to MST by the juvenile justice system, and are clients of multiple systems. In most of the trials, State or local agency stakeholders were directly involved as consultants to the study. While the earlier trials generally used university-employed project staff, this has changed with the later trials, and actual providers in community agencies have been trained—and in some cases, retrained—to deliver MST. The next step in the deployment agenda involves studying the transportability of MST by testing the effects of organizational climate on the ability of real-world clinical therapists to adhere to MST principles and ultimately to effect positive outcomes for children (Schoenwald, MH59138; Schoenwald et al., 2000a).
7. Dissemination Research and System Improvement: Closing the Loop
Progress
Long-standing concern about the fragmentation of mental health services for children, adolescents, and their families has led to a series of major national initiatives and calls for reform. Foremost has been the “systems of care” movement (see Section II.B.6. Combined Interventions and Services Effectiveness) which advocates coordinated services for children and families, attention to family-centered services, and adherence to cultural relevance in service and treatment planning. As indicated in the previous section, the systems of care studies demonstrated that system coordination alone did improve access to services and satisfaction, and modestly improved functioning. System coordination also reduced the use of hospitalizations or other restrictive forms of care (Bickman et al., 1999; Bickman, 2000; Bickman, 1996b; Lambert & Guthrie, 1996). However, clinical outcomes for children (e.g., symptom reduction) were the same whether children were receiving coordinated services through systems of care or usual services, and the cost was considerably higher for systems of care. Yet, the multiple problems associated with children who have serious emotional disturbance may best be addressed with a “systems” approach in which multiple service sectors work in an organized, collaborative way.
These findings have led to a reorientation of systems research in three major directions. Increased attention has been paid to the effectiveness of services within systems of care and especially to the types, dosage, and intensity of treatments delivered (Henggeler et al., 1997; Hoagwood, 1997; Weisz, 1997). This redirection is described in the previous section. There has also been a focus on the features of organizations—especially child welfare agencies and, to a lesser extent, schools—that impede or facilitate the delivery of effective treatments or services. Much of this work has arisen from the studies of Glisson and colleagues (1998), who developed models and measures of organizational culture and climate. Glisson has determined that these features predict psychosocial outcomes for children in the custody of the State. These findings have led to greater attention to the characteristics of organizations within systems of care that may be malleable and that may affect the ability of providers to deliver effective mental health care to children (Hohmann, 1999; Schoenwald & Hoagwood, 2001). Further, the relationship between the system level and the practice level must be clarified, including the need to assess treatment intervention fidelity.
Attention to systems change has redirected research toward questions about the sustainability and disseminability of effective services within practice settings. Burns and colleagues (1999) argued that the continuing, well-documented, and persistent unmet need for mental health care among children and adolescents in this country necessitates a timely response by those in both the scientific and practitioner fields. She proposed the creation of a research agenda on clinical interventions for youth to accomplish four tasks: (1) synthesize (through reviews of the evidence base) the status of science on promising interventions, (2) assess quality indicators of outcomes to improve standards of clinical practice, (3) evaluate outcome measures, and (4) develop a new research phase model for connecting research to practice. Important to this effort is not only identifying the evidence base on service effectiveness but also attending to the models of dissemination that will enable it to be used in clinical practice. The aim is to address historically intractable problems through learning how to shift relevant evidence-based interventions to youth with the most severe disorders. Critical activities will include (1) establishing criteria for interventions to be disseminated, (2) developing “user-friendly” training and supervisory and quality monitoring materials, and (3) conducting dissemination research to test theoretical and empirical approaches for changing practitioner and organizational behavior.
A comprehensive dissemination and knowledge transfer program would involve all three of these classes of activities. It would require that research findings, after having successfully gone through rigorous scientific peer review procedures, be provided in formats and language appropriate for other audiences, such as providers and consumers. Above and beyond the preparation of appropriate materials, a comprehensive and effective dissemination effort requires an interpersonal component. The National Center for the Dissemination of Disability Research (NCDDR) (1996) reported that perhaps the most consistent and ubiquitous finding in the literature on knowledge utilization is the primacy of personal interaction, and Crandall (1989) indicated that “adequate materials and procedural guidelines, coupled with responsive, in-person assistance during later implementation, are imperative for maximum success.” This finding is consistent with the finding that credibility of the source of information is critical for knowledge utilization. “Credibility” refers to both the level of perceived expertness and trustworthiness (NCDDR, 1996). Personal interaction is very important for promoting a level of trust that is more likely to result in utilization of research findings.
The implications are that even with advances in technology, in the complex area of interventions for child mental health disorders, effective knowledge transfer is labor-intensive and expensive. Researchers who have developed successful interventions need to be prepared to respond to requests for assistance and to proactively generate interest from groups that may implement the intervention with high fidelity to its principles and processes. Agencies such as NIMH and CMHS that are interested in promoting the use of evidence-based interventions in children’s mental health need to identify mechanisms to study and support this process.
Crossing the Boundaries
It is increasingly clear that a goal of public health science is ensuring that science-based services are embedded into everyday practice and used by all. Doing so necessitates new areas of investigation—what might be called dissemination and implementation science—to understand how best to position and sustain effective services in communities and identify factors that impede this positioning. Achieving this goal requires both a new genre of study and persistent attention to questions about why services are effective. Toward this end, scientists must engage families, providers, and other mental health stakeholders to increase the likelihood that the research is relevant to their needs and will produce findings that are credible and scientifically valid.
Changing Practitioner Behaviors
As knowledge about treatments and services with known outcomes becomes more widely available (e.g., combination or medication therapies for children with ADHD), it will be important to understand how best to change practitioner behaviors so that this knowledge will be used. Different strategies are likely to be needed for changing the behaviors of providers from different disciplines. Professional associations (e.g., the American Academy of Child Psychiatry, the American Academy of Pediatrics) have developed practice guidelines, but adoption of these guidelines into everyday practice may necessitate studies of characteristics of the practice environment, history of the professional discipline, or credentialing traditions that impede or facilitate such adoption. Approaches such as academic detailing, widely used by the pharmaceutical industry (Baro et al., 1998; Freemantle et al., 2000), or use of key opinion leaders within communities (Kelly et al., 1993) may be valuable approaches for changing practice. For example, theories of social diffusion suggest that adoption of new strategies or behaviors (such as cessation of smoking or eating a healthier diet) depend in part on the social value attached to the opinions of leaders who encourage such changes. The impact of opinion leadership with reference to children’s mental health treatments or services could be examined for its applicability to a range of services, providers, and service environments.
Changing Organizational Behaviors
As work by Glisson and Himmelgarn (1988) has shown, the organizational culture and context within which mental health providers work directly influences the attitudes, motivations, and behaviors of providers, and consequently indirectly influences child outcomes. Studies of the impact of organizational culture and climate on sustaining the fidelity of the therapeutic process and outcomes need to be conducted if science-based services are to be maintained within community-based agencies, schools, or health care settings. Studies are also needed to identify aspects of the practice environment that facilitate therapists fidelity to treatment. In addition, it will be important to examine those proximal features of the practice environment that influence the clinician/patient relationship and why some clinicians are motivated to change and adopt new strategies and others are not. To conduct such research, partnerships among scientists, providers, and agency administrators must be initiated from the very beginning.
Amplification of Interventions to Increase Organizational or Community Fit
A substantial knowledge base on school mental health services (Rones & Hoagwood, 2000) and psychosocial treatments for children exists in the literature (Kazdin, 2000b; Weisz et al., 1995; Weisz, Huey, & Weersing, 1998). Yet for the most part, these services have no sustaining power within schools, clinics, or agencies beyond the tenure of their creators. They come and go as grant support, faculty members, and faculty interests come and go. Studies of the augmentations are needed that will help to maintain scientifically driven services within a range of agencies and organizations. Augmented models, such as additions of wraparound services to core prevention programs, neighborhood resource centers, or additions of case management to after-school programs, may increase the likelihood that these services will be sustained.
Adaptation of Treatments to Increase Organizational or Community Fit
Because there now exists a knowledge base of hundreds of treatment studies demonstrating improved outcomes for children with a range of behavioral, emotional, or psychiatric problems, extension of this knowledge into a range of community settings would be valuable. However, to date, little attention has been paid to the kinds of adaptations needed to make these treatments practical and feasible for use in community settings. Because much of the knowledge about treatment efficacy has been developed in academic settings, a new generation of research is needed to address questions such as how far to adapt a manualized therapy for use within a mental health clinic (given that most children will attend only four or five sessions), what kinds of outcomes to assess when a treatment is embedded in a new service setting, or how to engage families in tailoring a treatment to enable it to match familial or cultural values and experiences. It will also be important to develop research-based triage standards to determine when children’s mental health needs are best managed by persons with different levels of mental health training. In addition, issues about whether to treat co-occurring disorders sequentially or simultaneously will need to be addressed for children with mental health and substance abuse problems.
Deconstruction of Interventions to Identify Core Potencies
Studies that deconstruct or dismantle therapies into elements that eventuate certain outcomes and that are practically amenable to being taught to mental health care providers (e.g., nurse providers, teachers, health care paraprofessionals) are sorely needed. A related issue is identifying the dosage of a given service that is needed to obtain a particular outcome. In part, the issue of appropriate dosage is being urged forward by the exigencies of health care accountability. The notion of service dose cannot be made meaningful until (1) the services themselves are well-specified, (2) the active ingredients composing the service can be specified, and (3) appropriate statistical scaling methods of dosage are used (Hoagwood, 2000).
Measurement Development: Functioning and Impairment
Measurement of child mental health outcomes has been dominated by attention to syndromes, problem areas, and diagnoses. Yet of greater importance to most health care administrators, teachers, parents, and front-line clinicians is the identification of problems related to a child’s functioning. Unfortunately, the measures that are currently available for assessing functional impairments or competencies are quite limited and reflect outdated notions of functioning. The most widely used measures are either global, thus inadequately reflecting cultural variations, or confound functioning with diagnosis (Canino, Costello, & Angold, 1999). Conceptual problems also plague the area of measurement of functioning. The basic concept originated from Vineland’s notion of “social usefulness,” a concept that was pertinent to adults with mental retardation in the 1930’s, but that is hardly sufficient for understanding children’s mental health needs. Further, the theoretical notions of “functioning” are conceptualized, measured, and used in different ways across the major service systems in which children are seen. As used in health settings, functioning refers to events and consequences such as losing a limb and requiring prosthetic devices. In education, it refers to skills such as social or communication abilities, as well as handwriting. In mental health settings, it may refer to a clinician’s global rating of whether the child completes tasks in school or at home. So measurement approaches that will not confound functioning with clinical syndromes, that will reflect culturally specific attitudes (rather than global ratings), and that can flexibly assess core elements of functioning are needed to cross health, education, and mental health settings.
Obstacles and Gaps
These new research directions will help to connect the research base to clinical practice. However, it should be acknowledged that one impediment to the efficiency and usefulness of the research base has been the scientific model that has driven the development of a usable science. As previously noted, one reason efficacy studies have not been readily deployed into service settings may be that the research model used to drive the development, refinement, and testing of those treatments does not mesh well with the exigencies of clinic or community-based care (Weisz, 2000). In the face of the mounting evidence base, different task forces and separate reviews have applied different criteria and guidelines. Despite the increased attention to evidence-based treatments, there is as yet no consensus on what constitutes this evidence base, how these interventions should be disseminated, or how outcomes for such efforts should be evaluated.
Furthermore, the financing of mental health services is currently not aligned with evidence-based practices. The relationship between financing policy and dissemination of evidence-based care is a close one. The current status quo (i.e., extensive fiscal investment in clinical interventions without an evidence base) is likely to continue unless policy mandates reimbursement for evidence-based care. Policymakers determine which interventions are paid for as well as whether support is available to train providers in evidence-based care. Professional sanctions manifested in training, licensing, and continuing education requirements are also approaches to facilitate change in practice. Providing the efficacy and effectiveness research findings, along with the likely benefits and costs of change, to policymakers and professional organizations is a necessary first step. The next challenge is to create assurances that widespread implementation of innovative interventions is feasible and that benefits obtained under controlled conditions will be sustained in real-world clinical settings.
As the field of mental health services research expands, it will be important to take advantage of opportunities to study new services as they arise, and to do so in a timely manner. Judging by past performance, when treatments are developed and tested via the traditional model, 10 to 20 years may be required to advance to the point at which the treatment can be understood with respect to its effects in a practice setting. This timeframe is impractical and inefficient if the goal of public health science via-a-vis children’s services is to improve practice. Instead, new models are needed, such as the one proposed in this report, to encourage studies of the real-world effectiveness of new treatments or services within the context of the practice setting where the service is ultimately to be placed. Improved dissemination and deployment of research should be a main goal of system reform so that the investment in research is truly extended to children in the United States who need effective treatment and to their families.
Recommendations for Dissemination/Deployment Research
A number of recommendations to improve research in the dissemination/deployment area are provided below.
- We recommend that investigators be strongly encouraged to conduct dissemination studies in public sector mental health sites, collaborating with other child-serving sectors. Because of the major activities of CMHS in promoting systems of care through its Comprehensive Community Mental Health Services for Children and Their Families Program, we strongly endorse the NIMH Program Announcement (PA-00-135), “Effectiveness, Practice, and Implementation in CMHS’ Children’s Service Sites.” This program announcement is sensitive to the need to disseminate evidence-based clinical practice to very high-risk youth receiving services in public sector programs. However, to facilitate meaningful research in these public sector sites, a major technical assistance effort will be necessary to bring together investigators and service sites.
- We recommend that priority be given to research on the factors that facilitate or impede the processes, transportability, or sustainability of evidence-based treatments. Factors identified may include extra-organizational factors (e.g., stakeholder involvement, triage system), organizational factors, provider behavior factors (e.g., attitudes and readiness to change), and family and child characteristics (e.g., attitudes, preferences, or co-occurring disorders) as they are related to dissemination and uptake of effective clinical services. Such factors may guide the development of incentives to optimize the use and sustainability of evidence-based treatments. Such research is especially needed in communities or populations where disparities in access to mental health care are prevalent, including minority communities and the uninsured.
- We recommend that NIMH consider the use of Small Business Innovation Research program funds for deployment, method/analysis development, or dissemination research to develop new commercial products and potentially expand the range, function, and effectiveness of therapeutic services.
- We support continued partnerships with other Federal agencies in order to capitalize on their dissemination arms. These agencies include those of HHS—CMHS/SAMHSA, AHRQ/HRSA, MCHB/HRSA, the Administration for Children and Families, and other NIH Institutes—the Office of Special Education and Rehabilitative Services, Department of Education; and the Office of Juvenile Justice and Delinquency Prevention, Department of Justice, to carry forward research advances in both policy and practice arenas.
- A highly visible, national dissemination effort is needed. We recommend the creation of a Dissemination Center. The research focus of this center would include dissemination and sustainability studies, with a special focus on understanding the validity of evidence-based treatments for minority populations. In order to conduct these studies, theoretical and empirical literature on organizational and practice change will need to be critically and creatively addressed, and different approaches to diffusion will need to be tested. Initial work by the center would be to identify experts in the change process from other fields and to utilize them in adopting or adapting the complex provision of mental health care services for targeted children and families.
III. Infrastructure and Training
Problems and Progress
Mental health research is a broad and complex field in which solutions to problems will likely require the synthesis of knowledge across various disciplines. Because an integrated knowledge base is critical to advancing the etiologic understanding of behavioral and emotional disorders in children and adolescents—and hence developing, implementing, and studying interventions with children within their diverse environments—interdisciplinary training must become the norm. As delineated in the Institute of Medicine (IOM) “Report on Bridging Disciplines in the Brain, Behavioral, and Clinical Sciences” (2000), many barriers to interdisciplinary research exist. In the child mental health arena, salient issues relate to the acute shortage of developmentally oriented clinical investigators with the interdisciplinary training to leverage rapidly emerging knowledge in developmental neuroscience, developmental psychology, cognitive and behavioral neuroscience, genetics, and other areas of basic science. One specific challenge is to reduce the fragmentation of knowledge across areas of child and adolescent psychiatry, pediatrics, adolescent medicine, developmental and behavioral pediatrics, pediatric neurology, developmental and clinical psychology, and developmental neuroscience. Most academic settings are organized into discipline-specific programs and provide little training in this interdisciplinary perspective.
The insularity of academic disciplines has resulted in a dearth of research training programs and mentors that bridge the traditional boundaries of the various scientific disciplines. Further, funding for interdisciplinary research is hampered by the conservative nature of grant review or study sections. Investigators who attempt to test innovative models or alternative paradigms are frequently penalized. For example, study sections are often unreceptive to investigations that seek to combine electrophysiological, molecular, and biochemical approaches with studies of environmental or activity-dependent determinants of brain and behavioral development.
The shortage of well-trained mental health investigators focused on children and adolescents has been recognized repeatedly (IOM, 1989; NAMHC, 1990; UNOCCAP Oversight Board, 1998). A major obstacle to expanding the pool of junior scientists is the lack of sufficient financial support for training. Traditional research training mechanisms are underused, in part, because training grants typically provide little or no overhead support in the form of indirect costs for faculty salaries. Also, in recent years, clinical revenue for many academic health sciences centers nationwide has declined. This decline, combined with the rise of financial requirements for faculty, further constrains resources to offset faculty time devoted to training and mentoring.
These issues are especially challenging for those interested in child mental health research because (1) child research is more expensive owing to the need for additional ethical precautions, the necessary involvement of families, the use of proxy informants, and sample size issues; (2) child psychiatric training requires longer training periods than traditional programs because trainees in many disciplines must complete regular programs and then complete additional pediatric training; and (3) free-standing children’s hospitals and general hospitals and their child training programs, in general, are not reimbursed by Medicare for graduate training similar to other clinical programs, and thus bear a higher portion of all training costs.
Funding Trends at NIMH—Research and Training Grants
Funding trends at NIMH highlight some of these issues. Overall, there has been an increase in the number of grants on research related to children and adolescents over the decade since the first NIMH National Plan for Research on Child and Adolescent Mental Disorders. From 1989 to 2000, the number of child-related grants funded by NIMH increased from 460 to 775 (see Figure A), and the amount of funding increased from $95 million to $262 million (see Figure B). The increase in research in the child area is proportionate to the increase in the overall NIMH research portfolio. In other words, despite the increase in numbers, the percentage of grants related to children and adolescents has actually remained steady as a proportion of the overall NIMH portfolio, both in terms of number of grants (approximately one-quarter; see Figure A) and amount of funding (approximately one-third; see Figure B).
Training funds include career awards (K grants), individual fellowships (F’s), and institutional training grants (T’s). Over the past decade, the distribution of training funds has shifted. Of the research funds related to children and adolescents (see Figure C), institutional training grants have not kept pace over the last 10 years. The proportion of institutional training grants has decreased in comparison to the total child portfolio, while career awards (K’s) targeted at bringing in new researchers have increased proportionately. Training fellowships aimed at supporting pre- and postdoctoral trainees have remained quite constant (at or below 0.5 percent). When viewed in context of how training grants are funded across the whole Institute (Figure D), it appears that the trend of decreased institutional training grants and increased K awards over the past 10 years is reflected Institute-wide. However, individual child training fellowships have not kept pace with the fellowship-funding pattern of the overall Institute. The percentage of funds allocated for fellowship training across the Institute is consistently double the percentage for child research. A second trend is the shift in funding from institutional training awards to career awards. Because institutional training grants are important in preprofessional training, the implication of this shift is that less money for training is available early on in the careers of potential child mental health investigators, a time when critical career choices are being made. At the same time, K awards are critically important to research career development. Currently, no formal mechanism is available to support interdisciplinary research training.
Training Issues From the Perspective of Professional Associations
The workgroup considered a wide range of training-related problems and issues central to research in child mental health. In its deliberations, the workgroup solicited input from approximately 10 major professional associations involved in training mental health scientists. Organizations surveyed included the National Association of Social Workers, the American Academy of Child and Adolescent Psychiatry, the American Psychological Association, and the Society for Developmental and Behavioral Pediatrics (see appendix C for a list of organizations who responded).
Respondents were asked about (1) major barriers to training future mental health scientists in child and adolescent issues, (2) problems in training capacity, (3) timing of training in mental health research, (4) availability of training in evidence-based treatments or services or in children’s service systems, (5) features of the child mental health infrastructure that either encourage or discourage research training, and (6) new training models that integrate training across disciplines, fields of science, or systems. In synthesizing the responses—responses from social work, child psychiatry, and child psychology—a striking similarity in issues emerges:
- Barriers—A major burden is the financial debt for people going into research training careers; more incentives must be offered. Another barrier is a lack of infrastructure and established programs.
- Capacity to train mental health scientists—Inadequate stipends are provided for the trainees, and the number of role models available for training is insufficient.
- Timing—Current opportunities for training are often introduced too late in the process, usually when the trainees have finished their post-doctorate or internship or when they are at the end of their residency, at the point of having to pay off their debt. Students need to be enticed early on in their career, including at the undergraduate level.
- Training about evidence-based treatments—All respondents felt the current training programs do talk a lot about evidence-based research and treatment within their clinical training, but evidence-based data are limited.
- Mental health structure helping or hindering research—Service issues and clinical training are a hindrance; the pressure is high on trainees and faculty who do not have as much time to spend with training when they have the pressure of clinical demands. In pediatrics, there used to be research that clinicians could do in departments with free, protected time, considered “limited studies.” That has disappeared because of declining reimbursements.
- Transdisciplinary and interdisciplinary training—All programs said some interdisciplinary training occurs.
- The Balanced Budget Act—Academic medical centers hit hard by the Balanced Budget Act, particularly those that focus on the health, well-being, and care of young people, need to be supported.
- Research Units in Pediatric Practice (RUPPs)—Many want to consider expanding RUPPs. A potential problem is that RUPPs are designed in pediatric psychopharmacology and follow a different model.
- Minority training—Minority supplements or some sort of supplements to R-01s should be considered; NIH has a minority training grant program.
- Timing for graduate students—Much of what is said about academic medical centers does not apply to graduate schools. For graduate students, specifically those in clinical psychology, the issue of timing is critical. When the funds are available, it is too late for clinical graduate students, because they have already decided on their career track.
- R-25, child practice research—Institutional groups need to come together to represent a critical mass, assuring review committees that there are enough investigators to carry out this research.
Recommendations
The recommendations below reflect the consensus of the workgroup discussions and the professional association responses. Recommendations are provided to facilitate and support the development of interdisciplinary centers that focus on conducting translational research for children and to expand the pool of well-trained investigators in child mental health.
A. Capacity Building
- We recommend that NIMH develop a payback program whereby individuals who pursue careers in child and adolescent research may apply for loan forgiveness.
- We recommend that NIMH develop additional mechanisms to support mentoring for new research scientists in child and adolescent mental health. This program may include funding for sabbatical leaves or teaching/mentoring time provided in the form of supplements to grants. Funding for teaching/mentoring time is critical because there are so few clinical investigators, all with multiple demands on their time.
- To build the research capacity needed to take advantage of the promise of interdisciplinary research, we recommend that NIMH issue a new initiative for the creation of Child and Adolescent Interdisciplinary Training Institutes (CITIs). Basic requirements would include training or exposure in at least the following scientific areas: basic behavioral and neuroscience, epidemiology, prevention, intervention development, services research, and health economics. Training seminars, summer institutes, and intensive coursework on methodology, statistics, and the range of service settings where mental health services are typically delivered (e.g., schools, primary care, community clinics) would be required. To initiate CITIs, we recommend that NIMH establish one or two pilot educational research experiences in inter-disciplinary and developmental research with the explicit focus of encouraging child and adolescent studies. The overall purpose would be to work out pragmatic and feasibility issues in detail in at least one or two universities on how to effectively integrate basic and clinical training for clinically oriented investigators. Successful pilot programs would serve as a model for further interdisciplinary training programs. We also recommend that the directors of the CITIs meet annually to discuss training initiatives and new programs and to modify educational objectives as needed.
- We recommend that a special announcement be issued for child and adolescent research supplements. Modeled along the lines of minority supplements, they would be used to encourage investigators in other fields (e.g., adult mental health, primary care, education, neurology) to receive training in child and adolescent mental health and thus increase the numbers of investigators with expertise in child mental health research.
- We recommend that NIMH develop a national mentorship program to increase the number of racial/ethnic minorities among NIMH-funded trainees who can address the unique needs of minority children. This mentorship program could include the NIMH Intramural Research faculty. Such an effort is critical in light of changing demographics; minority children are increasingly represented among those with significant mental health needs.
B. Partnerships to Facilitate Research Training
- To enhance child and adolescent research training activities, NIMH should explore opportunities to partner with other Federal agencies. Potential partners include MCHB and AHRQ/HRSA; CMHS/SAMHSA and CSAP/SAMHSA. For example, NIMH should consider MCHB’s Leadership in Education in Neurodevelopmental Disabilities (LEND) programs as an avenue for including more of a mental health perspective.
IV. Future Directions for Child and Adolescent Mental Health Research
Children and adolescents with undiagnosed mental illnesses may spend years depressed, perhaps anxious or withdrawn, unable to learn or unable to make meaningful connections with the people around them. The clinical case example in appendix B highlights the way significant scientific advances in understanding the course and causes of depression, its treatment, and service delivery can be brought explicitly to bear on clinical practice. From a public health standpoint, scientific advances that do not ultimately lead directly to improvements in clinical care are meaningless. The endpoint of scientific progress in child and adolescent mental health is improvement in care. The case example shows us the opportunities for, and limitations of, scientific knowledge in our efforts to reach this goal. Reaching this goal will require partnerships among scientists, families, and other stakeholders to ensure that scientific advances make their way into the clinics, schools, and other settings where children and adolescents receive mental health services. Such partnerships and how they may work are explicated in the conceptual models provided in chapter I, Figures 1 and 2.
This report was written to serve as a strategic guide for transforming the form, function, and purpose of research on child and adolescent mental health. Three key issues have been identified as essential to this transformation: (1) the recognition of the lack of connection between basic science (developmental neurobiology and developmental behavioral science) and clinical intervention development, (2) a commitment to accelerating the pace of intervention development by contextual repositioning of such work within real-world settings, and (3) realignment of the evidence base with clinical and service practice. To accomplish these goals, linkages must first be made among the various scientific disciplines in order to expand and strengthen intervention development. Doing so will entail not only support for interdisciplinary research activities but also encouragement of new training models. Second, the development of new interventions should take into account those contextual and system factors (often considered to be “noise” in traditional studies) that may in fact influence the outcomes of the intervention and their sustainability within diverse communities. Essentially, interventions must be developed that are usable and that attend to social, cultural, or community variations. Third, to improve the dissemination of scientifically proven interventions, those that have been shown to be effective must be used. To ignore such knowledge is to court disaster. But this requires strengthening the knowledge base so that social, cultural, or community factors that affect the value of interventions are better understood.
Priority Area 1: Basic Science and the Development of New Interventions
The linkages among neuroscience, genetics, epidemiology, behavioral science, and social sciences provide opportunities for increasing our understanding of etiology, attributable risk, and protective processes (their relative potency, sequencing, timing, and mechanisms). Such knowledge is critical for the creation of developmentally sensitive diagnostic approaches and theoretically grounded interventions. One critical piece of knowledge needed is an understanding of the etiology of mental illnesses, which can lead to better identification of “high-risk” groups as the target for these early interventions, as well as “high-risk” or vulnerable intervals in development. Despite our appreciation of developmental perspectives, many evidence-based interventions for children and adolescents continue to represent downward extensions of adult models, with limited consideration of basic knowledge about how causal mechanisms or processes may vary across development or sociocultural context. Conceptual approaches and developmental theories are needed to guide intervention and dissemination efforts. Information from developmental neuroscience, behavioral science, and epidemiology should be used to formulate competing and testable hypotheses about those developmental processes that lead to mental disorders. At the same time, knowledge gleaned from intervention testing and dissemination research must inform basic research theory and development.
Priority Area 2: Intervention Development, Moving From Efficacy to Effectiveness
The current model of treatment development (typically followed in biomedical science studies) stipulates that such development begin in laboratory settings; that highly specific sample selection criteria be used; that refinement, manualization or algorithm development, and delivery be carried out by research staff (as opposed to practicing clinicians); and that aspects of the service setting where it is ultimately destined to land be ignored. This model creates an illusion that science-based treatments are not meant to be used or usable. This report suggests that a different model of intervention development be followed. This new model requires two strands of research activity: The first strand necessitates a closer linkage between basic science and clinical realities (as described in Priority Area 1); the second strand requires that a focus on the endpoint and its context—the final resting place for treatment or service delivery—be folded into the design, development, refinement, and implementation of the intervention from the beginning. Furthermore, such interventions should also be developmentally sensitive and take into account family and cultural contexts. Finally, in order to explain why treatments work, it will be important to identify core ingredients of intervention, including the mechanisms that led to therapeutic change and the processes that influenced outcomes.
Priority Area 3: Intervention Deployment, Moving From Effectiveness to Dissemination
For evidence-based interventions to be used in clinical practice, knowledge about effective dissemination strategies is needed. The application of the traditional biomedical model of intervention development does not always lead to interventions that are adaptable, applicable, or relevant to real-world clinical practices. To ensure that the current evidence base is used appropriately, a new genre of scientific effort is needed to better understand factors that influence the transportability, sustainability, and usability of interventions for real-world conditions. Many promising preventive and treatment interventions have not paid enough attention to factors that influence family engagement in services, for example, nor to the broader socioecological contexts and systemic issues that influence access to and use of such services. Such research is critical if the current evidence base on effective interventions is to be brought to scale, sustained in service settings, and made accessible to the children and families in need.
Meeting These Priorities
Barrier to Change
Current research practice and incentives are not well-aligned to promote interdisciplinary research or the development of interventions that are transportable to or sustainable in real-world settings. Further, the research training infrastructure to support a cadre of investigators who can conduct the kind of research necessary to bridge the gaps among mental health researchers from various disciplines or among the research community, practice community, and policymakers is lacking. Such barriers occur at every level, including within the Institute (e.g., NIMH review practices/policies), within child and adolescent psychiatry (philosophical bias toward disease orientation rather than functional adaptation), and within academia, where the insularity of academic disciplines and the academic promotion structure do not support such efforts. Researchers need training so that they can step outside their prescribed area to consider the wider implications of their work on the larger system that affects children’s mental health care and their needs. Incentives must be provided to conduct research regarding the public health significance of their work.
Facilitating Change
In order to facilitate change, NIMH must make concerted efforts from within its own organization, as well as in partnership with other stakeholders in the field of child and adolescent mental health. NIMH needs to carefully consider the significant resources allocated for child research and identify ways to realign the incentives to encourage the linkages that will result in a true interdisciplinary research effort. Clearly, the viability of these linkages depends in part on the scientific advances within each area (e.g., neuroscience, behavioral science, prevention and treatment, and services research). Priorities for advancing research in each area are described in the corresponding sections of this report, and NIMH should pay close attention to guiding this research and research training.
In addition to increasing the interdisciplinary nature of child and adolescent mental health research, NIMH should continue to develop public-private partnerships with advocacy groups, professional organizations, service agencies, the health care industry, and legislators. Such partnerships are critical to ensure that the public has access to the most current, state-of-the-art knowledge on interventions, that limited resources are efficiently used, and that all children and their families have access to appropriate and timely care for their mental health needs. Partnerships with other stakeholders, including academic institutions and advocacy and professional organizations, could be forged to develop incentives for interdisciplinary research training and to create a usable science base that can ultimately address the mental health needs of children and their families.
Closing the Gaps and Meeting the Needs of Children and Adolescents
A public health effort to improve child and adolescent mental health, supported by taxpayer dollars, is warranted only insofar as it leads to improvements in the quality of care that children and adolescents receive and, thus, improvements in the quality of the lives they lead. The toll that preventable, untreated, or poorly treated mental illness takes on children, adolescents, and their families and society is profound and unacceptable. Over the past 10 years a vast amount of knowledge has been garnered about prevention, identification, treatment, and services for mental illness in children and adolescents. This knowledge can and should be used to improve care. But in the next decade, we must be more exacting. The next generation of child and adolescent mental health science will require a transformation of form, function, and purpose if a true public health model is to be realized and sustained.
V. Figures
A. NIMH Research and Training Grants, FY 1989–2000, by Number of Grants
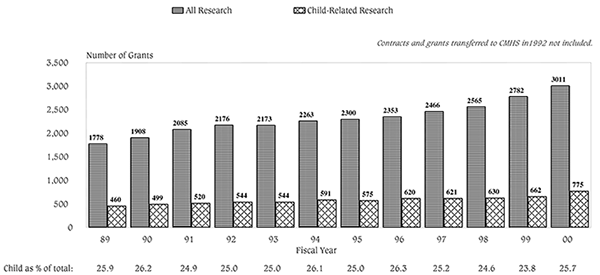
B. NIMH Research and Training Grants, FY 1989–2000, by Awarded Amount
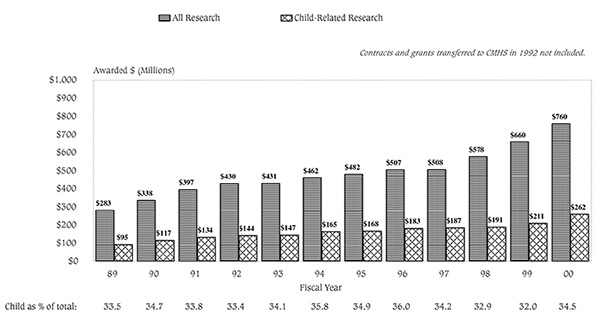
C. NIMH Child Training Grants, FY 1989–2000
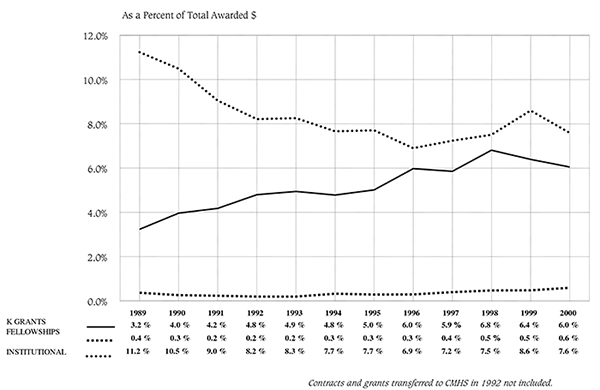
D. NIMH Training Grants, FY 1989–2000
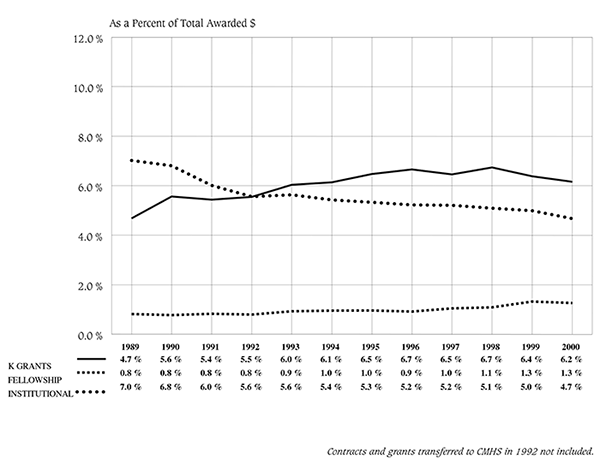
VI. Appendices
Research Center on Managed Care for Psychiatric Disorders
A Joint Program of the UCLA Neuropsychiatric Institute and RAND
National Estimates of Mental Health Utilization and Expenditures for Children in 1998
Roland Sturm, Jeanne Ringel, Catherine Bao, Bradley Stein, Kanika Kapur, Winnie Zhang, Feng Zeng
November 2000
Working Paper No. 205

Funded by the National Institute of Mental Health
Appendix A
National Estimates of Mental Health Utilization and Expenditures for Children in 1998
Executive Summary
This report provides updated utilization and expenditure estimates for mental health treatment provided to children and adolescents. It addresses the following questions:
- How many children and adolescents are using services?
- How does utilization differ by insurance status?
- How much was spent in 1998 on mental health treatment for children and adolescents?
- How were mental health expenditures distributed by type of service and child insurance status?
The report focuses on service utilization and associated expenditures and does not include any estimates of indirect costs, such as burden on family members or society.
Key Findings
- Based on three national surveys fielded between 1996 and 1998, between 5 percent and 7 percent of all children use any mental health specialty services in a year. This average rate is similar to the rate among adults, but it obscures major differences across age groups. Only 1 percent to 2 percent of preschoolers use any services, but 6 percent to 8 percent of the 6-to-11 age group and 8 percent to 9 percent of the 12-to-17 age group do.
- There is substantial variation in mental health service utilization by type of insurance, ranging from 8.4 percent for Medicaid enrollees to 4.0 percent for the uninsured. The intensity of outpatient care (number of visits) differs similarly. Children on Medicaid are estimated to have more than 1,300 specialty visits per 1,000 children per year, compared with 462 specialty visits per 1,000 children with private insurance, 391 visits per 1,000 children with other types of insurance, and 366 visits per 1,000 children with no insurance.
- Mental health utilization varies across racial/ethnic groups. Latinos are the least likely of all groups to access specialty care (5.0%), even though they and Black children have the highest rates of need (10.5%) based on measures in the National Health Interview Survey (NHIS). Approximately 7 percent of families with a child with need (based on NHIS measures) claimed financial barriers as the reason for not getting any mental health care.
- More than half of all outpatient specialty mental health services provided to children with private insurance are out-of-plan. The education sector likely provides a substantial portion of these services.
- Regarding inpatient mental health care, between 0.2 percent and 0.3 percent of children aged 1 to 17 use inpatient mental health services in community hospitals. This rate is much lower than the rate for adults (0.6%). Across all insurance types, adults and adolescents have greater inpatient days per 1,000 population than young children. Among the privately insured and the uninsured, adolescents have higher inpatient service use than adults. In contrast, among the publicly insured, inpatient days per 1,000 population are significantly higher for adults than for adolescents.
- Approximately 4.3 percent of children received psychotropic medication, and utilization is concentrated among older children: 5.0 percent of 6- to 11-year-olds and 5.6 percent of adolescents are on psychotropic medication, while only 0.7 percent of children ages 1 to 5 used such medication.
- Total treatment expenditures for children in 1998 are estimated to be approximately $11.75 billion, or about $173 per child. Adolescents (12 to 17) account for 59 percent of the total and also have the highest expenditures per child at $291; children 6 to 11 account for 34 percent of the total at $165 per child; children 1 to 5 for 7 percent at $39 per child.
- Across service types, outpatient services account for 57 percent of the total ($6.7 billion), inpatient for 33 percent ($3.9 billion), psychotropic medications for 9 percent ($1.1 billion), and other services for 1 percent ($0.07 billion).
- Across children’s insurance status, children with private insurance account for 47 percent ($5.5 billion), Medicaid enrollees for 24 percent ($2.8 billion), children with other public insurance for 3 percent ($0.4 billion), and the uninsured for 5 percent ($0.6 billion). We could not allocate State/local expenditures (21%, or $2.5 billion) by child insurance status. The majority of these services were provided to children with private insurance coverage or Medicaid, but they were not paid by insurance.
- Total expenditures on psychotropic medications for children in 1998 are estimated to be $1.1 billion. The largest proportion of expenditures was for stimulants, which accounted for slightly over 40 percent of the total. Antidepressant costs were the second largest category, accounting for 33 percent of the total.
Introduction
Over the course of a year, approximately 20 percent of children and adolescents meet criteria for a mental disorder diagnosis, and half of these youth also have significant functional impairment (U.S. Department of Health and Human Services, 1999). Thus, mental health services for children and adolescents should be a significant component of health care. Expenditures for the full population have been estimated repeatedly (Coffey et al., 2000; Mark et al. 2000; Mark et al., 1998; Rice et al., 1990; Frank & Kamlet, 1985), but no recent national data about utilization of services or about financing and expenditures for mental health care for children are available (Hoagwood and Rupp, 1994). The most recent available expenditure estimates were for 1986, and they were in the range of $3.5 billion (OTA, 1991; Burns, 1991).
This report provides an update of previous work in an effort to answer the following questions:
- How many children and adolescents are using services?
- How does utilization differ by insurance status?
- How much was spent in 1998 on mental health treatment for children and adolescents?
- How were mental health expenditures distributed by type of child insurance status?
Several factors help to explain the absence of national estimates of child/adolescent mental health care utilization and expenditures. First, the low prevalence rates of child mental health use requires very large data sets to obtain the necessary number of patients (or visits or days) for precise estimates. Second, national cost data that use a top-down approach by collecting data from more aggregate units (hospitals, providers, pharmacies) rather than at the individual patient level do not have the age-specific information to subset overall estimates for children (Institute of Medicine, 1989). Finally, the continuing fragmentation in the way child mental health services are delivered, as well as definitional and diagnostic inconsistencies, make comprehensive estimates difficult to obtain (Hoagwood and Rupp, 1994). In addition to private insurance and public treatment settings, some mental health services are delivered and paid for by the education, child welfare, and juvenile justice sectors. Social services are major sources of services for children but are not part of the National Health Accounts (NHA), the best known summary of annual health care costs (http://www.hcfa.gov/stats/NHE-Proj/ ; Levit et al., 2000).
The 1986 Office of Technology Assessment (OTA) report on Children’s Mental Health Problems and Services conjectured that “federal and private sources currently bear less of a burden” but warned that there are no data to support a firm conclusion: “In the case of Medicaid, for example, the only mental health expenditure known is that of mental hospitals. Private third-party payers prefer not to disclose what they pay for mental health services and the amount actually spent by clients themselves is not known. The proportion of costs specifically for children’s mental health treatment is even more difficult to determine” (p. 132).
A later OTA report on adolescents (1991) provided utilization estimates for specific services based on several different databases (National Ambulatory Care Survey, National Health Interview Survey, Inventory of Mental Health Organization, some secondary sources) but cautioned that “these estimates from varying sources do not allow an overall estimate of mental health services utilization by adolescents” (p.457). An unpublished background paper by Burns, Taube, and Taube cited in the report gave total estimates for U.S. adolescents in 1986 at $3.5 billion (see also Burns, 1991). Of this, 46 percent was attributed to hospital inpatient care, 28 percent to residential treatment centers, and 26 percent to outpatient care.
Background on Health Spending and Utilization Estimates
Since 1964, the U.S. Department of Health and Human Services has published an annual series of statistics presenting total national health expenditures during each year. The aim of these National Health Accounts (NHAs) is to identify all goods and services that can be characterized as relating to health care in the nation and determine the amount of money used for the purchase of these goods and services. The NHA framework is a matrix of operational categories classifying sources of health care dollars and services purchased with these funds (HCFA, various years). The NHA recognize several types of spending, including “personal health care,” “government public health activity,” “program administration,” and “research and construction.” In 1997, national health expenditures were estimated at $1,092.4 billion (13.5% of GDP and $3927 per capita) and expected to grow to $1,316.2 billion (14.3% of GDP and 4,611 per capita) by 2000. Most of the expenditures are for personal health care, broken down by type of expenditure and payer. For the purposes of this project, we are concerned only with personal health care, not the other categories, even if they relate to child mental health, such as NIMH funded research. The NHA collects information primarily from larger reporting units (e.g., hospitals) instead of trying to aggregate individual service or patient information. The NHA contains no information about health care utilization (e.g., number of physician visits or hospital days) for specific patient groups.
An ongoing project funded by the Substance Abuse and Mental Health Services Administration (SAMHSA) provides national estimates for mental health and substance abuse expenditures (Mark et al., 1998; Coffey et al., 2000). The project builds on earlier work by Frank and Kamlet (1985), Rice et al. (1990), and others but refines the methodology. The SAMHSA project uses an indirect approach that starts with aggregate NHA estimates as the basis for the general health care sector and carves out of the NHA estimates the share of mental health expenditures. The authors then add expenditures for specialty facilities from the Inventory of Mental Health Organizations (IMHO) and the Uniform Facility Data Set (UFDS). The IMHO and UFDS surveys are answered by facility administrators and report statistics at the aggregate facility level. No patient-level or service-level data are available from these surveys. Including specialty providers that were not captured in the NHA, the 1997 expenditure estimate was $85.3 billion, of which $73.4 billion (86%) was for treatment of mental health (MH) disorders and $11.9 billion (14%) for treatment of substance abuse (SA) (Coffey et al., 2000). NHA-equivalent MH/SA expenditures were about $3 billion less ($82.2 billion) in 1997. According to this approach, MH/SA expenditures represented about 7.8 percent of all U.S. health care expenditures in 1997, or 8.5 percent of personal health expenditures.
Most closely related to the current project in terms of goal and scope are two OTA reports: the 1986 report on Children’s Mental Health Problems and Services and the 1991 report on adolescents. The basis of utilization and expenditure estimates in the latter report was an unpublished background paper by Burns, Taube, and Taube, which gave total estimates for U.S. adolescents in 1986 at $3.5 billion. Of this, 46 percent was attributed to hospital inpatient care, 28 percent to residential treatment centers, and 26 percent to outpatient care. The estimates were based on several different databases (National Ambulatory Care Survey, National Health Interview Survey, Inventory of Mental Health Organization, some secondary sources), and the report cautioned that “these estimates from varying sources do not allow an overall estimate of mental health services utilization by adolescents” (p.457). A major difficulty in calculating national estimates of mental health service utilization and cost for children is determining which mental health services are provided in non-mental-health contexts, such as the educational, child welfare, and the juvenile justice systems. A top-down or indirect approach is difficult to implement because mental health services account for only a very small part of the resources in those sectors, and no national (and sometimes not even regional/local) data have measured individual services that would allow one to break out mental health expenditures. For example, even though education statistics provide expenditures on special education for children with serious emotional disturbances (SED) separately, one cannot include those numbers as mental health expenditures. The costs are made up of at least three components. First, there are the basic education costs that would be incurred if the child were not SED. Second, there are the higher educational costs per SED student not related to mental health treatment (such as increased costs incurred by having higher teacher-to-student ratios in special education classes). These costs could be considered part of the social costs of mental illness but not direct mental health care expenditures. Finally, there are the direct costs of providing mental health treatment services through the school. The sum of the latter two could be roughly estimated as the excess expenditures for special education over regular education, and we provide an estimate of this, but it is not possible to estimate the share of direct mental health services from such aggregate data. Similar considerations apply to the other sectors, primarily juvenile justice and child welfare. We are not aware of any study of national scope for those sectors. However, the National Survey of Child and Adolescent Well-Being, which is currently in the field, may provide such estimates for child welfare in the future.
For adults, several national or large multisite studies have been conducted that provide information on utilization of mental health services, including the Epidemiologic Catchment Area Program (ECA), the National Comorbidity Study (NCS), the Medical Outcomes Study (MOS), and HealthCare for Communities (HCC). The first wave of the HCC study, fielded in 1997–1998, is the most recent national data set currently available for public use (Sturm et al., 1999); a second wave is being fielded in 2000. Results from that survey found that the probability of a psychiatric disorder (measured by the Composite International Diagnostic Instrument (CIDI) screening items) was highest among Medicaid eligibles (nearly 41%), followed by the uninsured (22%), those with private insurance (12 to 13%), and elderly Medicare recipients (7.8%) (Wells et al., 2000). The probability of specialty mental health or substance abuse care in 1998 exhibited a similar pattern and ranged from 14 percent in Medicaid to about 5 percent among the privately insured and uninsured and 1 percent among Medicare recipients. However, the percentage that had contact with a primary care physician and discussed mental health issues or received treatment in that sector was much larger.
There have been no equivalent results to date on child mental health utilization. The NIMH Methods for the Epidemiology of Child and Adolescent Mental Disorders (MECA) study is the only multisite community study that has assessed mental health status and utilization among youths. It studied children and adolescents ages 9 through 17 years at four sites in 1992 (Leaf et al., 1996; Glied et al., 1997). The sites were not randomly selected or chosen for national representativeness (comparable to the ECA, but in contrast to the NCS and HCC, which were designed for national estimates), and the sample size was too small to assess detailed utilization patterns. The MECA study had fewer than 1,500 respondents at four sites, whereas the NCS and HCC had around 10,000 geographically dispersed respondents. The Great Smoky Mountains Study of Youth (GSMS) is another population-based community survey with around 1,000 children, but it is a regional sample (Burns et al., 1995, 1997; Farmer et al., 1999). These two studies (GSMS and MECA), however, appear to be the most representative estimates for child/adolescent mental health utilization that are currently available. The main results of these studies are summarized in table 1.
A further complication in the estimation of mental health utilization and costs for children is that a small number of individuals tend to account for a large proportion of costs. Children with particularly high needs and costs are in out-of-home placements, in foster care, or on probation. No national or multisite cost and utilization data are available, although results from two State case studies suggest that the higher costs of treatment for children in foster care are driven by higher rates of any use rather than by higher costs per user. The latest data, for 1995–1996 in California, indicate that 31 percent of children in foster care use mental health services, and the average expenditure is $1,864 per user (Libby, Rosenblatt, & Snowden 1999). Halfon et al. (1992a, 1992b) analyzed California Medicaid data from 1988 and found that although foster children accounted for less than 4 percent of enrollment, they accounted for over 40 percent of mental health service users and over 50 percent of all mental health outpatient visits or mental health hospital stays. The study reports that nearly 90 percent of adolescents in foster care used mental health services in 1988. Takayama et al. (1994) studied the use of mental health services by children in foster care in Washington State. The study focused on a younger population (children under age 8), and thus the utilization rate was somewhat lower than the estimates from Halfon et al. (1992a, 1992b). Utilization in this group, however, is still far higher than among other children on Medicaid (25% of children in foster care used mental health services in 1990, compared with 3% of other children in Medicaid). Adjusting for age group differences, the foster care utilization results from Washington State are similar to those of California (about 23% based on Halfon et al.’s numbers).
| Study | Population | Sample Size | Any MH Specialty Care | Inpatient Use | Outpatient Use | Intermediate Services | School-based | Social Service | Notes |
|---|---|---|---|---|---|---|---|---|---|
| Burns et al., 1997. Journal of Child and Family Studies 6(1): 89–111. | Public school youths in the GSMS ages 9, 11, and 13 followed over a 2-year period. | N=1,015 | Varies from 6.7% to 44.4% by insurance status and level of need. Including both inpatient and outpatient. |
Varies from .3% to 18.9% by insurance status and level of need. Including hospitals, residential treatment centers, detox units, group homes, and TFCs. |
Varies from 6.7% to 43.9% by insurance status and level of need. Including day hospitals, SA clinics, MH centers, and private MH professionals. |
N/A | Varies from 22% to 63% by insurance status and level of need. | N/A | Both MH and SA care during a 2-year period. Aggregate use data not available. |
| Burns et al., 1995. Health Affairs 14(3): 147–159. | Public school youths in the GSMS ages 9, 11, and 13 in 1992. | N=1,015 | 4.0% Inpatient + outpatient, same definition as in the study above. |
N/A | N/A | N/A Services received in the general medical sector: 16%* 12%=1.92% |
16% received some MH care, among which 70% to 80% seen by providers in the education sector: 16%*75%=12% | Child welfare: 1.2% to 16.4%; Juvenile justice: 0.5% to 4.3% by diagnostic groups. | First-wave data (1992–1993) and refers to the preceding 3 months. |
| Farmer et al., 1999. Community Mental Health Journal 35(1): 31–46. | Public school youths in the GSMS ages 9, 11, and 13 in 1992. | N=1,007 | Nearly 8% | 0.8% received out-of-home placement. | N/A | N/A | 12%, among which 95% received services from a school counselor. | Juvenile justice: 0.7% Child welfare: 1.4% Informal or nonprofessional sources: 4% |
Any use during the first year of the study. 21.1% received some type of service; general medical sector provided services to 4%. |
| Glied et al., 1997. Health Affairs 16(1): 167-174. |
MECA: Youths ages 9–17 in three U.S. communities in 1992 (the Puerto Rico sample was not included in this study). |
N=973 | Private ins: 0.6% Public ins: 1.5% No ins: 1.1% |
Offices of MH professionals and psychiatric OP departments: Private ins: 6.0% Public ins: 9.0% No ins: 6.5% Offices of general medical providers: Private ins: 3.2% Public ins: 3.0% No ins: 4.3% |
N/A | Private ins: 8.7% Public ins: 17.9% No ins: 12.9% |
Rate of any use: Private ins: 16.1% Public ins: 28.4% No ins: 20.4% Rate of any use during 1 year. Aggregate rate not available. |
||
| Leaf et al., 1996. Journal of the American Academy of Child and Adolescent Psychiatry 35(7): 889- 897. |
MECA: Youths ages 9–17 in four U.S. communities in 1992. |
N=1,285 | 8.1% | Not identified | Not identified | Not identified | 8.1% | Clergy: 1.2% Social services: 1.6% |
Unweighted rate of any use in 1 year, parent report; Rate of any MH use: 14.9% |
| Note: MH = mental health; OP = outpatient; SA = substance abuse; TFC = treatment foster care; N/A = not available. | |||||||||
| Study | Population | Sample size | Stimulant | Other Medication | School-based Care | Psychosocial Treatments |
|---|---|---|---|---|---|---|
| Angold et al., 2000. Journal of the American Academy of Child and Adolescent Psychiatry, 39(8): 975–984. | Children at 9, 11, and 13 years, from public schools in 11 counties in western North Carolina (the Great Smoky Mountains). | N=1,422; 4,964 annual observations over 4 waves. |
7.3%, at some point during the 4 years (average duration of treatment greater than 3 years; 7.3%*3/4=5.5%) |
N/A | N/A | N/A |
| Buck, 1997. Psychiatric Services, 48(1): 65–70. | Nondisabled children and adolescents under 19, continuously enrolled in Medicaid of Michigan and Tennessee in 1990 and with MH services, including SA treatment. |
N=16,544 in Michigan N=10,992 in Tennessee |
Michigan: 5%*1/3*64.0%=1.1% Tennessee:7%*1/4*36.1%=0.6% First number in the formula: percentage of the population using MH care; Second number: among those using MH care, proportion using prescription drug; Third number: distribution of prescription drug claims to stimulant |
Michigan: 5%*1/3*36.0%=0.6% Tennessee: 7%*1/4*63.9%=1.1% |
N/A | N/A |
| Jensen et al., 1999. Journal of the American Academy of Child and Adolescent Psychiatry, 3(7): 797–804. | Youths ages 9–17 in four U.S. communities; 12-month recall. | N=1,285 | 1.4% [0.9-2.3] | 1.1% [0.6-1.9] | 8.0% [6.6-9.7] | 9.9% [8.4-11.7] |
| LeFever et al., 1999. American Journal of Public Health, 89(9): 1359–1364. | Students in grades 2 through 5, enrolled in public schools in southeastern Virginia. | N=29,734 (N=5,767 in city A; N=23,967 in city B) |
City A: 8%*90%=7.2% City B: 10%*90%=9% Overall % weighted by sample size: 8.65% |
10% received another medication alone; 5% received with stimulant | N/A | N/A |
| Rappley et al., 1999. Archives of Pediatric and Adolescent Medicine, 153: 1039–1045. | Very young children (3 years old or younger) continuously enrolled in Michigan Medicaid for 15 months and with ADHD. | N=223 | Methylphenidate: 73/223=32.7% |
Clonidine: 48/223=21.5% 82.5% of the population received medication other than Methylphenidate. |
N/A | N/A |
| Safer et al., 2000. Pediatrics, 106(3): 533–539. | Maryland public school students (grades K-12); medication at the time of the survey. | N=816,465 | 2.46%+73%*0.46%=2.8% (Constituted 84% of all ADHD medication) K–5: 3.11% 6–8: 2.91% 9–12: 0.87% |
(1-73%)*0.46%=0.12% K–5: 0.55% 6–8: 0.57% 9–12: 0.19% |
N/A | N/A |
| Zito et al., 2000. Journal of the American Medical Association, 283(8): 1035–1050. | Preschoolers (ages 2–4 years) in two State Medicaid programs and a group-model HMO | Midwestern State Medicaid: 158,060; Mid-Atlantic State Medicaid: 54,237; Northwest HMO: 19,322 |
1995 data: 1.2% Children 2–4 treated at 1/10 the rate of their 5-14-year-old counterparts; largest gain in use seen in 15-19-year-old group. |
1995 data: Antidepressants: 0.32% Clonidine: 0.23% Neuroleptics: 0.09% For HMO: clonidine (0.19%) vs. antidepressants (0.07%) |
N/A | N /A |
| Zito et al., 1999. Archives of Pediatrics and Adolescent Medicine, 153: 1257–1263. | Children 5 to 14 years with office visits for ADHD | # of total youth visits from 1989 to 1996: N=20,013 N=3,315 in 1991 N=2,081 in 1996. Among the ADHD visits, 77% include a psychotherapy agent. |
Among the ADHD visits, visits with stimulant therapy only account for 77%*82.8%=63.8% | Among the ADHD visits, visits with one or more psychotherapies other than stimulant account for 77%*7.6%=5.9% visits with both stimulant and other account for 77%*9.6%=7.4% | N/A | N/A |
| Note: ADHD = attention deficit hyperactivity disorder; HMO = health maintenance organization; MH = mental health; SA = substance abuse; N/A = Not applicable. | ||||||
While the growth of managed care has changed utilization patterns for all types of services in the past two decades, nowhere have changes been more dramatic than in the use of psychotropic medication. This is likely due to the development of new, safer medications and to an increased willingness on the part of many physicians and parents to use psychotropic medications in children. For example, the proportion of outpatient psychiatric visits in which an antidepressant was prescribed more than doubled between 1985 and 1993 (Olfson et al., 1998). Table 2 summarizes results from the latest published studies on psychotropic drug use in children (some of the entries in the table are based on calculations by the authors of this report). Some studies are more recent than the MECA study and have larger sample sizes (such as Medicaid data). Unfortunately, the most recent studies are local or regional in scope and the wide variation across studies suggests very large regional variations that limit the generalizability of single-site data. The exception is the study by Zito et al. (1999) based on the National Ambulatory Medical Care Survey (NAMCS), but the design of the NAMCS (a sample of visits to physicians) is so different that it is difficult to compare results with those from other community studies. Besides, the populations studied vary in age, type of school attended, or type of health insurance plan.
Methods
The two goals of this study are
- To provide more recent estimates of mental health utilization patterns for children and adolescents and the relationship to insurance status and ethnicity.
- To obtain an overall estimate of all the resources available for child mental health by aggregating all expenditures by all types of services/providers and payers. Payment sources include out-of-pocket payments, private insurance, Medicaid, other State/local resources, and other Federal payments (primary block grants), as well as resources that are not usually included as part of the health system, such as counselors in schools.
Whenever possible, we provide estimates for preschoolers (ages 1 to 5), children (6 to 11), and adolescents (12 to 17). We do not consider children under the age of 1, because the diagnosis and treatment of mental health disorders in infants remains ill-defined and controversial.
Data Sources
Table 3 summarizes the sources of data we used. We tried to obtain 1998 data where possible. When only earlier data sets were available, we adjusted dollar numbers for inflation and corrected for changes in the population but made no adjustment for possible changes in utilization patterns. To obtain overall estimates of users and for details on differences in access among the noninstitutionalized household population and insurance status, we used the 1997 National Survey of American Families (NSAF), the 1996/1997 Community Tracking Study (CTS), and the 1998 National Health Interview Survey (NHIS). The NSAF also has items on intensity of care (number of contacts with a provider) and provides a sample of 1,700 child/adolescent users, which is more than twice the size of the NHIS and three times the size of the CTS. The NSAF, however, was fielded primarily in 13 States. In contrast, the CTS has national coverage, although it is concentrated at 60 sites. The NHIS is the most recent survey (by 1 year), but insurance information has not yet been released. Although 1996 Medical Expenditure Panel Survey (MEPS) provides more detailed cost data, it also is the smallest and oldest of those surveys. In fact, it is smaller than the NHIS by design as the MEPS surveys a subset of NHIS participants (from earlier NHIS rounds). None of these studies are large enough to estimate residential or inpatient costs precisely and do not assess them.
| Data Source | Description of Data Source | Most Recent Year of Data Source |
|---|---|---|
| National Survey of American Families (NSAF) | Household survey with 34,390 children and adolescents. Question on mental health use and intensity. | 1997 |
| Community Tracking Study (CTS) | Household survey with 10,646 children and adolescents. | 1996/1997 |
| National Health Interview Survey (NHIS) | Sampling frame for other surveys (MEPS). 14,390 children and adolescents. Contains screening version of the Child Behavior Check List. | 1998 (without insurance information) |
| Medical Expenditure Panel Survey (MEPS) | Nationally representative survey of health care use, expenditures, sources of payment, and insurance coverage for the U.S. civilian noninstitutionalized population. | 1996 |
| Ingenix | A proprietary database compiled by Ingenix, this is one of the largest single sources of private health insurance claims available for analysis. We use claims for about 1.5 million employees and dependents with private insurance, including mental health, pharmacy, and medical claims. | 1998 |
| United Behavioral Health Survey (UBH) | Proprietary data, largest claims database, but only managed mental health specialty care. | 1998 |
| Health Care Financing Administration (HCFA) Medicaid Statistics | HCFA statistics on health care utilization, most detailed summaries available for 10 States in 1993 (CMHS reports, Buck et al., 2000). Additional tables for Michigan and California for 1992 (Wright et al., 1995). | 1993 |
| National Hospital Discharge Survey (NHDS) | A nationally representative sample of hospitals and discharges, collected by the National Center for Health Statistics (NCHS). Data are for non-Federal, short-stay, and general hospitals in the U.S. and include about 300,000 of the 30,000,000 U.S. discharges per year. | 1997 |
| Healthcare Cost and Utilization Project, Nationwide Inpatient Sample (HCUP-NIS) | Hospital discharge data from 900 hospitals in 20 States. | 1997 |
| National Ambulatory Medical Care Survey (NAMCS) | NCHS national probability survey of visits to office-based physicians in the U.S. Drugs prescribed during the visit are included. | 1997 |
| National Hospital Ambulatory Medical Care Survey (NHAMCS) | NCHS national probability survey of visits to hospital emergency and outpatient departments in U.S. non-Federal, short-stay, and general hospitals. | 1992–1997 |
| Inventory of Mental Health Organizations (IMHO) | Substance Abuse and Mental Health Services Administration (SAMHSA) survey of mental health facilities. | 1994 |
| Education | Department of Education statistics (special education), Los Angeles Unified School District (mental health expenditures by type of provider and payment source). | 1998 |
The NSAF, CTS, and NHIS differ slightly in the questions asked (table 4). The CTS and NHIS use the same mental health utilization question, except that the CTS refers to the child talking to an MH specialist and the NHIS refers to the parent talking to an MH specialist about the child. Since some settings, especially counseling at schools, do not always involve the parent, we expect the NHIS estimates to be lower than the CTS estimates, except for the smallest children. The methods effect of the NSAF versus CTS question is less clear. The NSAF includes a broader range of providers, and “doctor” could be understood to include primary care providers, not just psychiatrists. This would suggest a higher estimate of any use in the NSAF. On the other hand, the NSAF wording about “receiving services” may suggest more active treatment to respondents than “seeing or talking” and, therefore, may lead to lower estimates. Another difference is that the NSAF asked for a specific number, not just yes or no. We also tested whether regional variations could account for differences in the estimates, but the CTS estimates remained unchanged when subset to the States in the NSAF.
It is important to note that relying on survey data for outpatient utilization is not without problems. In all three surveys, parents provide all the information about the child. Recent studies have found reporting errors and recall biases, such as telescoping and heaping when parents reported their children’s utilization (Bruijnzeels et al., 1998). Mathiowetz and Dipko (2000) examine differences in reporting biases between adults and adolescents and find that parents tend to underestimate their children’s utilization while adolescents tend to overreport use. Given these findings, the utilization rates from the NSAF, CTS, and NHIS may underestimate total mental health service use among children.
| Survey | Questions |
|---|---|
| NSAF | During the past 12 months, how many times has [child] received mental health services, including mental health services received from a doctor, mental health counselor, or therapist (do not include treatment for substance abuse or smoking cessation). Valid range: 0 to 500 |
| CTS | During the past 12 months, has [child] seen or talked to a mental health professional, such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker? |
| NHIS | During the past 12 months, have you seen or talked to any of the following health care providers about [child’s] health? A mental health professional such as a psychiatrist, psychologist, psychiatric nurse, or clinical social worker? |
The 1997 NAMCS/NHAMCS provide two other data sets for outpatient care. Unfortunately, the NAMCS/NHAMCS data are quite small. The most recent NAMCS only includes about 4,000 physician visits for children/adolescents, and only about 3 percent of those had a mental health diagnosis. The unit of observation in the NAMCS is a visit, and it is not possible to estimate number of users or visits per user, which makes the NAMCS somewhat less useful than other survey data to assess utilization patterns. Although the earlier releases have been used in previous studies of mental health use (Zito et al. 1998; Olfson et al., 1998, 1999), we note that estimates relying on the NAMCS/NHAMCS result in a substantially lower number of mental health visits than estimates based on any other data set. A main reason is that the NAMCS only includes nonfederally employed office-based physicians primarily engaged in direct patient care. However, non-MD mental health specialists account for most psychotherapy and counseling. A recent study of managed behavioral health plans found that Ph.D. psychologists (33.4%) accounted for most mental health claims in 1996, followed by psychiatrists (30.5%), social workers (19.8%) and other master’s-level therapists (13.8%) (Sturm & Klap, 1999).
The Healthcare Cost and Utilization Project (HCUP) and the National Hospital Discharge Survey (NHDS) are the main data sources for national information on inpatient utilization. One important limitation is that NHDS excludes hospitals with an average length of stay of more than 30 days, Federal hospitals, and hospital units of institutions (such as prison hospitals). These settings are not included in the HCUP-NIS either but are included in some of the HCUP State data.
The Ingenix database provides a cross-section of private insurance plans, similar to the MedStat data used in the SAMHSA studies by Coffey et al. (2000) and Mark et al. (1998). Neither one is designed as a nationally representative sample; they primarily reflect the clients of Ingenix or MedStat. Nevertheless, these two databases are the only available data sources for research that provide comprehensive data on utilization and costs for large privately insured populations under a cross-section of insurance plans. We also use the Ingenix database to estimate expenditures per service unit, and it is the source for studying the use of medications among children and adolescents.
For Medicaid, CMHS has compiled detailed tables on mental health utilization for 10 States (Buck et al., 2000). Those data are already somewhat older (1993), and the States were not necessarily representative because they had a larger share of traditional indemnity insurance than other States (Buck, personal communication). Wright et al. provide similar numbers for California and Michigan for 1992. Other than 1998 data on mental health service utilization in Medicaid managed care programs for counties in the State of Washington, we could not obtain more recent data. Relying on those older utilization estimates for Medicaid is a limitation of this study, but new data analysis on those complex data sets was outside the scope of this project.
Important other sectors that provide mental health services to children include education, child welfare, and juvenile justice. There are no national data sets available to estimate mental health services delivered in these sectors, and we therefore have to combine estimates from the literature or use specific regional data sets. For the educational system, we obtained data from the Los Angeles County Office of Education. While regional data are not likely to be nationally representative, they will provide some insight into the extent of mental health services provided for children in schools.
Calculation of Mental Health Expenditures
In this project, we consider only services provided by health and mental health professionals to treat mental illness, not other social expenditures. Broader types of services in the general population—such as testing and supportive services to patients or their families (special education)—that are related to mental health are excluded. We also exclude indirect costs associated with mental health disorders (such as future lost wages as a consequence of worse educational outcomes) or comorbid health costs (for example, injuries related to suicide attempts or other trauma). Such potential costs would be part of the social cost of illness.
Two general approaches can be used to estimate the costs of children’s mental health service use. The first approach is direct and associates expenditures with estimated utilization patterns, aggregating to national expenditures from the bottom up. The advantage of this approach is its consistency with the reported utilization data. This is our preferred approach in this project. A second approach is indirect; it starts with aggregated data and uses micro-information to carve out individual pieces. This indirect, top-down approach, which calibrates estimates against NHA, is particularly useful for comparisons with other reports that use a similar approach, such as Coffey et al. (2000). As a sensitivity analysis, we try to replicate the SAMHSA approach by comparing utilization patterns for mental health care for children versus adults to derive weights and applying them to the numbers reported by Coffey et al. (2000).
It is important to keep in mind that all approaches are conventions that have different advantages and shortcomings. The direct approach may omit services for which no data are collected and is therefore more likely to be biased downward; the indirect approach, which tries to separate a larger conceptual piece into specific categories, may misattribute expenditures and can be biased upward if the separation does not account for all the components that went into the aggregate. The direct approach becomes more advantageous with narrowly defined target estimates (e.g., insurance payments to psychiatrists for child mental health services). All methods approximate a theoretical concept of health spending differently, but none can capture it unambiguously, even if there is agreement on what to include under “mental health” expenditures.
The Direct, Bottom-Up Approach
Expenditures on mental health services are calculated for each category of insurance coverage that children have: private, Medicaid, other public, and none. Total mental health expenditures (including insurance and patient copayment) are calculated for the different categories of services, such as outpatient care, inpatient care, and psychotropic medications. Totals from each category are summed to get total mental health expenditures. To estimate the number of children in the United States with each category of health insurance, we use a weighted average of estimates from the Community Tracking Study (CTS) and the National Survey of American Families (NSAF). Both surveys are nationally representative and go to great lengths to determine the health insurance status of survey respondents and provide mutually exclusive point-in-time categories. However, they include only children in the community, so we must adjust for institutionalized children using other data sources, primarily from payers (Medicaid and State mental health agencies).
For privately insured children, we use the average cost per mental health visit estimated from the Ingenix data, combined with estimates of the number of visits per user from the NSAF, to estimate outpatient expenditures. For expenditures on inpatient services, we use a combination of data from the IMHO and the HCUP. The IMHO captures inpatient stays in psychiatric hospitals, while the HCUP is used to estimate the costs of inpatient stays in community hospitals. In our calculations from the HCUP, we use cost/charge ratios from the Agency for Healthcare Research and Quality (AHRQ) to deflate charges reported on the hospital discharge records. Expenditures on psychotropic medications and other mental health services are calculated using estimates from the Ingenix data on costs per member per year for each category.
No public agency or insurance company maintains a large database on the use of health care services by the uninsured. Thus, some assumptions about the patterns of mental health services use for the uninsured must be made. We assume that cost per service unit is the same for the uninsured and the privately insured and that the two groups differ in the percentage of any use and the number of visits per user. Estimates of expenditures on inpatient mental health service are taken from HCUP. For psychotropic medication, we assume the same costs per user for the uninsured and the privately insured but adjust for the lower probability of any use among the uninsured.
A recent CMHS publication, Mental Health and Substance Abuse Services in Medicaid, 1993 (Buck et al., 2000), has information on Medicaid mental health service utilization in 10 States: Delaware, Georgia, Kentucky, Maine, Missouri, Tennessee, Utah, Vermont, Washington, and Wisconsin. We use the results from those 10 States as representative of all children enrolled in Medicaid in the United States and assume that utilization patterns remain constant between 1993 and 1998. Additionally, we have been unable to develop an adjustment for differences in utilization across managed care and fee-for-service programs and assume that utilization across the two types of programs is comparable. Thus, the only adjustments to the tables published in Buck et al. (2000) are for changes in Medicaid enrollment by age group and for inflation between 1993 and 1998. The Medicaid spending estimates must be interpreted with the limitations of the available data in mind.
A relatively small group of children (approximately 3%) have insurance through public programs other than Medicaid. These “other public” programs vary widely across cities and States. To estimate the costs of mental health services obtained by children in these other public programs, we assume that the utilization patterns are the same as among children in Medicaid.
Expenditures by State mental health agencies and other State and local payers on children’s mental health service utilization are largely outside the categories mentioned so far. This includes all non-community hospitals (excluded from HCUP) and residential treatment centers for children. Unfortunately, no patient/encounter-level data are available and we therefore need to deviate from our general approach to capture this sector. We use data from the IMHO to estimate the expenditures made by State and local governments (excluding Medicaid). As a comparison, we obtained State-level expenditure data for children obtained from the National Association of State Mental Health Program Directors (NASMHPD). The NASMHPD numbers are fairly consistent with our estimates based on IMHO (within 10%). This approach may lead to a small amount of double counting if services used by some of the privately insured children and the uninsured children are paid for by State agencies. This would be primarily for outpatient services that we have calculated based on NSAF/CTS, which we expect to be very small.
Mental Health Expenditures in the Education Sector
While there is wide agreement that the education sector is an important provider of mental health services for children, there are no comprehensive national data on the amount of money spent providing such services. Given the paucity of national data, we have looked to other sources. We have obtained data from the Los Angeles County Office of Education regarding expenditures on services provided by mental health professionals working in the schools, but we caution that Los Angeles County is unlikely to be representative. To provide additional information on the extent of expenditures for mental health services in the education sector we use estimates taken from the literature on the excess cost of educating children designated as having a serious emotional disturbance (SED).
The Top-Down Approach
Coffey et al. (2000) estimated that $73.4 billion was spent on mental health services in 1997 (see also Mark et al., 2000). The top-down approach to estimating total expenditures on mental health for children uses micro-level information to allocate the total expenditures between children and adults. We estimate children’s (versus adults’) share of expenditures for each major category of mental health services: outpatient, inpatient, and prescription drugs. For outpatient visits, we use the children’s share of total mental health outpatient visits estimated from NSAF and CTS; inpatient expenditures are allocated according to HCUP estimates; psychotropic expenditures are based on Ingenix. The expenditures on residential treatment centers for children from Coffey et al. are fully attributed to children.
Limitations
Estimating how much is spent on child/adolescent mental health care is a very complex project and requires aggregating across data sources that are not necessarily comparable. Several important pieces of data rely on regional or State information that is not necessarily nationally representative, and other crucial data sources are older than desirable, in particular IMHO and the Medicaid data summary published by SAMHSA (Buck et al., 2000). Unfortunately, running new analyses even on only a few selected Medicaid databases was not possible in the scope of this project. Other limitations are well known and not unique to this study. For example, underreporting of MH diagnoses in health care claims may be due to differential coverage for mental health or to concern about stigma. Claims data may underestimate out-of-pocket spending when there are no claims because of limits in insurance coverage.
One of the biggest problems is the fragmentation of mental health delivery. Individual survey data are more likely than administrative claims data to capture the full range of services. Our attribution by a child’s health insurance status, however, will misclassify such services if they are paid for by nonhealth sectors (for example, publicly paid services received by children with private insurance are allocated to private insurance).
To see the complexity of trying to build up expenditures using individual payment sources—and the holes in these estimates—consider the following table, which shows the type of non-Federal funding sources in sites that participated in the Comprehensive Community Mental Health Services for Children and Their Families Program. That program was established by Congress in 1992 as a demonstration program that reorganizes child mental health services into true “systems” of care. Of course, these programs include more than just the direct mental health services that are the scope of this report, and most of the funding sources are very minor. Nevertheless, the table highlights the impossibility of collecting data from all potential sources and suggests that relying on survey data will remain essential for future work that assesses mental health services more broadly. The existing national survey data are limited in their scope and are used in this study only for direct mental health services. Assessing broader social services would require different survey instruments.
| Source | System | Description |
|---|---|---|
| State | Mental health | General fund; Medicaid; Federal mental health block grant |
| Child welfare | Title IV-B (family preservation); Title IV-B (foster care services); Title IV-E (adoption assistance, training, administration) | |
| Juvenile justice | Federal funds for juvenile justice prevention; State appropriations | |
| Education | Special education; general education; training and technical assistance; in-kind staff resources | |
| Governor’s office/cabinet | Special children’s initiatives, often including interagency blended funding | |
| Social services | Title XX funds and realigned welfare funds Temporary Assistance for Needy Families (TANF) | |
| Bureau of children with special needs | Title V Federal funds and State resources | |
| Health department | State funds | |
| Public universities | In-kind support | |
| Department of children | In States where child mental health services are responsibility of child agency | |
| Vocational rehabilitation | Federal and State-supported employment funds | |
| Housing | Various sources | |
| Local | County, city, or local township | General fund |
| Social services/child welfare | Locally controlled funds | |
| Juvenile justice | Courts; probation department and community corrections | |
| Education | Local schools (including in-kind donations of staff time); school district | |
| County | Tax for specific purposes | |
| Food programs | In-kind donations | |
| Health | Local health-authority-controlled resources | |
| Substance abuse | In-kind support | |
| Private | Third-party reimbursement | Private insurance and family fees |
| Local businesses | Donations and in-kind support | |
| Foundations | Grants | |
| Charities | Faith organizations, homeless programs, and food | |
| Family organization | In-kind support | |
| Source: Koyanagi C, Feres-Merchant D. (2000). For the long haul: Maintaining systems of care beyond the federal investment. Systems of Care: Promising Practices in Children’s Mental Health, 2000 Series, Volume III. Washington, DC: Center for Effective Collaboration and Practice, American Institutes for Research. | ||
New Estimates of Service Utilization From Micro-Level Data
This section provides new results from databases that have only recently become available. These utilization results are the foundation of the direct cost estimates. Only our new analysis results are shown here, not components for which we relied on earlier studies or secondary sources (Medicaid, other State/local expenditures, education, welfare).
Use of Any Services
Based on three national surveys fielded between 1996 and 1998, between 5 percent and 7 percent of all children use any mental health specialty services in a year. This average rate is similar to the rate among adults, but it obscures the major differences across age groups. Only 1 percent to 2 percent of preschoolers use any services, but the rate is 6 percent to 8 percent for the 6–11 age group, and 8 percent to 9 percent for the 12–17 age group (see Figure 1). Survey information differs from claims data in that it captures out-of-plan use, which is particularly important because it is widely believed that school-based services are a major component of child mental health care (Burns et al., 1995).
Figure 1: Access to Specialty Mental Health Services
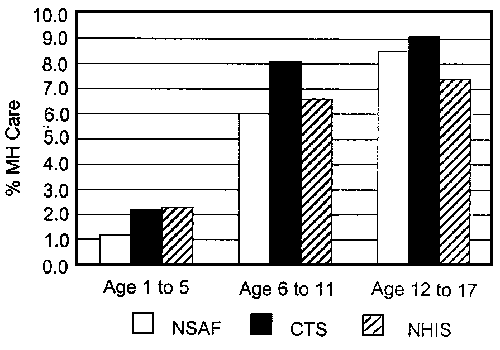
Calculations based on data from the National Survey of American Families (NSAF), the Community Tracking Study (CTS), and the National Health Interview Study (NHIS).
As expected, there is a substantial variation in rates of any mental health service use by type of insurance. Children in Medicaid are most likely to receive mental health services, and children without insurance are least likely. The utilization rates are roughly 1 percentage point higher than the mental health specialty rates for comparable age/insurance groups based on the 1992 MECA sample (Glied et al., 1997). While this could indicate an increase in the percentage of children accessing mental health services, it is not strong evidence of such an increase. The MECA study is based on a small sample size at a limited number of sites; thus, the results are not necessarily generalizable to the national level. Unfortunately, none of the surveys collects information about the source of care.
Also noticeable is the variation across ethnic groups. Black and Latino children have lower rates of any service use, and those differences increase when adjusting for insurance status.
Figure 2: Insurance Differences in Access to Specialty Mental Health Services
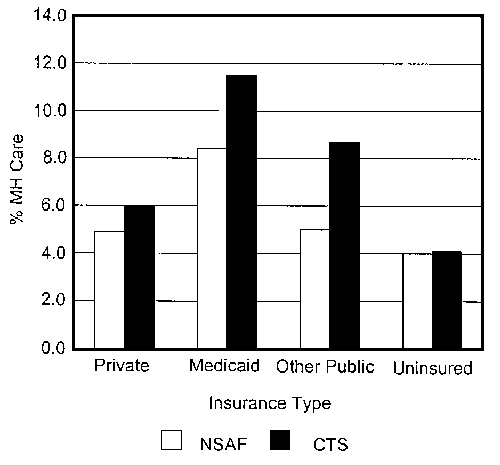
Calculations based on data from the National Survey of American Families (NSAF) and the Community Tracking Study (CTS).
Figure 3: Ethnic Disparities in Access to Specialty Mental Health Services
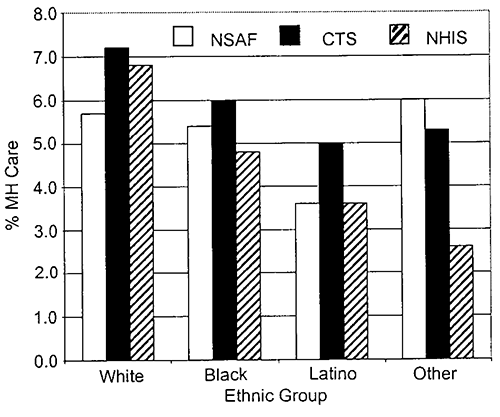
Calculations based on data from the National Survey of American Families (NSAF), the Community Tracking Study (CTS), and the National Health Interview Study (NHIS).
Results from the NHIS and NSAF indicate that the majority of children who are likely to benefit from mental health care do not receive any. The index of mental health need in the NHIS ranges from 0 to 8 and is based on four questions from the Child Behavior Check List (CBCL). Based on NHIS, 9.2 percent of the children had a need for mental health care, ranging from 4.4 percent among preschoolers to 11.0 percent among adolescents. Black and Hispanic children display higher need (10.5%) compared with White (8.7%) and other minority (6.6%) children. Among those with a need, only 23.5 percent received some care. Hispanics and other minorities show the highest rates of unmet need, 86.4 percent and 86.6 percent, respectively, compared with 78.3 percent for Blacks and 69.3 percent for Whites. Approximately 7 percent of the families with a child in need claimed financial barriers as the reason for not getting any mental health care.
The intensity of care is as important a factor as the percentage of users when considering utilization patterns. The bar graph in Figure 5 shows the number of contacts per 1,000 population by age group. Among the privately insured and the uninsured, adolescents tend to have more contacts with mental health specialists than adults, while the younger children (ages 1 to 11) have the fewest. In Medicaid and other public insurance programs, adults (ages 18 to 64) tend to have more contacts per 1,000 population than children. The high contact levels for publicly insured adults reflects the fact that the adults who are eligible for public insurance programs tend to have more serious mental illnesses than the general population.
Figure 4: Unmet Need for Mental Health Services
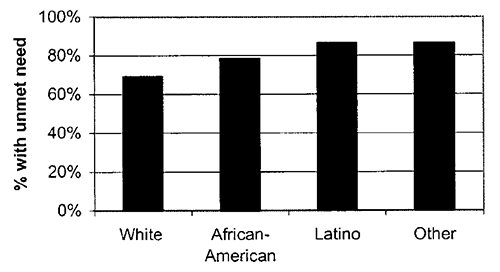
Calculations based on data from the National Health Interview Study.
Figure 5: Outpatient Visits per 1,000 Population
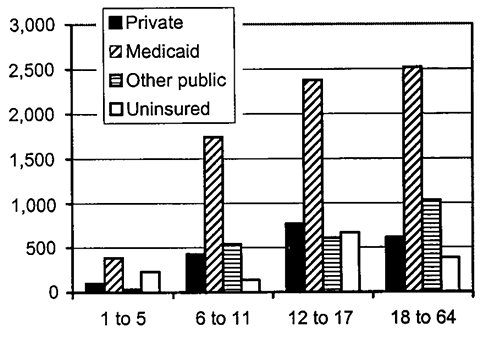
Calculations based on data from the National Survey of American Families.
We compared the survey results regarding contacts per 1,000 population with 1998 claims/encounter data from United Behavioral Health, the third-largest managed behavioral health organization, with around 18 million covered lives in all 50 States (Cuffel et al., 1999), and traditional plans of large employers that are customers of Ingenix. The rates of any mental health specialty use among the privately insured members were somewhat lower than the survey rates (roughly 1 percent, although with a substantial variation across employers and States), but the number of visits per user was substantially lower. As a consequence, the number of outpatient visits per 1,000 was under 220 in the privately insured 6–11 age group and under 360 for the 12–17 age group. These numbers account for only about 50 percent of the outpatient visits per 1,000 estimated from the NSAF, which suggests that a large proportion of services is provided outside mental health specialty settings covered by insurance. The education sector likely accounts for a large portion of the difference. Our estimates of out-of-plan specialty care use may even be an underestimate, because parent reports of child utilization, as in the NSAF, are likely to be biased downward. It is important to note that not all outpatient mental health services are obtained through specialty providers. Data from Ingenix provide evidence that a substantial amount of mental health care is provided in primary care settings (304 primary care mental health outpatient visits per 1,000 population).
Inpatient Utilization in Community Hospitals
Data from the HCUP and NHDS indicate that between 0.2 percent and 0.3 percent of children ages 1 to 17 use inpatient mental health services. This rate is substantially lower than the rate for adults (0.6%). While the two data sources lead to similar estimates of population inpatient use, the percentage of hospital inpatient stays with a primary diagnosis of a mental health disorder is higher in the NHDS. The patterns of use across age and insurance groups, however, are quite similar. The youngest group has the lowest utilization of inpatient mental health services and adolescents have the highest. There is no major difference in the average length of mental health inpatient stays, although the mean stay for children ages 6 to 11 was slightly longer than for the other age groups. Interesting differences in inpatient mental health care utilization are found across insurance types. Medicaid and other public insurance programs have the longest stays. The privately insured and the uninsured look very similar in their patterns of inpatient mental health service use.
Figure 6: Inpatient Days per 1,000 Population
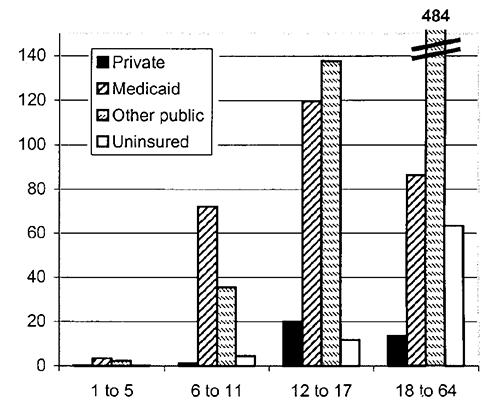
Calculations based on data from the Healthcare Cost and Utilization Project.
The HCUP data highlight interesting differences in the patterns of inpatient mental health service use between adults (ages 18 to 99) and children. Across all insurance types, adults and adolescents have greater inpatient days per 1,000 population than young children. Among the privately insured and the uninsured, adolescents have higher inpatient service use than adults. In contrast, among the publicly insured, inpatient days per 1,000 population are significantly higher for adults than for adolescents. The adults who are eligible for Medicaid and other public insurance programs tend to have higher levels of mental health service need than the general population.
Medications
The fast-growing use of psychotropic medications for children has received attention in both the professional and popular press. The Ingenix data provide estimates of medication use among privately insured children in 1998. Approximately 4.3 percent of children received psychotropic medication. Utilization is concentrated among older children, with 5.0 percent of 6- to 11-year-olds and 5.6 percent of adolescents on psychotropic medication, while only 0.7 percent of children ages 1 to 5 had any use.
Stimulants were the most common medication prescribed in all age groups; they were used substantially more often than all other medications combined in 1- to 5-year-olds and 6- to 11-year-olds. In adolescents, the rate of antidepressant use approached that of stimulants, which is not surprising given the increased prevalence of mood disorders in teens.
Figure 7: Utilization of Psychotropic Medications
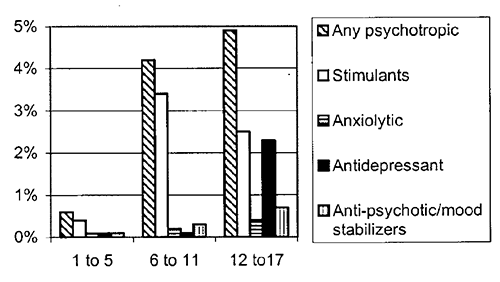
Calculations based on data from Ingenix.
National Expenditure Estimates
Total treatment expenditures for children in 1998 were estimated to be around $11.75 billion, or about $173 per child. Adolescents (12–17) account for 59 percent of the total and also have the highest expenditure per child at $291; children 6 to 11 account for 34 percent of the total and $165 per child; children 1 to 5 for 7 percent and $39 per child.
Figure 8: Total Mental Health Costs, by Age Group
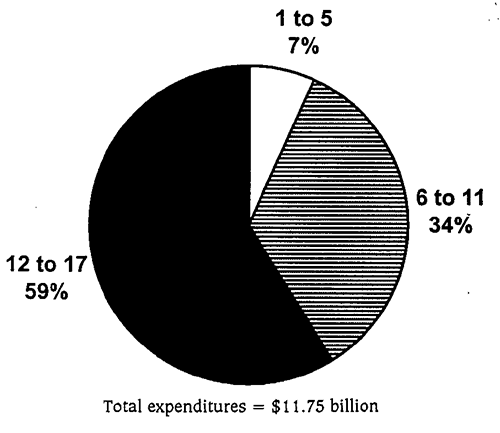
In contrast to the previous estimates for adolescents, which attributed about two-thirds of all expenditures to inpatient (hospital and residential) care (OTA, 1991; Burns, 1991), estimates for 1998 show that outpatient care accounts for the largest share (see Figure 9). This finding for children replicates the differences between recent managed care data and earlier actuarial databases for privately insured populations (Sturm, 1997). Over the past decade, there has been a dramatic shift away from inpatient toward outpatient care, a trend that is not unique to mental health. Some of the shift has been driven by economic factors and managed care, and some has been the result of therapeutic advances.
In the calculation of the cost shares by service type, the State and local expenditures estimated from the IMHO are allocated between outpatient and inpatient services. This process may lead to some overcounting, as some of the outpatient visits paid for by State and local payers may be included in the NSAF-based estimates of specialty outpatient expenditures for the privately insured. We expect, however, that this double counting is minimal.
There is some variation across age groups in the cost share of outpatient services. The share of outpatient costs for the 1–5 age group is greater than that for the other groups, while the share of inpatient costs is lower. The share of medication costs remains relatively constant across age groups.
For targeting policy interventions, it is important to see which children account for what proportion of expenditures. One difficulty in separating costs by payer is that a child’s insurance status is not a reliable indicator of who actually pays for services. State and local mental health agencies (including Federal block grants) account for about 25 percent of all expenditures but serve children with private insurance, no insurance, or Medicaid or other public insurance programs, and we cannot assign the relative proportions. Nevertheless, Figure 11 shows that children with private insurance account for at least 47 percent of all expenditures and possibly over 55 percent, depending on the share of the resources from State mental health agencies that they receive. The role of private insurance also differs by age groups and is largest for adolescents.
Similar patterns of shares are seen across all age groups. The expenditure share attributed to the privately insured is smaller than the percentage of children with private insurance. Likewise, the Medicaid share of expenditures is greater than the percentage of children with Medicaid coverage.
Figure 9: Total Mental Health Costs, by Type of Service
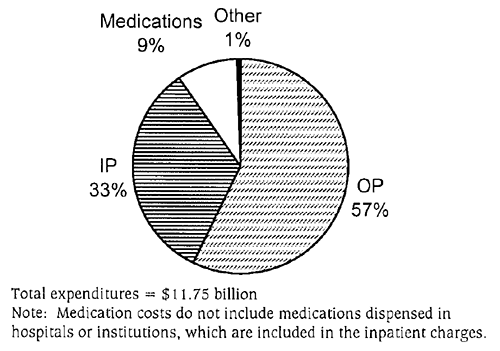
Figure 10: Total Mental Health Costs, by Type of Service and Age Group
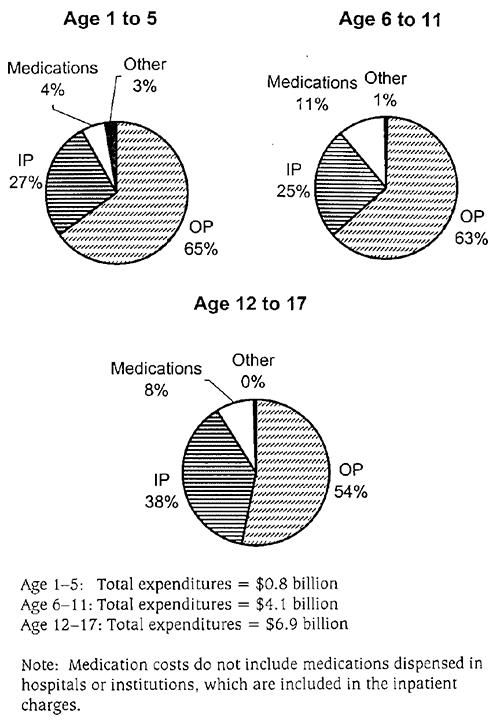
These estimates indicate that the mental health costs per child enrolled are higher under Medicaid than under private insurance.
Based on survey data, children with private insurance have more mental health specialty visits than can be accounted for by paid claims. A large share of those additional visits are provided through schools, and some services are self-paid, out-of-plan use or services provided by public mental health agencies. In addition, expenditures for mental health services in primary care paid for by insurance are greater than specialty mental health services paid by insurance. Figure 13 shows that primary care outpatient expenditures paid by insurance are significantly larger than for specialty care in the adolescent group. For the younger age groups, the expenditures between the different types of providers are closer in size. The primary care expenditures shown in Figure 13 may include some expenditures for specialty mental health outpatient visits. There appears to be some inconsistency in the reporting of specialty versus primary care in our private sector data sets, and some specialty visits may be categorized as primary care.
For uninsured children, probably only a small share of the expenditures will be paid out-of-pocket; most are paid through a mixture of charity care, school-based services, and public agencies.
Figure 11: Total Mental Health Costs, by Insurance Status
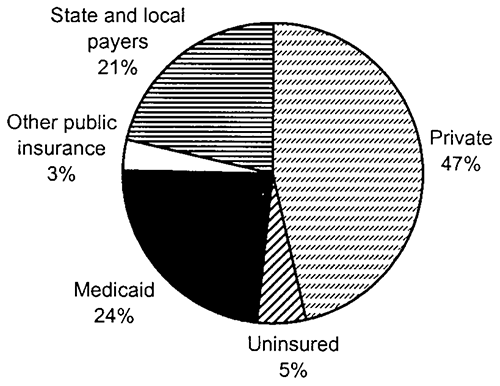
Figure 12: Total Mental Health Costs, by Insurance Status and Age Group
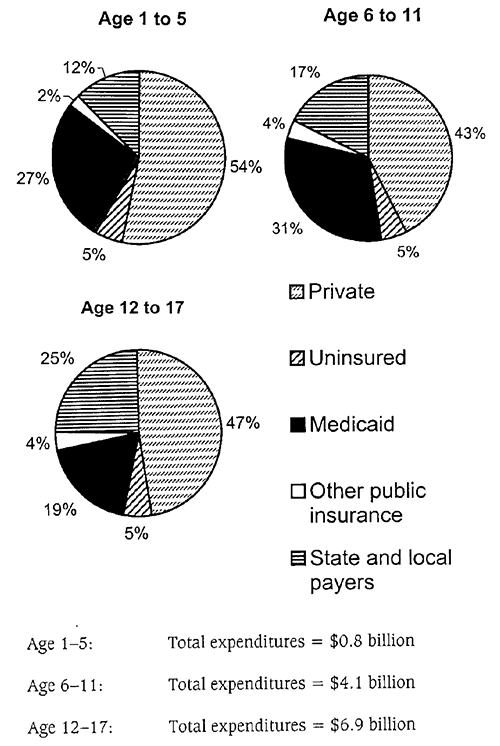
Medication Costs
Total expenditures on psychotropic medications for children in 1998 are estimated to be $1.1 billion. The largest proportion of expenditures was for stimulants, which accounted for slightly over 40 percent of the total. Antidepressant costs made the second largest contribution, accounting for 33 percent of the total. The share of prescriptions differs because the majority of stimulant prescriptions written in 1998 were relatively inexpensive generic methylphenidate, while the majority of antidepressant and antipsychotic prescriptions were for brand name medications for which generic equivalents are not yet available. However, the recent increase in prescribing of nongeneric stimulants (new stimulant formulations and extended-release methylphenidate) may lead to an increase in the overall cost of stimulants.
The shares of total drug costs vary across age groups. The stimulant cost share is lower for adolescents than for the other age groups. This is due in part to the increased importance of antidepressants in the total drug costs for the 12–17 age group.
Mental Health Expenditures in the Education Sector
The out-of-plan specialty outpatient visits that are seen in the NSAF likely reflect in large part services received through the school system. The data however, do not allow us to test this hypothesis. In an effort to estimate school-based expenditures directly, we obtained data from the Los Angeles County School District on salaries for mental health professionals. These data show that the district spends approximately $72 per enrolled student on mental health professionals in the school. If Los Angeles County were representative of all school districts, this finding would indicate that total school expenditures in the United States on mental health professionals would be $4.1 billion. Los Angeles County, however, does not appear to be typical in that its expenditures per student are higher than we would expect to find in most districts. Thus, these data likely provide a high estimate of school-based expenditures on the provision of mental health services in the education sector.
An additional method of measuring the expenditures on mental health treatment in the school setting is to compare the expenditure per pupil in regular and special education. The difference between the two per-pupil measures can be seen as the excess cost of educating a child with a disability. Estimates in the literature of this excess cost range from approximately $4,600 to $10,100 per student (Lankford and Wyckoff, 1996; Lewit et al., 1995; Chaikind and Corman, 1991). The excess cost incorporates both direct mental health treatment expenditures and expenditures on ancillary services. Unfortunately, we are unable to break the aggregate estimate down into these two components. To obtain national estimates of school mental health expenditures, we used data from the U.S. Department of Education report on the implementation of the Individuals with Disabilities Education Act (IDEA)(U.S. Department of Education, 2000). These data indicate that approximately 450,000 children with SED were served under IDEA during the 1997-98 school year. Consequently, the excess cost of educating SED children in the United States is estimated to be between $2.0 and 4.5 billion.
The Top-Down Approach
As a basis of comparison for our estimates, we started with the total mental health spending estimates for all ages from Coffey et al. (2000) and used micro-level data to carve out the portion that could be attributed to children. This method produces an estimate of child mental health expenditures of $14.3 billion. Although the total is somewhat higher, the share breakdown across the type of service provided based on the top-down approach (shown in Figure 14) is quite similar to that from our bottom-up approach.
Figure 13: Outpatient Health Costs for the Privately Insured
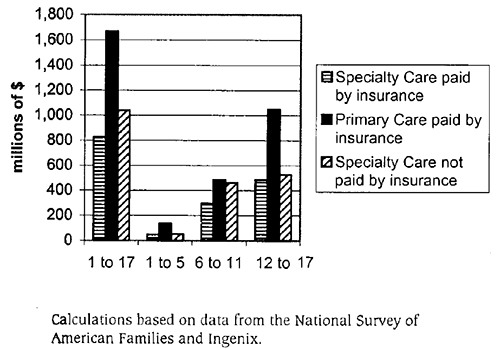
Figure 14: Expenditures on Psychotropic Medications, by Drug Category
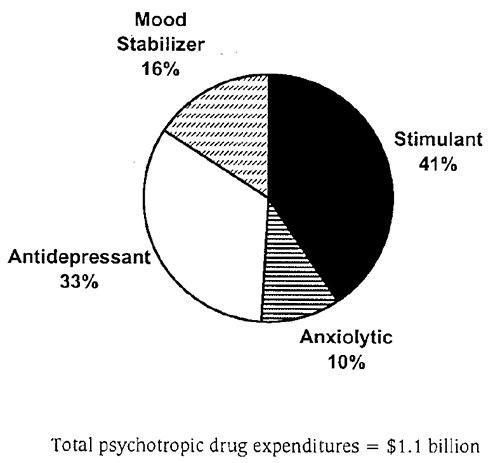
Figure 15: Expenditures on Psychotropic Medications, by Drug Category and Age Group
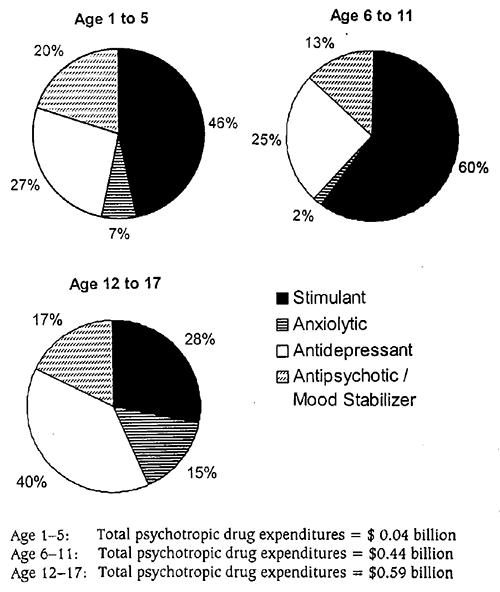
Figure 16: Total Mental Health Costs From the Top-Down Approach, by Type of Service
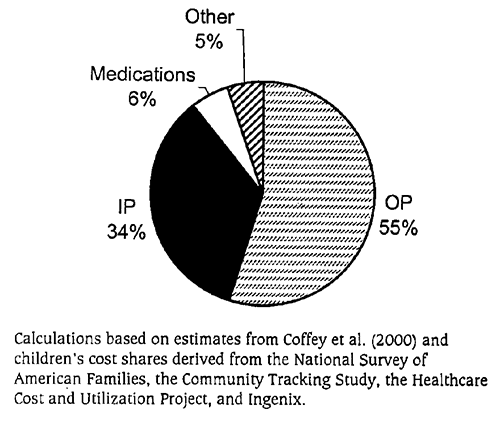
Acknowledgments
NIMH funded the research for this report. We thank Barbara Burns, Agnes Rupp, and members of the NIMH Child Council Workgroup for comments during the preparation of the report. Cheri Dolezal, John Landsverk, Noel Mazade, Abram Rosenblatt, and Bonnie Zima helped us to gain access to additional data.
References for Appendix A
Angold A, Erkanli A, Egger HL, Costello EJ. Stimulant Treatment for Children: A community perspective, Journal of the American Academy of Child and Adolescent Psychiatry 2000; 39(8):975–984; 984–994.
Bruijnzeels MA, van der Wouden JC, Foets M, Prins A, van den Heuvel WJ. Validity and accuracy of interview and diary data on children’s medical utilisation in The Netherlands, Journal of Epidemiology and Community Health 1998;52(1):65–69.
Buck JA. Utilization of Medicaid mental health services by nondisabled children and adolescents, Psychiatric Services 1997; 48(1):65–70.
Buck JA, Miller K, Bae J. Mental Health and Substance Abuse Services in Medicaid, 1993, DHHS Pub. No. (SMA) 99-3368. Rockville, MD: Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, 2000.
Burns BJ. Mental health service use by adolescents in the 1970s and 1980s, Journal of the American Academy of Child and Adolescent Psychiatry 1991;30(1):144–150.
Burns BJ, Costello EJ, Angold A, Tweed D, Stangl D, Farmer EM, Erklani A. Children’s mental health service use across service sectors, Health Affairs (Millwood) 1995; 14(3):147–159.
Burns BJ, Costello EJ, Erkanli A, Tweed DL, Farmer EMZ, Angold A. Insurance coverage and mental health service use by adolescents with serious emotional disturbance, Journal of Child and Family Studies 1997; 6(1):89–111.
Chaikind S, Corman H. The impact of low birth weight on special education costs, Journal of Health Economics 1991; 10:291–311
Coffey RM, Mark T, King E, Harwood H, McKusick D, Genuardi J, Dilonardo J, Buck J. National Estimates of Expenditures for Mental Health and Substance Abuse Treatment, 1997. SAMHSA Publication SMA-00-3499. Rockville, MD: Center for Substance Abuse Treatment and Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, July 2000.
Cuffel B, McCulloch J, Goldman W. Behavioral Health Service Use by Children and Adolescents in a Managed Behavioral Health Carve-Out. Report prepared for NIMH, 1999.
Farmer EM, Stangl DK, Burns BJ, Costello EJ, Angold A. Use, persistence, and intensity: patterns of care for children’s mental health across one year, Community Mental Health Journal 1999; 35 (1):31–46.
Frank RG, Kamlet MS. Direct costs and expenditures for mental health in the United States, Hospital and Community Psychiatry 1985;36(2):165–168.
Glied S, Hoven CW, Moore RE, Garrett AB, Regier DA. Children’s access to mental health care: Does insurance matter? Health Affairs (Millwood) 1997;16(1):167–174.
Halfon N, Berkowitz G, Klee L. Children in foster care in California: An examination of Medicaid reimbursed health service utilization, Pediatrics 1992a;89(6 pt 2):1230–1237.
Halfon N, Berkowitz G, Klee L. Mental health service utilization by children in foster care in California, Pediatrics 1992b;89(6 pt 2):1238–1244.
Health Care Financing Administration. National Health Accounts: Lessons from the U.S. Experience, available at http://www.hcfa.gov/stats/nheoact/lessons .
Hoagwood K, Rupp A. Mental Health Service Needs, Use and Costs for Children and Adolescents with Mental Disorders and Their Families: Preliminary Evidence. In Mental Health, United States, 1994, ed. Ronald W. Manderscheid and M.S. Sonnenschein. DHHS pub. SMA 94-3000. Washington, DC: U.S. Government Printing Office. Chapter 4, pp. 52-64.
Institute of Medicine, National Academy of Sciences. Research on Children and Adolescents’ Mental, Behavioral, and Developmental Disorders: Mobilizing a National Initiative. Washington, DC: Academy Press, 1989.
Jensen PS, Kettle L, Roper MT, Sloan MT, Dulcan MK, Hoven C, Bird HR, Bauermeister JJ, Payne JD. Are stimulants overprescribed? Treatment of ADHD in four U.S. Communities, Journal of the American Academy of Child and Adolescent Psychiatry 1999;3(7):797–804.
Koyanagi C, Feres-Merchant D. For the Long Haul: Maintaining Systems of Care Beyond the Federal Investment. Systems of Care: Promising Practices in Children’s Mental Health, 2000 Series, Volume III. Washington, DC: Center for Effective Collaboration and Practice, American Institutes for Research, 2000.
Lankford H, Wyckoff J. Special Education and Regular Instruction. In Holding Schools Accountable, ed. Helen Ladd. Washington, DC: Brookings Institution, 1996.
Leaf PJ, Alegria M, Cohen P, Goodman SH, Horwitz SM, Hoven CW, Narrow WE, Vaden-Kiernan M, Regier DA. Mental health service use in the community and schools: Results from the four-community MECA study, Journal of the American Academy of Child and Adolescent Psychiatry 1996;35(7):889–897.
LeFever GB, Dawson KV, Morrow AL. The extent of drug therapy for attention deficit-hyperactivity disorder among children in public schools, American Journal of Public Health 1999; 89(9):1359–1364.
Levit K, Cowan C, Lazenby H, Sensenig A, McDonnell P, Stiller J, Martin A. Health spending in 1998: Signals of change, Health Affairs (Millwood) 2000;19(1):124–132.
Lewit E, Baker L, Corman H, Shiono P. The direct cost of low birth weight, The Future of Children 1995;5(1):35–56.
Libby A, Rosenblatt A, Snowden L. Mental Health Screening, Assessment, and the Treatment Services and Additional Costs for Children in Foster Care or on Probation and Their Families. Report prepared for California Department of Mental Health, 1999.
Mark T, McKusick D, King E, Harwood H, Genuardi
J. National Expenditures for Mental Health, Alcohol, and Other Drug Abuse Treatment, 1996. Rockville, MD: Office of Managed Care, Center for Substance Abuse Treatment, 1998.
Mark TL, Coffey RM, King E, Harwood H, McKusick D, Genuardi J, Dilonardo J, Buck JA. Spending on mental health and substance abuse treatment, 1987–1997, Health Affairs 2000;19(4):108–120.
Mathiowetz NA, Dipko SM. A comparison of response error by adolescents and adults: Findings from a health care study, Medical Care 2000; 38(4):374–382.
Olfson M, Marcus SC, Pincus HA. Trends in office-based psychiatric practice, American Journal of Psychiatry 1999;156(3):451–457.
Olfson M, Marcus SC, Pincus HA, Zito JM, Thompson JW, Zarin DA. Antidepressant prescribing practices of outpatient psychiatrists, Archives of General Psychiatry 1998;55(4):310–316.
Rappley MD, Mullan PB, Alvarez FJ, Eneli IU, Wang J, Gardiner JC. Diagnosis of attention-deficit/hyperactivity disorder and use of psychotropic medication in very young children, Archives of Pediatric and Adolescent Medicine 1999;153:1039–45.
Rice DP, Kelman S, Miller LS, Dunmeyer S. The Economic Costs of Alcohol and Drug Abuse and Mental Illness, 1985. San Francisco: Institute for Health and Aging, University of California, 1990.
Safer DJ, Malever M. Stimulant treatment in Maryland public schools, Pediatrics 2000;106(3): 533–539.
Sturm R. How expensive is unlimited mental health care coverage under managed care? Journal of the American Medical Association 1997;278(18):1533–1537.
Sturm R, Klap R. Use of psychiatrists, psychologists, and master’s level therapists in managed behavioral health care carve-out plans, Psychiatric Services 1999;50(4):504–508.
Sturm R, Gresenz C, Sherbourne C, Minnium K, Klap R, Bhattacharya J, Farley D, Young AS, Burnam MA, Wells KB. The design of health care for communities: A study of health care delivery for alcohol, drug abuse, and mental health conditions, Inquiry 1999;36(2):221–233.
Takayama JI, Bergman AB, Connell FA. Children in foster care in the state of Washington, Journal of the American Medical Association 1994;271(23):1850–1855.
U.S. Congress, Office of Technology Assessment. Adolescent Health, Chapter 11, Vol. II: Background and the Effectiveness of Selected Prevention and Treatment Services, OTA-H-466. Washington, DC: U.S. Government Printing Office, 1991.
U.S. Congress, Office of Technology Assessment. Children’s Mental Health: Problems and Services—A Background Paper, OTA-BP-H-33. Washington, DC: U.S. Government Printing Office, December 1986.
U.S. Department of Education. The Twenty-Second Annual Report to Congress on the Individuals with Disabilities Education Act (IDEA). Washington, DC: U.S. Government Printing Office, 2000.
U.S. Department of Health and Human Services. Mental Health: A Report of the Surgeon General—Executive Summary. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health, 1999.
Wells KB, Sherbourne CD, Sturm R, Young AS, Burnam MA. Profiles of Care for Alcohol, Drug Abuse, and Mental Health Problems for Uninsured and Insured Adults. Research Center on Managed Care for Psychiatric Disorders Working Paper No. 202, November, 2000.
Wright G, Smolkin S, Bencio D. Medicaid Mental Health and Substance Abuse, 1992. Use and Cost Estimates in Michigan and California, Mathematica Reports, prepared for NIMH, 1995.
Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications to preschoolers, Journal of the American Medical Association 2000;283(8):1035–1030.
Zito JM, Safer DJ, dosReis S, Magder LS, Gardner JF, Zarin DA. Psychotherapeutic medication patterns for youths with attention deficit-hyperactivity disorder, Archives of Pediatrics and Adolescent Medicine 1999;153:1257–1263.
Zito JM, Safer DJ, dosReis S, Magder LS, Riddle MA. Methylphenidate patterns among Medicaid youths, Psychopharmacology Bulletin 1997;33(1):143–147.
Zito JM, Safer DJ, Riddle MA, Johnson RE, Speedie SM, Fox M. Prevalence variations in psychotropic treatment of children, Journal of Child and Adolescent Psychopharmacology 1998;8(2):99–105.
| 1 to 17 | 1 to 5 | 6 to 11 | 12 to 17 | |
|---|---|---|---|---|
| Grand Total | 11,750 | 774 | 4,047 | 6,930 |
| Totals by Insurance Status | ||||
| Private | 5,456 | 411 | 1,725 | 3,320 |
| Uninsured | 621 | 41 | 202 | 378 |
| Medicaid | 2,762 | 207 | 1,267 | 1,288 |
| Other public insurance | 408 | 18 | 146 | 243 |
| State and local payers | 2,504 | 96 | 707 | 1,701 |
| Totals by Service Type | ||||
| Outpatient | 6,739 | 502 | 2,554 | 3,683 |
| Inpatient | 3,870 | 209 | 1,032 | 2,629 |
| Medications | 1,068 | 42 | 439 | 586 |
| Other mental health services | 74 | 20 | 22 | 32 |
| Note: Expenditures are in millions of dollars. | ||||
| Totals by Insurance Status and Type of Service | 1 to 17 | 1 to 5 | 6 to 11 | 12 to 17 |
|---|---|---|---|---|
| Private | ||||
| Specialty outpatient | 1,867 | 98 | 758 | 1,011 |
| Primary care outpatient | 1,669 | 137 | 484 | 1,048 |
| Inpatient | 1,190 | 138 | 195 | 856 |
| Medication | 670 | 20 | 270 | 380 |
| Other mental health services | 61 | 18 | 19 | 25 |
| Private Total | 5,456 | 411 | 1,725 | 3,320 |
| Medicaid | ||||
| Outpatient | 1,460 | 165 | 672 | 623 |
| Inpatient | 1,047 | 26 | 479 | 542 |
| Medication | 254 | 17 | 115 | 122 |
| Other mental health services | 0.9 | 0.0 | 0.2 | 0.7 |
| Medicaid Total | 2,762 | 207 | 1,267 | 1,288 |
| Other Public Insurance | ||||
| Outpatient | 264 | 15 | 96 | 153 |
| Inpatient | 83 | 1 | 27 | 54 |
| Medication | 57 | 2 | 22 | 32 |
| Other mental health services | 4 | 0.1 | 0.9 | 3 |
| Other Public Insurance Total | 408 | 18 | 146 | 243 |
| Uninsured | ||||
| Specialty outpatient | 214 | 12 | 81 | 121 |
| Primary care outpatient | 285 | 24 | 78 | 183 |
| Inpatient | 27 | 0 | 8 | 18 |
| Medication | 88 | 3 | 33 | 52 |
| Other mental health services | 8 | 2 | 2 | 3 |
| Uninsured Total | 621 | 41 | 202 | 378 |
| Note: Expenditures are in millions of dollars. The $2,504 million in expenditures made by State and local payers cannot be allocated among children with different insurance types. | ||||
Appendix B
Clinical Case Study
How Research Informs Clinical Case Management in Childhood-Onset Depression
Introduction
The direct relevance of research findings to clinical care is not always clear. This appendix presents a clinical case example to illustrate how clinicians, in treating children, can use specific research findings from basic and applied studies. The clinical case about Amy provides an illustration of how the types of research discussed throughout this report can guide clinical care and influence the developmental trajectory of childhood-onset depression. Depression is highlighted because of its public health relevance. It is a common, chronic, and recurrent condition that can disrupt and skew normal development and result in significant long-term morbidity (e.g., academic problems, delinquency, unemployment, marital difficulties, and medical hospitalization) and mortality (e.g., suicide). In spite of the recognition of the serious consequences of depression, it is frequently under-diagnosed and inadequately treated in children (Beasley & Beardslee, 1998; Wolraich, Felice & Drotar, 1996). This case illustrates how consistent application of research findings to clinical practice can allow for a more systematic, science-based and developmentally informed approach to treatment and prevention of depression in children.
The utility of the science base and its importance for preventive efforts and clinical decision-making will be highlighted in this appendix with discussions addressing risk factors, phenomenology of depression across development, psychosocial and pharmacological treatments, suicide and social connectedness, course and outcome, and access to care and prevention.
Case Presentation
Amy is a 10-year-old girl with new onset depressive symptoms over a 5-month period. These were first noted in school, where her teachers described her as irritable, with a low frustration tolerance, decreased concentration, and decreased motivation in completing her school assignments. She attended the 4th grade in a public school, and over the past several months, her grades began to drop from B’s to D’s. Amy reported feeling increasingly guilty “for being the cause of the fighting” between her parents and for “having caused” her parents to divorce 2 years ago. Amy was offered supportive therapy by a school counselor, with whom she met weekly for the next 2 months. Not only did her symptoms not improve, but also, her mother noted Amy’s increased tearfulness, difficulty falling asleep, low energy, and decreased appetite, with a 5-pound weight loss, despite a ½" growth in height. In addition, Amy complained to the school counselor that nothing was fun anymore, and that she felt worthless. She was becoming increasingly socially isolated from a group of same-sex peers and dropped out of her community basketball league. Although Amy could be defiant at times, she did not tend to break rules at home or school and her only conduct problem was a new trend of telling lies to her friends, “so they will like me better,” behavior which was consistent with the low self-esteem noted by her teachers. Amy tended to view the world in a negative self-defeating manner, even when positive things happened to her.
Amy’s parents became concerned with her change in behavior and decreased functioning and took Amy to her pediatrician for a medical evaluation. Her mother felt very guilty for not recognizing her daughter’s symptoms earlier because she was distracted by her failing marriage. Amy’s parents had each tried to talk her out of her sad and irritable moods, but the discussions would usually result in Amy’s increased crying and running out of the room yelling, “Nobody understands me.” At the conclusion of the pediatric interview, it was apparent that her parents had been emotionally unavailable to Amy over the past several years, had not been involved with or aware of her school or social functioning skills, were often critical of her apparent lack of motivation, and were often inconsistent with discipline.
In terms of her past history, Amy struggled with reading in the first grade but was never tested for learning disabilities. She was described as an anxious, shy child who frequently had difficulty separating from her mother. She was able to overcome this anxiety to such an extent that she could make friends and go to school without any psychological or psychiatric intervention. In terms of her past medical history, Amy had been diagnosed with mild asthma at age 8; she used a steroid inhaler for flare-ups of the disease. She had reached precocious puberty with menarche at age 10. She was of average height and weight.
Her parents divorced when Amy was 8 years old, but marital conflict had been present for many years prior to the divorce. Her parents now had minimal contact with each other, and their contact was often filled with conflict. Amy, her 16-year-old brother, and her mother moved into a small house in a substantially less-expensive part of town, while her father moved away to a neighboring middle-class suburb where he continued to work as a salesman. Amy missed her father, with whom she had limited contact every other weekend. Her mother, who worked as a secretary, had a history of recurrent depression and Amy’s older brother, although an average student and good athlete, used marijuana and alcohol regularly. There was also a history of depression in the maternal grandparents, as well as a paternal uncle who suffered from alcoholism.
Amy’s parents married after high school, and while her mother was continuing her education, she unexpectedly became pregnant with Amy’s brother at the age of 20. Amy was the result of a planned pregnancy 6 years later. The pregnancy progressed normally and there was no prenatal exposure to medications, alcohol, or drugs, except for intermittent tobacco use. Amy was delivered 2 weeks early by a caesarian section due to hypoxia, but appeared normal at birth. Amy’s mother had depressive symptoms throughout the pregnancy, which evolved into a severe depression during the first year of Amy’s life, making her emotionally unavailable to her baby. Although Amy reached normal developmental milestones in terms of walking and talking, when compared with her toddler peers she did not seem to explore her environment with the same enthusiasm, had less affective responsiveness to emotion-inducing situations, and demonstrated an insecure attachment to her mother.
The pediatrician ruled out medical causes for depressive symptoms such as hypothyroidism, anemia, or drug abuse. The family was referred to a local mental health clinic. During her evaluation with a licensed psychologist, Amy was cooperative and superficially friendly. Her speech and cognitive functioning appeared normal. She was intermittently fidgety in her chair but otherwise had no abnormal movements. She described her mood as sad and her affect fluctuated between forced cheerfulness and tearful lability. She denied any current suicidal or psychotic thoughts, but she endorsed guilt and worthlessness during the end of the interview after initially denying these symptoms.
Discussion
1. Risk Factors for Child and Adolescent Depression
Known vulnerabilities for childhood depression include familial, biological, psychosocial, and cognitive factors. The case illustrates the presence of multiple risk factors commonly seen among children at risk for depression. A discussion of each of these risk factors follows.
A. Familial Risk Factors
Many studies suggest that familial factors are the best predictors of the development of depressive disorders in youth (Garrison et al., 1997; Kaslow, Deering & Ash, 1996; Kaslow, Deering & Racusin, 1994) and such factors may serve as an important starting point in diagnostic and treatment considerations. The case example illustrates several types of family risk factors, including the presence of parental psychopathology, high levels of family conflict, and inconsistent parenting (Birmaher et al., 1996; Reinherz, Giaconia, Hauf, Wasserman & Paradis, 2000; Rutter, 1990). Maternal depression can have an especially profound effect on infant development, not only by increasing the heritable risk for depression (Beardslee, Versage & Gladstone, 1998), but also psychosocially by sensitizing the child to later loss experiences or threats and undermining opportunities for social development due to parental unresponsivity and neglect (Radke-Yarrow, Cummings, Kuczynski & Chapman, 1985; Rutter, 1995). The effects of a mother’s depression on shaping her child’s brain circuitry and subsequent behavioral performance can begin in utero. Studies examining the neurobiology of pregnant, depressed women found higher plasma cortisol, beta-endorphins, and corticotropin-releasing hormone levels (Handley, Dunn, Waldron & Baker, 1980; Smith et al., 1990). The fetus, via placental blood flow, can experience these maternal neuroendocrine abnormalities. Further, fetuses may be at elevated risk due to inadequate health care and health risk behaviors (e.g., maternal smoking, poor nutrition) that have been associated with depression (Stowe, Calhoun, Ramsey, Sadek & Newport, 2001). Thus, even in utero factors such as depressive symptoms and intermittent tobacco use by her mother may have shaped Amy’s neurobiological vulnerability.
Family interactions of depressed parents with depressed offspring are characterized by more conflict, rejection, problems with communication, and less expression of affect, attention, and support when compared with families of normal controls (Beardslee et al., 1996; Downey & Coyne, 1990; Goodman & Gottlib, 1999; Harrington et al., 1997; Schwartz, Dorer, Beardslee, Lavori & Keller, 1990). Families of depressed children also showed increased levels of criticism (Puig-Antich et al., 1985) and rejection (Cole & McPherson, 1993), attachment difficulties, and elevated maternal/parental overprotection compared with controls (Armsden, McCauley, Greenberg, Burke & Mitchell, 1990; Burbach, Kashani & Rosenberg, 1989; Lovejoy, Graczyk, O’Hare & Neuman, 2000; Martin & Waite, 1994; McFarlane, Bellissimo & Norman, 1995). However, the stress caused by associated marital or economic factors may have more impact on parenting than direct aspects of parental depression (Downey & Coyne, 1990; Goodman & Brumley, 1990; Goodyer, Herbert, Tamplin, Secher & Pearson, 1997; Stubbe, Zahner, Goldstein & Leckman, 1993).
Studies show that the emotional stress Amy experienced as a result of her mother’s affective illness may have been reduced if her parents had learned how to respond in an accepting and validating way to her emotional needs (Focht-Birkerts & Beardslee, 2000). Collectively, studies suggest that early detection and treatment of maternal depression during pregnancy and in the postpartum period may have had a positive impact on Amy’s depressive trajectory, given the available effective treatment of depression during pregnancy (Szigethy & Wisner, 2000).
In addition to neglect secondary to maternal depression, this case also highlights another form of parental nonavailability: family conflict and divorce, and the need to focus more attention clinically on the impact of these factors on children like Amy. Recent studies investigating the impact of divorce on children have found that many of the psychological effects seen in children can be accounted for by the negative effects of a troubled marriage prior to divorce (Kelly, 2000). In fact, marital conflict has been shown to be a more important predictor of child adjustment than either the divorce itself or any post-divorce conflict (Hetherington, 1999; Hetherington & Stanley-Hagan, 1999; Kline et al., 1989). Direct detrimental effects of marital conflict include modeling of parents’ behavior, failure to learn appropriate social interaction skills, and physiological effects (Davies & Cummings, 1994). More recent research points to disturbances in affect regulation or emotional arousal mechanisms in young children exposed to violent or repetitive severe parental conflict (DeBellis, 1997; Lieberman & Van Horn, 1998). Indirect effects of marital conflict highlighted by the current case include poor quality of parenting and less paternal involvement, which can make children feel rejected or guilty, particularly children in the pre-adolescent developmental phase (Hetherington, 1999).
Children of divorce, when compared with children in never-divorced families, have significantly more adjustment problems. Hetherington (1999) summarized the complexity of gender and age issues with adjustment and achievement in boys and girls after divorce varying with age, time since divorce, type of parenting, and type and extent of conflict. These findings may explain why Amy manifested depressive symptoms while her brother struggled with substance abuse issues. The findings emphasize the need for the clinician to focus on each child individually and in the appropriate developmental context, particularly in high-conflict divorce families.
These reciprocal interactions with parents not only influence the child’s behavior but may also affect the development of neural circuits of the infant’s brain (Lyons-Ruth & Zeanah, 1993; Rogeness & McClure, 1996). Recent findings in rats suggest that the impact of early life events on the development of behavioral and endocrine responses to stress are mediated through changes in mother-offspring interactions; these findings have identified brain regions (e.g., locus ceruleus, amygdala, frontal cortex) and hypothalamic-pituitary-adrenal (HPA) glucocorticoid systems as critical targets for the effects of variations in maternal care (Francis, Caldji, Champagne, Plotsky & Meaney, 1999; Caldji et al., 1998; Francis & Meaney, 1999; Meaney et al., 1996; Meaney, 1999). In human infants, neglect has been associated with lower reactivity of the HPA axis, which has been hypothesized to represent a self-protective feedback mechanism to counter the potentially damaging effects of elevated cortisol levels (Gunnar, 1998). Elevated cortisol levels have been associated with damage to the hippocampus, a region essential for memory (Sapolsky, 1996). Finally, both monkey and human infants exposed to maternal neglect have shown changes in the development of norepinephrine systems; norepinephrine is a neurotransmitter implicated in many regulatory brain functions (Fleming, O’Day & Kraemer, 1999; Rogeness & McClure, 1996). Such fundamental work in neuroscience has helped to connect what is known about the effects of parental neglect on the developing brain and has important implications for the development of early interventions for any form of parental neglect.
The interplay between genetic and environmental factors in determining risk for psychopathology in children at risk of depression is complex. Amy showed vulnerability to depression in several domains of functioning, including cognitive (low self-esteem, helplessness), affective (poor emotional regulation), and behavioral functioning (social isolation, low mastery motivation). Goodman & Gotlib (1999) proposed a developmental model, based on empirical evidence from animal and human studies, for understanding the mechanisms of transmission of risk from depressed mothers to their offspring. In this model, four mechanisms through which risk might be transmitted are evaluated: (1) heritability of depression; (2) innate dysfunctional neuroregulatory mechanisms; (3) exposure to negative maternal cognitions, behaviors, and affect; and (4) the stressful context of the children’s lives. Three factors were proposed to moderate such risks, including the father’s health and involvement with the child, the course and timing of the mother’s depression, and characteristics of the child. This model is consistent with the literature on resiliency. Many children appear to develop normally both in terms of brain and behavior in the face of parental adversities (Luthar & Cicchetti, 2000). Similar factors appear to play a role in determining resilience: (1) attributes of the children (e.g., temperament, cognitive and social-emotional competence, self-confidence, realistic assessment of parental limitations); (2) aspects of their families (e.g., parental perspectives about children and the developmental process, maternal interactive behaviors); and (3) characteristics of their wider social environments (family social support, social status) (Cicchetti & Rogosch, 1997; Luthar & Cicchetti, 2000; Masten, Best & Garmezy, 1990; Sameroff, Seifer, Barocas, Zax & Greenspan, 1987). Resilient youth with affectively ill parents were found to be activists, deeply involved in school and extracurricular activities, deeply committed to interpersonal relationships, and they valued self-understanding in coping with parental affective illness (Beardslee & Podorefsky, 1988). Similarly, protective buffers for children in high-conflict marriages include a good relationship with at least one parent, parental warmth, supportive siblings, and, for adolescents, good self-esteem and peer support (Emery, 1999).
Based on this research, multiple interventions can be included in a treatment plan to reduce Amy’s risks and increase her resiliency. These could include working with her parents to increase consistent parenting and more positive engagement with Amy and decreasing parental conflict given the detrimental effects of untreated adversity on the child’s developing brain and behavior (Downey & Coyne, 1990). Additional strategies may include increasing paternal involvement; identifying and treating maternal depression; utilizing extended family or community social support; encouraging Amy’s continued involvement in extracurricular activities to increase social competence and self-confidence; providing psychoeducation about depression; and offering age-appropriate explanations of the psychological and legal aspects of the divorce process to support children’s positive adjustment and mental health (Beardslee et al., 1997; Pruett & Pruett, 1999).
B. Biological Considerations/Risk Factors
Gender—Another important risk factor for Amy’s expression of depression is her female gender. Adolescent females are twice as likely to experience depression than their male peers; this is a cross-cultural phenomenon (Angold, Costello & Worthman, 1998; Nolen-Hoeksema et al., 1994). Explanations for the increase in adolescent females’ vulnerability to depression include differences in sex-role socialization, cognitive styles, presence and timing of negative life events, greater interpersonal sensitivity, and differential hormonal changes associated with puberty (e.g., changes in circulating gonadal hormones exerting direct or potentiating effects on the central nervous system related to mood disturbances) (Brooks-Gunn & Warren, 1989; Cyranowski, Frank, Young & Shear, 2000; Petersen et al., 1993; Schraedley, Gotlib & Hayward,1999; Silberg et al., 1999; Warren & Brooks-Gunn, 1989). Physical changes associated with puberty (e.g., breast development, increased body fat) have been related to negative perceptions of body image, particularly if females experience these changes before those in their peer group (Angold et al., 1998; Ge, Conger & Elder, 1996; Siegel, Yancey, Aneshensel & Schuler, 1999). The precocious puberty exhibited by Amy is consistent with studies that related early pubertal maturation in female offspring to maternal depression, an effect that appears to be mediated by discordant family relationships and the absence of the biological father (Ellis & Garber, 2000; Kim & Smith, 1998).
One integrative model exploring the etiology of depression further suggests that the combination of social and hormonal mechanisms present in pubertal females stimulates heightened needs for affiliation (e.g., preference for intimacy within interpersonal relationships) (Cyranowski et al., 2000). While most adolescent females undergo the transition from parental to peer attachments with relative ease, children like Amy, with insecure parental attachments, poor interpersonal coping skills, or anxious or inhibited temperaments, can have increased difficulties with socially expected role transitions and thus have a greater risk of depression during puberty. These findings suggest that these related realms of functioning deserve particular attention by the treating clinician, particularly for children at a higher risk for depression.
Psychiatric Comorbidity—One promising area for integrating basic behavioral and neuroscience research into clinical practice is the comorbidity of depressive and anxiety disorders. As noted above, children with anxious temperaments, particularly girls like Amy, have an increased risk for later onset of social anxiety and depression and differences in sympathetic reactivity (Kagan & Snidman, 1999; Schwartz, Snidman & Kagan, 1999). In adults, generalized anxiety disorder has been conceptualized as a prodrome or severity marker of major depression (Birmaher et al., 1996; Kessler, DuPont, Berglund & Wittchen, 1999; Merikangas, Risch & Weissman, 1994; Pine, Cohen, Gurley, Brook & Ma, 1998; Pine & Grun, 1999;); in adolescents, the expression of depression has been related to changes in processing fear, threat, and anxiety (Pine et al., 1998; Pine & Grun, 1999). Further, both depressive and anxiety disorders share a common genetic diathesis, puberty-specific expression in females, similar neuroanatomical underpinnings (e.g., amygdala, cingulate cortex, orbital cortex), and neurochemical substrates (e.g., serotonin, catecholamines) for pharmacological interventions (Birmaher et al., 1996; Dahl, 2001; DeBellis et al., 2000; Drevets, 2000; Kendler, 1996; LeDoux, 1998). In fact, abnormal amygdaloid function has been implicated in anxiety and depression and its function normalized after antidepressant treatment (Drevets, 1999; Drevets, Gadde & Krishnan, 1999). Finally, cognitive-behavioral interventions have been shown to be effective in the treatment of both anxiety disorders and depression. It is possible that such interventions targeted early in the course of some anxiety disorders (and/or in some high risk individuals at risk for anxiety/depression) may be capable of altering the developmental path of these disorders. A better understanding of the basic changes in affect regulation and underlying neurobehavioral systems and circuits may help to better focus these interventions.
Another area for integrating basic behavioral and neuroscience research is in the area of learning disabilities. It is not uncommon for children like Amy to encounter learning problems in conjunction with anxiety and depression (Lyon, 1996). A comprehensive neuropsychological assessment will be important to better understand the extent of her learning problems. Such an assessment is important for an understanding of the emotional and neuropsychological contributions to Amy’s learning difficulties. In other words, understanding whether Amy’s learning problems are secondary to her depression and anxiety or if they coexist with her psychiatric conditions can aid in the development of a more effective treatment plan. Identifying the pattern of cognitive functioning within different cognitive areas (e.g., executive functioning, language functioning, sensory-perceptual functioning) can aid in the choice of treatment(s) for her learning problems as well as her psychiatric disorders. Developmental processes (Durlak, Fuhrman & Lampman, 1991) can influence whether particular types of therapy (e.g., CBT) will be useful.
Physical Illness Comorbidity—Another important yet often neglected area in the clinician’s office is the overlap of depression and chronic physical illness in children and adolescents. Children like Amy, with comorbid depressive disorder and chronic physical illness such as asthma, have higher health care utilization, poor medical outcome, more functional impairment, decreased quality of life, and increased mortality (Strunk, 1987). Despite findings that children with certain disorders (e.g., asthma, cancer, sickle cell anemia) appear to have increased risk of depressive symptoms compared with other disorders, physical illness factors (e.g., type of disorder, severity or duration of disorder) are generally poor predictors of depressive symptoms (Bennett, 1994). This is further complicated by difficulties defining and measuring depression in this population due to overlap of symptoms (e.g., insomnia, changes in appetite and energy). Interestingly, certain psychosocial interventions (e.g., writing about stressful experiences, family therapy) have been shown to improve physical disease status in adults with asthma (Smyth, Stone, Hurewitz & Kaell, 1999) even in the absence of depression. This effect is thought to be mediated by the improvement of the immune response. Such studies could provide the foundation for examining potential mediators and moderators of treatment effect when co-morbid depression is present, as was the case for Amy, and suggests that psychosocial strategies to help her cope with her asthma may have had preventive effects on her depressive symptoms.
C. Psychosocial Factor
Cultural—Another often-neglected area in clinical practice is the appreciation of the role of cultural differences and similarities in the etiology, expression, and phenomenology of depressive disorders (Marsella, 1987). A number of risk factors have been associated with depression in African-American children, including higher levels of child-reported daily stress, poverty, teenage pregnancy, lack of maternal contact, low educational level of mother and/or head of household, high levels of family conflict, use of corporal punishment, and domestic violence (Marsella, 1987). Research also suggests that culture influences the manifestations of depressive symptoms in youth. For example, somatic complaints and interpersonal difficulties are common in depressed American Indian children, whereas cognitive and affective complaints characterize depressed European American children (Manson, Ackerson, Dick & Baron, 1990). An understanding of the cultural background of Amy’s family, the context within which her symptoms developed, and the family’s response to them are all important issues to consider.
Poverty—Although poverty has been shown to be a risk factor for juvenile depression, data are mixed regarding the link between social class and rates of depression and depressive symptoms in youth. There are virtually no data on the interaction of socioeconomic status and ethnicity with depressive symptoms/disorders and youth. Interestingly, the effect of low socioeconomic status may be more a function of being at the bottom of the social hierarchy and less due to absolute income levels or cultural differences (Goodman & Gottlib, 1999; Keating & Hertzman, 1999). The divorce-related change in the socioeconomic status of Amy’s mother may have additionally contributed to maternal unavailability (through work pressures) and may have the potential to indirectly affect Amy’s mental health outcome by limiting the family’s access to mental health care.
Cumulative Life Stressors—Life events are positively correlated with symptoms of depression, particularly when these events are severe, numerous, and/or related to key interpersonal relationships (Birmaher et al., 1996; Compas, Grant, & Ely, 1994; Garber & Hilsman, 1992; Williamson, Birmaher, Anderson, al-Shabbout & Ryan, 1995). Negative life events most likely to precipitate depression in adolescents relate to structural changes in the family (e.g., divorce) and rejection from peers (Bell-Dolan, Last & Strauss, 1990; Brent et al., 1993; Reinherz et al., 1993; Weller, Weller, Fristad & Bowes, 1991). Although most research suggests that depression is a familial disorder with strong genetic influences, environmental factors appear to account for the variance in liability to major depression (Sullivan, Neale & Kendler, 2000). The influence of environmental factors is highlighted in this case by the fact that while both Amy and her brother shared a family vulnerability for major depression and substance abuse, and may have shared a genetic vulnerability, Amy manifested depressive symptoms while her brother presented with substance abuse issues. Studies to date support a number of potential reasons for this differential expression of psychopathology in the two siblings. The cumulative presence, timing, and contextual threat level of negative life events (e.g., changes in family structure, social isolation from peers, or coping with asthma) may have been more etiologically relevant in inducing depression in Amy than in her brother. Alternatively, her brother’s less-inhibited temperament, increased cognitive maturity, and good athletic abilities may have been protective factors against depression.
D. Cognitive Style
Individuals with negative attributional styles, cognitive distortions, and social skill deficits tend to become hopeless and dysphoric, and they appear to be at higher risk for developing depression (Asarnow & Bates, 1988; Gladstone & Kaslow, 1995; Gotlib, Lewinsohn, Seeley, Rohde & Redner, 1993; Hammen & Zupan, 1984; Rudolph, Hammen, & Burge, 1994; Wagner, Rouleau, & Joiner, 2000). Children with maladaptive attachments to parents may develop unhealthy cognitive styles, including negative models of self and others, and poorly developed social and coping skills (Burge et al., 1997). Others have proposed that negative attributional styles and negative cognitions increase the risk of depression when prepubertal children experience stressful life events (Hammen, 1992; Hillsman & Garber, 1995). In the case of Amy, an awareness of factors that could induce or maintain her negative self-image (e.g., a learning disability preventing academic competence or social skill problems interfering with peer social competence) may help guide the target of psychosocial interventions.
Summary of Risk Factors
For Amy, factors such as an inhibited/anxious temperament, the absence of maternal emotional responsivity, prenatal exposure to tobacco, and genetic predisposition for depression could have primed her neurobiological reactivity to stress. Exposure to adversity during sensitive periods of brain development may have induced alterations in her perceptions and responses to environmental stressors, making her more vulnerable to react negatively to future stress (e.g., family conflict), particularly in the absence of effective coping models at home and increased genetic susceptibility for depression. It is important to note that any single risk factor may lead to a variety of different negative outcomes or may have no effect at all (Rutter, 1990). For example, evaluation of the effects of parental depression on offspring over a 10-year period revealed that offspring of depressed parents had higher rates of suicide, major depression, phobias, panic disorder and alcohol dependence, and lower levels of functioning at home, work, and within marriage and families than children with non-ill parents (Weissman, Warner, Wickremaratne, Moreau & Olfson, 1997). The specificity of negative outcomes may be enhanced when several risk factors are combined. Thus, in cases like Amy’s, it may be more important to address the multiplicity of risk factors in treatment rather than any single risk variable (Hammen, 1992; Rutter, 1979). Beardslee et al. (1996) developed an “adversity index” using a nonreferred sample of adolescents with affectively ill parents. They found that the combination of the duration of parental affective disorders, the number of parental non-affective diagnoses, and the total number of prior child psychiatric diagnoses predicted the onset of disorder in these adolescents over a 4-year period. Similar findings regarding the cumulative effects of risk factors in predicting outcomes in young children have been reported by Sameroff et al. (1987). Thus, the phenotypic expression of depression appears to be related to the interaction of genetic vulnerability, cognitive coping style, and psychosocial stress factors. In diagnostic considerations, it is important to identify malleable risks such as family communication, parenting style, adequate treatment of parental psychopathology, and adequate consideration of the presence of, or risk for, comorbid psychiatric, substance abuse, and medical conditions.
The science base clearly suggests several possible interventions that can address the variety of risk factors to better prevent and treat psychopathology in the child and the family. Yet, the science base is limited in terms of providing guidance as to the relative potency of these risk factors at different developmental periods, their specificity of effect, strategies to target such risks (e.g., sequence, timing and type of intervention), or determining how much of an effect is possible in light of the resources and sociocultural context of Amy’s family.
2. Phenomenology of Depression Across Development
If lasting solutions to these problems are to be achieved, research into the environmental and genetic interactions that bring about brain and behavioral development must develop in parallel with psychological and sociological solutions to the problems faced by children in our society. Knowledge pertaining to the neurobiological underpinnings of behavior and their relation to the etiology of mental disorders over the developmental trajectory will be fundamentally important in developing accurate diagnostic tools and early interventions.
Infancy to Middle Childhood
The importance of linking genetic, environmental and brain developmental factors during childhood is well-illustrated in the particular case of maternal depression, where negative effects on the child have been documented during both infancy (e.g., more fussy/difficult temperaments, delayed mental and motor development, and less secure maternal attachments) and toddlerhood (e.g., more negative reactions to stress and delayed acquisition of effective self-regulation strategies). Although early brain development is predominantly genetically determined, the determination of which synaptic connections will persist in the brain is environmentally regulated. Given that affect-regulation processes require maturation of the frontal lobes, a process that is not completed until adolescence, early mother-infant interactions are critical in helping the child acquire healthy self-regulation strategies. One aspect of maternal depression is the absence of these sensitive interactions between parent and young child. Some depressed mothers are withdrawn and disengaged; others are insensitive, intrusive, and sometimes angry (Cohn & Tronick, 1989). In the absence of experiences of external modulation of affect, the infant brain is unable to learn self-regulation of affect, part of the process of ontogenesis (development of self through self-regulation) (Glaser, 2000). The understanding of such brain-environment interactions could lead to earlier detection of maternal depression and to preventive psychosocial interventions that are better at targeting the mother-infant dyad.
The diagnosis of depression in infants and toddlers is compromised, as infants lack the cognitive and language skills necessary to self-reflect and report depressive thoughts and symptoms. Nevertheless, depressive-like states in infants and toddlers have been described in the literature. Distressed infants exhibit symptoms commonly associated with depression, including lethargy, feeding and sleep problems, irritability, sad or expressionless faces, and decreased affective responsivity, attentive behavior and curiosity (Carlson & Kashani, 1988; Field, 2000). Changes in these behaviors imply changes in underlying neural development, such as cell survival, neuron density, brain vascularization, neural connectivity, and neurochemical expression. It is interesting to speculate how identification of many of these behaviors during Amy’s infant years and consequent intervention with the mother-infant dyad may have altered the course of her depressive illness. Several studies have examined the outcome of such interventions for infants and children at high risk for developing such problems on the basis of the presence of depression in the mothers (Cicchetti, Rogosch & Toth, 2000; Field, 1998; Lyons-Ruth, Connell, Grunebaum & Botein, 1990; Sexson, Glanville & Kaslow, in press). Collectively, these studies found improved affective regulation, lower levels of salivatory cortisol, increased weight gain in treated infants, and improved cognitive functioning both in the short and long term (3 years) in treated toddlers.
Middle Childhood to Adolescence
It is important that depressive phenomenology and its treatment be considered in a developmentally appropriate context for this age group. For example, while there is a relatively stable pattern of depressive symptoms in 6- to 8-year-olds that includes prolonged unhappiness, decreased socialization, sleep problems, irritability, lethargy, poor school performance, accident-proneness, phobias, separation anxiety, and attention-seeking behaviors (Carlson & Kashani, 1988; Edelsohn, Ialongo, Werthamer-Lars, Crockett & Kellam, 1992), children at this age typically do not verbalize hopelessness and self-deprecation. In contrast, 9- to 12-year-olds who are more self aware often verbalize feelings of low self-esteem and helplessness when depressed (Carlson & Kashani, 1988; Weiss et al., 1992). More severe symptoms may also emerge at this time, such as suicidal ideation (Poznanski, 1982).
Other studies comparing the phenomenology of depression in child and adolescent samples indicate that the similarities in symptom expression exceed the differences (Mitchell, McCauley, Burke & Moss, 1988; Ryan et al., 1987). Both groups evidence somatic complaints, social withdrawal, hopelessness, and irritability. However, as a result of the cognitive developmental shift that accompanies formal operations, when compared with depressed elementary school children, depressed adolescents report more concern about the future and pessimism, worthlessness, and apathy, as demonstrated by Amy (Weiss et al., 1992). As adolescents mature, their self-reported symptoms seem to be more accurately correlated with a diagnosis of depression (Kazdin, French & Unis, 1983; Shain, Naylor & Alessi, 1990). The case illustrates the importance of using multiple informants, including the child’s report, when assessing internalizing symptoms. Although the family situation may have contributed to the parents’ lack of attunement to Amy’s depression, it is not uncommon to miss early signs of depressive symptoms due to young children’s limited ability to verbalize their hopeless thoughts and feelings, nor is it uncommon for their depressive symptoms to manifest themselves as irritability rather than sadness. In this case, Amy did not receive help until teachers at school noted a decline in her school functioning and her symptoms became more severe.
In conclusion, juvenile depression is a heterogeneous condition resulting from interactions between genetic, biological, and environmental factors at any given developmental period. Knowledge of underlying biological, cognitive, and social processes in normal development is critical in understanding the risks for the development of psychopathology in children. Understanding what leads to failures in the development of competence can aid in designing better preventive interventions and better treatment of depressive symptoms. Current treatment of juvenile depression generally neglects the following areas: comorbid diagnoses, academic and social functioning, and environmental stressors (Hammen, Rudolph, Weisz, Rao & Burge, 1999). Treatments need to be informed by and address the actual characteristics of depressed youngsters and their environments, which are often highly dysfunctional.
As Amy’s case illustrates, key developmental issues for depressed youth are that they often find themselves caught in environments that they cannot control, they may lack the cognitive skills to cope with such situations, and they may have long-standing additional problems contributing to ongoing difficulties in achieving developmentally important academic and interpersonal competence. The plasticity of the young brain suggests that appropriate early intervention may allow the child to return to a healthy developmental trajectory. The case raises questions about the importance of the timing of interventions. Would the course of Amy’s depression have been altered if the mother had received treatment for postpartum depression with subsequent improvement in her parenting capacity and emotional availability? Would Toddler-Parent psychotherapy, an intensive treatment to address attachment difficulties, have been as helpful in improving cognitive functioning as suggested in other at-risk toddlers (Cichetti et al., 2000)? Would family or marital therapy have been effective in helping to deal with the marital conflicts? Such interventions may have led to both behavioral improvement and normalizing underlying brain function. As the research evidence suggests, failure to make appropriate diagnoses or provide efficacious treatment regimens in a timely manner can result in early onset mood disorders that may derail development in very serious ways, with very high costs not only to the child but also to her family.
After evaluation by the psychologist, Amy, who was now almost 11 years old, was diagnosed with a new-onset major depression of moderate severity, a history of anxiety symptoms, and possibly a learning disability. Individual cognitive behavioral therapy (CBT) was initiated with a family component to educate parents about depression and help them parent Amy in a more unified, less conflict-laden manner. Several meetings were arranged with her school to develop an educational plan to help Amy recapture her academic functioning. At the end of this treatment, Amy felt significantly better and was functioning back at her baseline at school. She was also spending more time socializing with her friends. Residual symptoms of intermittent insomnia and a sense of worthlessness persisted. CBT sessions were continued on a monthly basis for 6 months, during which time Amy remained in remission. The family stopped coming to treatment after they had used up their 20 allowable visits under their insurance plan.
3. Psychosocial Treatment of Juvenile Depression
In contrast to the dearth of research on treatments for depression in infants and toddlers, a larger body of evidence exists regarding treatments of depression in middle childhood. At present, psychosocial treatments for depression in children under age 13 have been investigated in10 studies. Most of the studies have focused on cognitive behavioral approaches, with most finding favorable results, compared to a variety of comparison conditions in both school-based (Rehm & Sharp, 1996; Stark et al., 1987) and clinic-based (Kahn, Kehle, Jenson & Clark, 1990; Weisz, 1997) programs. For adolescent depression, CBT has been the most widely evaluated treatment and has been found to demonstrate success across modalities, in individual, group, and school-based treatment (Clarke et al., 1995; Lewinsohn, Clarke, Hops & Andrews, 1990; Reynolds & Coats, 1986). Interpersonal therapy (IPT) has also been shown to reduce depressive symptoms and improve social functioning in adolescents (Mufson, Weissman, Moreau & Garfinkel, 1999). IPT and CBT share many common components; both forms of therapy attempt to treat depressive symptoms in a problem-focused, time-limited manner with attention to engagement in activities, problem solving, and improvement of interpersonal relationships. Unlike CBT, however, IPT focuses primarily on addressing interpersonal conflicts, deficits, and themes rather than on changing cognitive patterns and errors. One recent study compared IPT, CBT, and wait-list control conditions in a sample of Puerto Rican adolescents. While both treatment groups showed improvement in depressive symptoms and social adaptation, the IPT group showed a greater improvement in self-esteem and social adaptation relative to the wait-list control group, suggesting that IPT may be more useful for teens whose depression either revolves around interpersonal issues or has adversely affected their social functioning (Rossello & Bernal, 1999). In clinical practice, access to IPT appears to be limited, as few clinicians are trained to use this modality.
Developmental factors in cognitive maturity and style may play a role in determining optimal clinical strategies for choosing a particular therapy modality. During pre-puberty, cognitive strategies include catastrophization, personalization, egocentric thinking with perceived causal responsibility for negative events, and absolutist thinking which may decrease cognitive flexibility (Weisz, Rudolph, Ranger & Sweeney, 1992). However, more superficial and less global/stable self-concepts may decrease vulnerability for prolonged depression. Throughout adolescence, cognitive processes undergo dramatic transformations that allow adolescents to handle and process more complex information. With increased ability for abstraction, recursive thinking, and an ability for mutual perspective taking, adolescents can understand the emotions of others, appreciate mixed or contradictory emotions, separate behavior and emotion, and understand the influence of experiences outside of immediate relationships as affecting emotions. In terms of cognitions and skill deficits during depression, cognitive distortions, negative self-concept, social skills deficits, passive or avoidant coping strategies, and increased focus on interpersonal schemas are more prevalent (Gladstone & Kaslow, 1995; Hammen & Rudolph, 1996; Weisz, Rudolph, Ranger & Sweeney, 1992).
In the case described, Amy may have been more susceptible than her older brother to certain cognitive errors during her middle childhood (e.g., catastrophization, personalization), and to certain aspects of depressive attributional style (e.g., attribution of negative events to internal, stable, and global causes), thus making her more vulnerable to developing depression. Although chronological age is often used to decide treatment modalities, the fact that a child uses cognitive processing styles characteristic of a particular age group may constitute more useful clinical data than a child’s age alone.
Therapeutic interventions may be further informed by knowledge about age-related changes in the importance of particular domains of self-cognition. For example, because acceptance and support from peers becomes increasingly important in late childhood and early adolescence, negative beliefs about one’s social competence may be strongly linked to depression at this stage, and interventions targeting such cognitions may be particularly beneficial. More broadly, Harter (1988) has suggested that successful treatment depends not only on knowledge of a child’s perceived competencies across domains, but also on the affective salience the child assigns to the various domains. Treatment must be sensitive to age differences in focus, meaning, and impact of self-descriptive schemes across time in terms of physical appearance, athletic ability, peer acceptance, and academic ability. For example, in adolescent depression, studies suggest depression onset may be associated with social competence deficits and with poor peer relationships.
Evidence, however, is mixed with regard to three issues: specificity (whether deficits are linked specifically to depression or more generally to psychopathology); state-dependence (whether deficits are evident only during states of depression or are characteristic of depression-prone kids even when they are not depressed); and co-morbidity (whether low levels of social competence in depressed groups are accounted for by subgroups who also meet criteria for other diagnoses, especially conduct disorder and attention deficit disorder). These three issues remain unresolved for academic and behavioral competence as well, but they still must be considered in comprehensive treatment plans. In Amy’s case, a variety of factors other than depression (e.g., parental criticism, family conflict, anxious predisposition, poor social skills, learning problems) likely contributed to the maintenance of her sense of poor self-concept.
A few studies examining family involvement in treatment also emphasize the importance of adjusting interventions in developmentally appropriate ways. In depressed elementary school children, supplementation of individual CBT with monthly family meetings was shown to enhance outcome (Stark, Rouse & Livingston, 1991), but this was not found to be the case for depressed youth (Lewinsohn et al., 1990; Clarke, Rohde, Lewinsohn, Hops & Seeley, 1999). Multi-Family Psychoeducational Groups (MFPG) is a recently developed family-based approach for treating depressed adolescents, aimed at improving family functioning by reducing the burden on family caregivers in a manner more sensitive to normal individuation-separation issues integral to adolescence. Preliminary results suggest that MFPG is associated with improved family climate, increases parents’ understanding of the disorders, and the ability to use appropriate resources (Fristad, Gavazzi & Soldano, 1998).
In one of the only studies that included a family therapy condition for adolescents with depression, individual CBT was found to be more effective than individual nondirective supportive therapy (NST) or systemic behavioral family therapy (SBFT) post-treatment (Brent et al., 1997). An exclusive focus on recovery rates immediately after treatment, however, may obscure the benefits of SBFT, which is designed to bring about systemic rather than simply individual change, and may have a slower and subtler effect on depressive symptoms than CBT. Thus, although treatment response was significantly more rapid and remission rates were significantly higher in the CBT group than in the SBFT group (Brent et al., 1997), at 24 months post-treatment, recovery rates did not differ significantly among CBT, SBFT and NST groups (Birmaher et al., 2000). Participant characteristics were better predictors of treatment outcome; individuals who were less depressed at baseline and those who reported lower levels of parent-child conflict, hopelessness, and cognitive distortion were more likely to recover over time following treatment.
In summary, studies of CBT, IPT, and treatments involving families in developmentally appropriate ways indicate that these short-term therapies show promise as efficacious treatments for depression. Each, however, appears to confer a slightly different set of benefits on recipients. Research that matches treatment protocols with participant characteristics may be an important next step in evaluating treatment efficacy. IPT, for example, may be the better treatment for teens whose depression is associated with disrupted relationships, as it has been shown to affect social functioning as well as depressive symptomatology. SBFT or MFPG, in contrast, may be preferable when it is clear that family behavior patterns support the development of depression or when multiple family members are depressed.
Research findings suggest that the impact of comorbid diagnoses like anxiety merit additional clinical attention. Brent and colleagues (1998) found that comorbid anxiety was among the primary predictors of poor outcome at the end of treatment. Given that rates of comorbidity between depression and other disorders are high (Brady & Kendall, 1992), it is critical that researchers explore strategies that effectively address problems extending beyond depression. Kendall, Kortlander, Chansky & Brandy (1992) outlined a framework for designing treatment protocols targeting comorbid depression and anxiety in children, which is largely applicable to adolescents as well. In particular, they recommended flexible use of manualized treatment programs so that therapy can be geared to the individual client and his or her unique constellation of symptoms. Additionally, Kendall and colleagues suggest adaptations of traditional cognitive behavioral techniques (e.g., teaching problem-solving skills) that address issues raised by both anxiety and depression.
It is also critical for clinicians to consider such variables as gender and ethnicity in treatment studies (Rosello & Bernal, 1999). Not surprisingly, given the gender difference in depression prevalence during adolescence, samples in most of the treatment studies to date have been weighted toward females. At least one gender-targeted treatment study, evaluating a family treatment protocol designed for depressed African-American girls with a history of abuse, is currently under-way (Kaslow et al., in press). In terms of culture, clinicians must be aware that depression, particularly suicidal depression, may manifest differently in traditionally underserved populations such as African American, Asian American, Latino, and Native American adolescents than it does in European American teens (e.g., Rotheram-Borus & Trautman, 1988; Summerville, Abbate, Siegel, Serravezza & Kaslow, 1992). Understanding gender and cultural variations may be useful in helping clinicians target treatments to address potential for suicide or other functional impairments.
Amy appeared to do well without mental health intervention over the next year lbut at age 13 she began to experience depressive symptoms and again showed a decline in her academic functioning and social interactions. She was re-evaluated by her initial treating psychologist, and the onset of her current depression appeared to be related to a break-up with her boyfriend of 3 months. On closer examination of her peer relationships, Amy was found to have a fear of intimacy and difficulty keeping friends. She endorsed severe neurovegetative symptoms and extreme worthlessness, hopelessness, and suicidal ideation, stating she wanted to kill herself “to escape” but didn’t have a specific plan. She denied alcohol use but had started smoking with peers, which resulted in “increased energy” and feeling “jittery.” Weekly group CBT sessions were initiated to work on coping strategies with peers. However, given worsening depressive symptoms over the next month, the therapist initiated an evaluation by a child psychiatrist to augment treatment with an antidepressant. Fluoxetine (Prozac), a selective serotonin uptake inhibitor (SSRI), was initiated, after some reluctance on the part of Amy and her mother. Eight weeks later, she reported feeling significantly better and did not want to continue further therapy because “it interfered too much with her social life.” She did agree to come to the psychiatric clinic every month for medication checks, and admitted to her psychiatrist that she felt somewhat embarrassed about receiving psychiatric treatment and feared that her friends would think she is “crazy.”
4. Pharmacological Treatment of Juvenile Depression
Psychopharmacologic treatment studies using tricyclic antidepressants in childhood depression have generally been disappointing due to high placebo response rates and/or the lack of significant differences between active treatment and placebo. Of the double-blind placebo controlled studies in children (Connors & Petti, 1983; Geller, Cooper, McCombs, Graham & Wells, 1989; Hughes, Preskorn, Wrona, Hassanein & Tucker, 1990; Kashani, Shekim & Reid, 1984; Petti & Law, 1982; Preskorn, Weller, Hughes, Weller & Bolte, 1987; Puig-Antich et al., 1987) using tricyclic antidepressants, only one study, Preskorn et al. (1987), found statistical significance evaluating symptom reduction on an outcome variable. Factors such as high placebo response rates and small sample sizes may have contributed to the poor response rates.
Recent focus has shifted to the use of selective serotonin reuptake inhibitors (SSRI’s) in adolescent depression, based mainly on reports of efficacy in adults with major depression (Greenberg, Bornstein, Zborowski, Fisher & Greenberg, 1994), the benign side-effect profile, and low lethality in overdose. While a double-blind, placebo-controlled study of 40 adolescents with major depression did not find any significant differences between placebo and fluoxetine (Simeon, Dinicola, Ferguson & Copping, 1990), more recent studies with much larger samples and lower overall placebo responses have suggested response rates comparable to those reported in adults. Several open studies have reported 70 to 90 percent response rates to fluoxetine or sertraline for treatment of adolescents with major depression (DeVane and Sallee, 1996). An 8-week double blind study of treatment of depression in a large sample of youth showed that both children and adolescents responded significantly better to fluoxetine than to placebo (56% vs. 33%) (Emslie et al., 1997). In addition, a multicenter, double-blind, placebo-controlled study examined the efficacy of paroxetine and imipramine in 275 adolescents with unipolar depression (Keller, Ryan, Birmaher et al., 1998). Youth treated with paroxetine had a statistically greater improvement over those treated with placebo in global functioning and depression scores at the end of study, and there was a remission of depressive symptoms.
Better study paradigms, including augmentation strategies, multiple medication strategies to manage comorbid disorders, and the use of algorithmic treatments, are needed to help guide clinical practice. It is interesting that from 1996 to 1997, children between the ages of 6 and 18 received 792,000 prescriptions for SSRI’s to treat depression (Hoar, 1998). This pattern is based on relatively few studies, with relatively modest effects, as noted above. For this reason, a multi-site study was completed to develop an algorithm for treating major depression, based on consensus among academic clinicians, researchers, practicing clinicians, administrators, consumers, and families. The process initially addressed strategies of treatment and tactics to implement the strategies, including medication augmentation and medication combinations (Hughes et al., 1999).
In sum, most clinical trials of antidepressants conducted to date have been based on open studies and/or relatively small sample sizes, with conclusions about their safety, efficacy, and effectiveness based on group-means comparisons. From a clinical utility perspective, separate and distinct algorithms for management of the same illness or disorder may be necessary for different patient populations or different types of treatment environments. In addition, unique developmental characteristics, the presence of comorbid symptoms, and the role for nonmedication alternatives need to be considered. For example, a study in adults found that treatment with combined medication (nefazodone) and psychotherapy (cognitive behavioral analysis system) was more efficacious than treatment alone for chronic major depression, suggesting that combined treatments are superior (Keller et al., 2000).
The mechanisms by which antidepressants work to address depressive symptoms are not well understood. While both noradrenergic and serotonergic neurotransmitter systems have been implicated in the etiology of major depression, their role must be understood in the developmental context of how these systems mature during childhood and adolescence. For example, lack of response to tricyclic antidepressants in younger cohorts could be secondary to later maturation of noradrenergic brain substrates (Murrin, Gibbens & Ferrer, 1985). Dopamine beta-hydroxylase, the enzyme involved in the conversion of dopamine to noradrenaline, increases in activity from birth to about age 8 (Weinshilboum, 1983). Such developmental differences are key in understanding the molecular effects of antidepressants. Animal studies have begun to characterize the subcellular actions of antidepressant treatments such as activation of the cyclic adenosine monophosphate (cAMP), which in turn leads to regulation of specific target genes (e.g., increased expression of brain-derived neurotrophic factor in the hippocampus and cerebral cortex) (Duman et al., 1997). Clinical studies also provide evidence for atrophy and cell death in the hippocampus as well as the prefrontal cortex in response to stress and impaired function of these neurons in depression (Bowen, Najlerahim, Procter, Francis & Murphy, 1989; Sapolsky, Uno, Rebert & Finch, 1990; Rajkowska et al., 1999). Thus, it is possible that various antidepressant treatments could limit these adverse cellular events that might be best conceptualized as a loss of neuronal plasticity in the developing nervous system of children and adolescents. The clinical utility of these research findings lies not only in their potential for developing safer and more effective treatments for children whose nervous systems are still developing, but also, as in Amy’s case, for educating her and her family about the potential benefits of antidepressant treatment at both the behavioral and the brain level.
Amy appeared to do better over the next year, but then her progress appeared to come to a halt. During the summer of her sophomore high school year when Amy was 16, her mother made a decision to move from a house to a small apartment in another neighborhood, due to significant financial stress. Amy was extremely upset by the move, became increasingly anxious about how her friends might perceive her living situation, and refused to socialize or engage in activities she used to enjoy. She felt so dejected that she impulsively attempted suicide by ingesting 30 Tylenol tablets. She became scared of dying and told her mother, who immediately took her to the emergency room. Given the severity of her depression and the lethal intent of her attempt, she was admitted to an adolescent psychiatric inpatient unit for 4 days. During this stay, she received intensive individual therapy and family work and was switched from fluoxetine to serzone (Nefazodone), a newer generation of antidepressant with properties of both an SSRI and a tricyclic antidepressant (TCA), to target both depressive and anxiety symptoms. Amy and her mother continued with outpatient treatment over the next 6 months until her mother’s work conflicts made it difficult for them to continue.
5. Suicide and Social Connectedness
Suicide is the third leading cause of death among teenagers; nearly half of these suicides are associated with depression. Several lines of evidence indicate that suicidal behavior is linked to a lack of social connectedness. Suicidal risk is associated with interpersonal conflicts or losses (e.g., romantic break-ups and parental divorce) in adolescents (Brent et al., 1993; Gould, Fisher, Parides, Flory & Shaffer, 1996). Another phenomenon reported in the adolescent age group is the clustering of teen suicides in close temporal and geographic proximity to successful suicide attempts, likely due to imitative behavior (Gould, 1990; Gould & Shaffer, 1986; Phillips & Carstensen, 1986). In the case of Amy, these findings argue for careful observation of social behavior in teens predisposed to depression. Other known risk factors for suicide that did not appear to be present for Amy include substance abuse, lifetime history of abuse, availability of a gun, and past suicide attempts.
Primate studies suggest that the activity of the serotonergic system helps regulate social interactions and that social interactions can affect serotonergic activity (Raleigh, McGuire, Brammer & Yuwiler, 1984). For example, a dominant monkey isolated from his social group can experience a decrease in whole blood serotonin, while a submissive monkey can be made dominant with treatment using drugs such as fluoxetine and tryptophan, which enhance serotonin function (Rogeness & McClure, 1996). These findings offer further indirect support for using serotonergic antidepressants to treat adolescent depression and improve social functioning in this developmentally vulnerable period.
As adolescents transition to early adulthood, they are faced with a number of major environmental changes (e.g., leaving home, school changes, employment) (Feehan, McGee, Williams & Nada-Raja, 1995). Petersen and colleagues (1993) reported that the accumulation of simultaneous changes is associated with increased risk for depression. The risk of depression and suicidality was further increased when prepubertal children with social skill deficits entered adolescence (Garber & Hilsman, 1992; Marton & Kutcher, 1995; Reinecke, 2000; Sadowski & Kelley, 1993). The association between social problem-solving and suicidality among adolescents appeared, however, to be mediated by more directed effects of negative mood and negative cognitions (Reinecke, 2000). It is interesting to speculate whether more careful attention to the social consequences of a major move during high school for Amy, a teen with a history of social difficulties, may have prevented her suicide attempt.
In terms of suicide prevention, pediatricians, in collaboration with psychiatrists and other mental health professionals, can make an important contribution to the mental health of children and adolescents through identification, referral, and management of depressed and suicidal youth (Brent et al., 1993). Clinical training must emphasize diagnostic proficiency, assessment of the entire family unit, and availability of firearms in the home. With respect to changes in service delivery, treatment is recommended for the entire family unit, with a special focus on treatment of psychiatric and substance abuse problems in the same setting, and the need for a continuum of intensity of care from inpatient to outpatient (Rotheram-Borus et al., 1996). With respect to policy changes, one suicide prevention study recommended parity of mental and physical health insurance coverage, screening for psychiatrically at-risk youngsters in schools and physician offices, and gun control laws to restrict access to handguns (Brent & Perper, 1995).
Over the next 3 years, Amy remained in remission. Given her recurrent depression, history of comorbid anxiety, and family history of depression, her psychiatrist decided to continue her medication even with her sustained remission. Although she did well academically during her sophomore year at a community college, she struggled to maintain peer relationships for any sustained period.
6. Depression Course and Outcome
The continuity of depressive episodes from childhood to adulthood has been studied longitudinally in clinic (Harrington et al., 1990; Kovacs, 1996; Weissman et al., 1999a; 1999b), community (Lewinsohn et al., 2000; Pine et al., 1998; Rueter et al., 1999), and high-risk populations (Weissman et al., 1997). Data on adolescent depression quite consistently point to the continuity of depression into adulthood, with varying degrees of association across studies. Stronger rates of recurrence are found in clinical settings (70 to 80 percent, Kovacs, 1996) relative to community-based settings (less than 50 percent, Lewinsohn et al., 2000; Pine et al., 1998). By contrast, data on pre-pubertal depression have not been as consistent. Pre-pubertal depression shows as strong or stronger associations with other disorders as it does with major depression, including bipolar disorder, conduct disorders and substance use disorders (Harrington, 2001; Weissman et al., 1999b).
The mean duration of an untreated depressive episode is 7 to 9 months for clinically-referred children, and 1 to 2 months for community samples. While approximately 90 percent of major depressive episodes remit within 2 years after onset, up to 10 percent have a more protracted course (Birmaher et al., 1996; Kovacs et al., 1984a). Factors that appear to predict a protracted course include depression severity, comorbid psychiatric conditions, exposure to negative life events, parental psychopathology and poor psychosocial functioning (Birmaher et al., 1996, Lewinsohn, Rohde, Seeley, Klein & Gotlib, 2000; Sanford et al., 1995). Even those adolescents who recover from an acute depressive episode continue to manifest subclinical depressive symptoms, negative attributions, pessimism, impaired interpersonal relationships and increased physical problems (Garber et al., 1988; Harrington et al., 1990; Kovacs, Feinberg, Crouse-Novak, Paulauskas & Finkelstein, 1984a). Depression in young adolescent females has been strongly associated with teenage pregnancy, higher rates of marriage and subsequent marital dissatisfaction, increased risk of tobacco use, and more medical problems. In addition, longitudinal studies have shown that the probability of recurrence is 6 percent by two years after remission, and climbs to 70 percent after 5 years (Hammen, Burge, Burney & Adrian, 1990; Kovacs et al., 1984b; Lewinsohn, et al., 1999, 2000; Rao et al., 1995). Predictors of recurrence of depression include earlier age of onset, number of previous episodes, severity of index episode, psychosis, presence of psychosocial stressors and presence of comorbid psychiatric disorders. In addition to increased severity and duration of depressive episodes, the presence of comorbid disorders has been correlated with frequency of suicidal behaviors, functional outcome, response to treatment, and utilization of health services. In a community sample of formerly depressed adolescents, factors related to the recurrence of major depressive disorder in young adulthood included female gender, multiple depressive episodes in adolescence and elevated borderline personality symptoms (Lewinsohn et al., 2000). Conflict with parents in females independently predicted recurrent major depressive disorder. Comorbid anxiety and substance abuse disorders in adolescence and elevated antisocial personality disorder symptoms independently distinguished adolescents who developed recurrent major depression comorbid with non-mood disorder from those who developed pure major depressive disorder.
Amy manifested many of the risk factors for a protracted and recurrent course for her depression. Over time, it is impossible to determine the extent to which neurobiological vulnerability to stress, poorly developed coping skills, psychosocial deficits, and other contextual issues contributed to her risk for recurrent depression. A better understanding of the potency of such risks and how they interact with one another to rekindle a depressive episode have important implications for clinicians in developing targeted interventions that help individuals with chronic or intermittent depression manage their disorder with minimal interference of functioning. The limited current research evidence suggests that continued monitoring of individuals like Amy for depression and associated problems as they transition into adulthood and onward is warranted, including identifying ways to prevent further intergenerational transmission of depression.
7. Dissemination of Services and Access to Care and Prevention
Research in the area of serious emotional problems in children and adolescents supports the view that effective mental health services should be family-based, individualized, and multifaceted. In the case of juvenile depression, studies show consistent, serious problems associated with characteristics of the youth, their family, peer relations, and broader ecological contexts (Birmaher et al., 1996). Yet research focused on intervention development to date often fails to take into account larger contextual issues that influence treatment outcomes. In particular, service context and factors that influence family engagement in treatment have received limited attention. The effectiveness of services, no matter what they are, may hinge less on the particular type of service, and more on “how, when, and why families or caregivers are engaged in the delivery of care” (Burns, Hoagwood & Mrazek, 1999). Evidence-based services are not routinely available. There are long waiting lists even for existing services, and restrictions in mental health coverage are common. Recent evidence presented at the Surgeon General’s Conference on Children’s Mental Health (U.S. Public Health Service, 2000) indicated substantial disparities in access to specialty mental health care (Wells, unpublished data). Racial, ethnic, and cultural differences influence the expression and identification of the need for services, quality of care, referral bias or access to appropriate care, the diagnostic process, and hence, subsequent care and health outcomes. Insurance status also predicted outcome, with the uninsured having the least access. As seen in the case of Amy, parental availability for treatment due to work commitments, insurance limitations, financial constraints, stigma, and the availability of evidence-based care are common barriers in accessing adequate treatments for their children.
Mental health programs for children and adolescents need to draw from the adult literature on how to disseminate effective treatment and collaborative care models. In adult patients, quality improvement programs in managed care practices for depressed primary care patients have been found to improve quality of care, health outcomes, and employment (Wells, 2000). While such improvement was small, it could reflect substantial societal impact when accumulated nationally. The dissemination trial is similar to a social experiment in that it replicates naturalistic practice conditions including usual care providers and full choice of treatments.
Evidence for the poorer prognosis of early-onset depression suggests that more focus on preventive programs targeting infants, children and adolescents at risk for future depressive episodes are needed. Studies designed to intervene with depressed mothers at various points in their children’s development are needed. Several NIMH-funded studies are currently underway: one focusing on the perinatal period (Zayas, MH57936); one on postpartum depression (O’Hara, MH50524); one on infants of depressed mothers (Field, MH46586); one on toddlers of depressed mothers with demonstrated beneficial effects on cognitive development (Cicchetti, MH45027; Cicchetti et al., 2000); and three targeting older children and adolescents (Diamond, MH57977; Garber, MH57822; Riley, RO1MH58384). One preventive intervention has demonstrated some success in preventing depression among at-risk adolescents (with subclinical symptoms) using school-based cognitive behavioral programs (Clarke et al., 1995). Interventions selectively targeting adolescents with a family history of affective disorder have also demonstrated some beneficial effects (Beardslee et al., 1997). Ways to assess the viability of such programs in service settings and their cost-effectiveness once adapted for widespread dissemination and implementation are critical in light of the chronic and costly nature of juvenile-onset depression. It is interesting to speculate how the availability of such programs may have altered the trajectory of Amy’s illness course.
8. Summary
Amy’s case emphasizes the critical interplay among genetic or biological predisposition and child characteristics, family factors, and the broader social context in the development of mental disorders. It further illustrates the importance of understanding developmental processes in child mental health treatment, prevention, and services. Clearly, a scientific knowledge base is available to guide clinical decision-making. It is equally clear that this knowledge base is uneven.
Amy’s case demonstrates how a more integrated approach, which combines basic neuroscience (pharmacological, genetic) and behavioral and prevention research knowledge with developmental processes and contextual issues, is critical in understanding, preventing, and treating childhood depression. A major barrier to developing more effective early interventions (and, ultimately, preventive efforts) for depression is the lack of understanding of the etiology, pathophysiology, and mechanisms underlying affect dysregulation and negative cognitions. Cognitive and biological theories of depression remain relatively isolated (Weissenberger & Rush, 1983). In cognitive models, adolescent depression is characterized by negative cognitions (Laurent & Stark, 1993). Diathesis-stress models of depression propose that depressive etiology is found in the activation of latent depressive schema by stressors, such as physical illness (Burke & Elliott, 1999; Garber & Hilsman, 1992). The second type of model links clinical depression to altered neurobiology (e.g., HPA axis dysfunction, sleep changes, neurochemical changes) (Armitage, Emslie, Hoffmann, Weinberg, Kowatch, Rintelmann, & Rush, 2000; Dahl, 1992; Rao et al., 1996; Williamson et al., 1995) and implicates certain brain regions (e.g., the prefrontal cortex) (Drevets, 2000). The interaction between the neurobiology and negative cognitions is complex and not understood. Clearly, a better understanding of the pathophysiology, etiology, and mechanisms of risks leading to depression may help clinicians identify critical windows of opportunity for targeting and adjusting the intensity, type, and duration of treatment to increase the likelihood of Amy’s optimal functioning. Further, the recognition that so many children with mood disorders, like Amy, have additional diagnoses including anxiety disorder, learning disability, and substance abuse disorders, suggests that the current classification system may have set boundaries between disorders in a way that does not reflect what goes wrong in the brain.
The episodic and chronic nature of childhood onset depression indicates that we need to better understand the relative potency of risks and protective factors and the timing of their effects. At the same time, identifying the mechanisms by which various factors at the individual, familial, sociocultural, and organizational levels interact to influence the etiology and course of illness over time is a critical next step in child and adolescent mental health. In Amy’s case, knowledge about risks and protective factors was useful in identifying her as a child at high risk. Such knowledge must be augmented by research that determines the mode of genetic-psychosocial transmission of depression across the life span so that clinical practice can be guided to effectively prevent her illness, or the onset of comorbid conditions and more severe impairments. Longitudinal assessments of risks factors spanning infancy, childhood and adolescence that examine genetic, cognitive, interpersonal and other contextual processes associated with depression risk and course can help identify targeted opportunities for intervention throughout the developmental trajectory.
To date, we are still excessively reliant on CBTs, which have been shown to be efficacious mainly in adults. The effectiveness of such therapies in older children is equivocal and clearly inappropriate for young children. Although cognitive behavioral treatments make the assumption that altering cognitions leads to reduced depression, most fail to provide evidence on (a) whether cognitions were in fact altered, (b) whether changes in depressive symptomatology were mediated by changes in cognition, or (c) any other processes that may have operated as mediators of change. This suggests that considerable work will be needed to bring research designs into synchrony with our need to understand causal mechanisms by which psychotherapy for depression produces effects.
Although several researchers have included family-based interventions for treating childhood depression, the effectiveness of such therapies has yet to be rigorously examined. It is also critical that we begin to apply what we know about the developmental processes involved in functional brain maturation and the regulation of cognitions, emotions, and mood to design developmentally sensitive psychotherapies for children and adolescents. Researchers must find ways of directly assessing the developmental dimensions of interest rather than relying on assumptions about where children fall on those dimensions, based on children’s chronological age alone.
Given that childhood-onset depression is often chronic, intermittent, and comorbid with other disorders, intervention studies must go beyond the typical short-term trials and address problems beyond depressive symptoms. The frequent and increasing use of psychotropics to treat childhood depression in clinical practice, despite limited evidence of its safety or efficacy, points to the need to better understand the long-term impact (beneficial or detrimental) of acute and chronic exposure to pharmacological agents on brain development. The reluctance of parents like Amy’s to consent to medication treatment is understandable, given the limited science base. To this end, animal models are critical in advancing our knowledge about the development of the circuits that underlie emotion, brain-behavior relationships, and the mechanisms of drug action.
It is critical to note that the current research base is largely developed using group-means comparisons derived from studies on subpopulations, and in settings that may not be readily generalized to many real-world settings. Conceptual frameworks and research paradigms that recognize individual differences (e.g., vulnerabilities and protective factors) and contextual variables (e.g., family context, cultural factors, service settings) are needed to increase the usability of the science base by clinicians in practice. In Amy’s case, when the use of evidence-based CBT treatments or medications result in limited benefits, understanding the individual factors that may moderate or mediate their effectiveness will be important in guiding clinical decisions to adjust or augment treatment accordingly.
This case also illustrates commonly encountered difficulties in access to mental health treatment. Multiple opportunities for prevention and intervention were missed from the time even before Amy was born. The lack of availability or the difficulty that pregnant women and their children have in accessing mental health treatments needs to be better understood in the larger organizational and sociopolitical context. There is a clear need to increase the science base on how to develop treatments that are transportable into real-world settings so that they can be disseminated and implemented with fidelity in a variety of settings. As a step forward in bridging the gaps among research, practice, and policy, researchers must work not only across disciplines to advance the science base, but they must also ensure that their research findings are ultimately usable in real-world settings. To do so, the clinical utility of research must be considered at the very start of any research endeavor, be it basic, intervention, or services research. Further, public and private efforts are needed to ensure that current resources are utilized in ways that increase the likelihood that science-based interventions and services are positioned permanently within communities to provide adequate care over time to children and their families.
References for Appendix B
Armsden, G.C., McCauley, E., Greenberg, M.T., Burke, P.M., & Mitchell, J.R. (1990). Parent and peer attachment in early adolescent depression. Journal of Abnormal Psychology, 18(6): 683–97.
Angold, A., Costello, E.J., & Worthman, C.M. (1998). Puberty and depression: The roles of age, pubertal status and pubertal timing. Psychological Medicine, 28(1): 51–61.
Armitage, R., Emslie, G.J., Hoffmann, R.F., Weinberg, W.A., Kowatch, R.A., Rintelmann, J., & Rush, A.J. (2000). Ultradian rhythms and temporal coherence in sleep EEG in depressed children and adolescents. Biological Psychiatry, 47(4): 338–50.
Asarnow, J.R., & Bates, S. (1988). Depression in child psychiatric inpatients: Cognitive and attributional patterns. Journal of Abnormal Child Psychology, 16(6): 601–15.
Beardslee, W.R., Keller, M.B., Seifer, R., Lavori, P.W., Staley, J., Podorefsky, D., & Shera, D. (1996). Prediction of adolescent affective disorder: Effects of prior parental affective disorders and child psychopathology. Journal of the American Academy of Child & Adolescent Psychiatry, 35(3): 279–88.
Beardslee, W.R., & Podorefsky, D. (1988). Resilient adolescents whose parents have serious affective and other psychiatric disorders: Importance of self-understanding and relationships. American Journal of Psychiatry, 145(1): 63–9.
Beardslee, W.R., Versage, E.M,. & Gladstone, T.R.G. (1998). Children of affectively ill parents: A review of the past 10 years. Journal of the American Academy of Child & Adolescent Psychiatry, 37(11): 1134–1141.
Beardslee, W.R., Versage, E.M., Wright, E.J., Salt, P., Rothberg, P.C., Drezner, K., & Gladstone, T.R. (1997). Examination of preventive interventions for families with depression: Evidence of change. Development and Psychopathology, 9(1): 109–30.
Beasley, P.J., & Beardslee, W.R. (1998). Depression in the adolescent patient. Adolescent Medicine, 9 (2): 351–62, vii.
Bell-Dolan, D.J., Last, C.G., & Strauss, C.C. (1990). Symptoms of anxiety disorders in normal children. Journal of the American Academy of Child and Adolescent Psychiatry, 29(5): 759–65.
Bennett, B. (1994). Depression among children with chronic medical problems: A meta-analysis. Journal of Pediatric Psychology, 19: 149–169.
Birmaher, B., Brent, D.A., Kolko, D., Baugher, M., Bridge, J., Holder, D., Iyengar, S., & Ulloa, R.E. (2000). Clinical outcome after short-term psychotherapy for adolescents with major depressive disorder. Archives of General Psychiatry, 57(1): 29–36.
Birmaher, B., Ryan, N.D., Williamson, D.E., Brent, D.A., Kaufman, J., Dahl, R.E., Perel, J., & Nelson, B. (1996). Childhood and adolescent depression: A review of the past 10 years. Part I. Journal of the American Academy of Child and Adolescent Psychiatry, 35: 1427–1439.
Bowen, D.M., Najlerahim, A., Procter, A.W., Francis, P.T., & Murphy, E. (1989). Circumscribed changes of the cerebral cortex in neuropsychiatric disorders of later life. Proceedings of the National Academy of Science, 86: 9504–9508.
Brady, E.U., & Kendall, P.C. (1992). Comorbidity of anxiety and depression in children and adolescents. Psychological Bulletin, 111(2): 244–55.
Brent, D.A., Holder, D., Kolko, D., Birmaher, B., Baugher, M., Roth, C., Iyengar, S., & Johnson, B.A. (1997). A clinical psychotherapy trial for adolescent depression comparing cognitive, family, and supportive therapy. Archives of General Psychiatry, 54(9): 877–85.
Brent, D.A., Kolko, D.J., Birmaher, B., Baugher, M., Bridge, J., Roth, C., & Holder, D. (1998). Predictors of treatment efficacy in a clinical trial of three psychosocial treatments for adolescent depression. Journal of the American Academy of Adolescent and Child Psychiatry, 37(9): 906–14.
Brent, D.A., & Perper, J.A. (1995). Research in adolescent suicide: Implications for training, service delivery, and public policy. Suicide and Life Threatening Behavior, 25(2): 222–30.
Brent, D.A., Perper, J.A., Moritz, G., Allman, C., Friend, A., Roth, C., Schweers, J., Balach, L., & Baugher, M. (1993). Psychiatric risk factors for adolescent suicide: A case-control study. Journal of the American Academy of Child & Adolescent Psychiatry, 32: 521–529.
Brooks-Gunn, J., & Warren, M.P. (1989). Biological and social contributions to negative affect in young adolescent girls. Child Development, 60(1): 40–55.
Burbach, D.J., Kashani, J. H., & Rosenberg, T.K. (1989). Parental bonding and depressive disorders in adolescents. Journal of Child Psychology & Psychiatry & Allied Disciplines, 30(3): 417–429.
Burge, D., Hammen, C., Davila, J., Daley, S.E., Paley, B., Lindberg, N., Herzberg, D., & Rudolph, K.D. (1997). The relationship between attachment cognitions and psychological adjustment in late adolescent women. Developmental Psychopathology, 9(1): 151–67.
Burke, P., & Elliott, M. (1999). Depression in pediatric chronic illness: A diathesis-stress model. Psychosomatics, 40: 5–17.
Burns, B.J., Hoagwood, K., & Mrazek, P.J. (1999). Effective treatment for mental disorders in children and adolescents. Clinical Child and Family Psychology Review, 2(4): 199–254.
Caldji, C., Tannenbaum, B., Sharma, S., Francis, D., Plotsky, P.M., & Meaney, M.J. (1998). Maternal care during infancy regulates the development of neural systems mediating the expression of fearfulness in the rat. Proceedings of the National Academy of Sciences, 28;95(9): 5335–40.
Carlson, G.A., & Kashani, J.H. (1988). Phenomenology of major depression from childhood through adulthood: Analysis of three studies. American Journal of Psychiatry, 145(10): 1222–5.
Cicchetti, D. NIMH Grant Number MH45027, Preventive Interventions—Toddlers of Depressed Mothers.
Cicchetti, D., & Rogosch, F.A. (1997). The role of self-organization in the promotion of resilience in maltreated children. Development and Psychopathology, 9(4): 797–815.
Cicchetti, D., Rogosch, F.A., & Toth, S.L. (2000). The efficacy of toddler-parent psychotherapy for fostering cognitive development in offspring of depressed mothers. Journal of Abnormal Child Psychology, 28(2): 135–48.
Clarke, G.N., Hawkins, W., Murphy, M., Sheeber, L.B., Lewinsohn, P.M., & Seeley, J.R. (1995). Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of a group cognitive intervention. Journal of the American Academy of Child and Adolescent Psychiatry, 34: 312–321.
Cohn, J.F., & Tronick, E. (1989). Specificity of infants’ response to mothers’ affective behavior. Journal of the American Academy of Child & Adolescent Psychiatry, 28(2): 242–8.
Cole, D.A., & McPherson, A. E. (1993). Relation of family subsystems to adolescent depression: Implementing a new family assessment strategy. Journal of Family Psychology, 7(1): 119–33.
Compas, B.E., Grant, K.E, & Ey, S. (1994). Psychosocial stress and child and adolescent depression: Can we be more specific? In Reynolds,
W.M. & Johnston, H.F. (Eds) Handbook of depression in children and adolescents : Issues in clinical child psychology. pp. 509–523. New York, NY: Plenum Press. xv, 616 pp.
Connors, C.K., & Petti, T. (1983). Imipramine therapy of depressed children: Methodological considerations. Psychopharmacology Bulletin, 19: 65–68.
Ge, X., Conger, R.D., & Elder, G.H. (1996). Coming of age too early: Pubertal influences on girls’ vulnerability to psychological distress. Child Development, 67(6): 3386–3400.
Cyranowski, J.M., Frank, E., Young, E., & Shear, M.K. (2000). Adolescent onset of the gender difference in lifetime rates of major depression: A theoretical model. Archives of General Psychiatry, 57(1): 21-7.
Dahl, R.E. (2001). Affect regulation, brain development, and behavioral/emotional health in adolescence. CNS Spectrums, 6(1): 1–12.
Davies, P.T., & Cummings, E.M. (1994). Marital conflict and child adjustment: An emotional security hypothesis. Psychological Bulletin, 116(3): 387–411.
DeBellis, M.D. (1997). Posttraumatic stress disorder and acute stress disorder. In: Ammerman, R.T. & Hersen, M. (Eds.), et al. Handbook of Prevention and Treatment with Children and Adolescents: Intervention in the Real World Context. pp. 455–494. New York, NY: John Wiley & Sons, Inc.
DeBellis, M.D., Casey, B.J., Dahl, R.E., Birmaher, B., Williamson, D.E., Thomas, K.M., Axelson, D.A., Frustaci, K., Boring, A.M., Hall, J., & Ryan, N.D. (2000). A pilot study of amygdala volumes in pediatric generalized anxiety disorder. Biological Psychiatry, 48: 51–57.
DeVane, C.L., & Sallee, F.R. (1996). Serotonin selective reuptake inhibitors in child and adolescent psychopharmacology: A review of published experience. Journal of Clinical Psychiatry, 57(2): 55–66.
Diamond, G. NIMH Grant Number MH57977, Treatment of Depression in Parents—Impact on Children.
Downey, G., & Coyne, J.C. (1990). Children of depressed parents: An integrative review. Psychological Bulletin, 108(1): 50–76.
Drevets, W.C. (1999). Prefrontal cortical-amygdalar metabolism in major depression. Annals of the New York Academy of Sciences, 877: 614–637.
Drevets, W.C. (2000). Neuroimaging studies of mood disorders. Biological Psychiatry, 48: 813–829.
Drevets, W.C., Gadde, K., & Krishnan, R. (1999). Neuroimaging studies of depression. In: Charney, D.S., Nestler, E.J., Bunney, B.J. (Eds). Neurobiology of Mental Illness. New York: Oxford University Press, 394–418.
Duman, R.S., Heninger, G.R., & Nestler, E.J. (1997). A molecular and cellular theory of depression. Archives of General Psychiatry, 54(7):597–606.
Durlak, J.A., Fuhrman, T., & Lampman, C. (1991). Effectiveness of cognitive behavioral therapy for maladapting children: A meta-analysis. Psychological Bulletin, 110: 204–214.
Edelson, G., Ialongo, N., Werthamer-Lars, L., Crockett, L., & Kellam, S. (1992). Self-reported depressive symptoms in first-grade children: Developmentally transient phenomena. Journal of the American Academy of Child & Adolescent Psychiatry, 31(2): 282–90.
Ellis, B.J., & Garber, J. (2000). Psychosocial antecedents of variation in girls’ pubertal timing: maternal depression, stepfather presence, and marital and family stress. Child Development, 71(2): 485–501.
Emery, R.E. (1999). Postdivorce family life for children: An overview of research and some implications for policy. In: Thompson, R.A., Amato, P.R., et al, (Eds.). The Postdivorce Family: Children, Parenting, and Society, pp. 3–27. Thousand Oaks, CA: Sage Publications, Inc. xxiii.
Emslie, G.J., Rush, A.J., Weinberg, W.A., Kowatch, R.A., Hughes, C.W., Carmody, T., & Rintelmann, J. (1997). A double-blind, randomized, placebo-controlled trial of fluoxetine in children and adolescents with depression. Archives of General Psychiatry, 54(11): 1031–7.
Feehan, M., McGee, R., Williams, S.M., & Nada-Raja, S. (1995). Models of adolescent psychopathology: Childhood risk and the transition to adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 34(5): 670–9.
Field, T. NIMH Grant Number MH46586, Preventing Depression in Infants of Depressed Mothers.
Field, T.M. (1998). Early interventions for infants of depressed mothers. Pediatrics, 102(5E):1305–1310.
Field, T.M. (2000). Infants of depressed mothers. In: Johnson, S.L., Hayes, A.M., et al. (Eds.). Stress, Coping, and Depression, pp. 3–22. Mahwah, NJ: Lawrence Erlbaum Associates, Inc., Publishers.
Fleming, A.S., O’Day, D.H., & Kraemer, G.W. (1999). Neurobiology of mother-infant interactions: Experience and central nervous system plasticity across development and generations. Neuroscience & Biobehavioral Reviews, 23(5): 673–685.
Focht-Birkerts, L., & Beardslee, W.R. (2000). A child’s experience of parental depression: Encouraging relational resilience in families with affective illness. Family Process, 39(4): 417–34.
Francis, D.S., Caldji, C., Champagne, F., Plotsky, P.M., & Meaney, M.J. (1999). The role of corticotropin-releasing factor-norepinephrine systems in mediating the effects of early experience on the development of behavioral and endocrine responses to stress. Society of Biological Psychiatry, 46: 1153–1166.
Francis, D.D., & Meaney, M.J. (1999). Maternal care and the development of stress responses. Current Opinion in Neurobiology, 9(1): 128–134.
Fristad, M.A., Gavazzi, S.M., & Soldano, K.W. (1998). Multi-family psychoeducation groups for childhood mood disorders: A program description and preliminary efficacy data. Contemporary Family Therapy, 20(3): 385–402.
Garber, J. NIMH Grant Number MH57822, Treatment of Depression in Parents—Impact on Children.
Garber, J., & Hilsman, R. (1992). Cognitions, stress, and depression in children and adolescents. Child & Adolescent Psychiatric Clinics of North America, 1(1): 129–167.
Garber J., Kriss, M.R., Koch, M., & Lindholm, L. (1988). Recurrent depression in adolescents: A follow-up study. Journal of the American Academy of Child and Adolescent Psychiatry, 27(1): 49–54.
Garrison, C.Z., Waller, J.L., Cuffe, S.P., McKeown, R.E., Addy, C.L., & Jackson, K.L., (1997). Incidence of Major Depressive Disorder and Dysthymia in Young Adolescents. Journal of the American Academy of Child and Adolescent Psychiatry, 36: 458–465.
Geller, B., Cooper, T.B., McCombs, H.G., Graham, D., & Wells, J. (1989). Double-blind, placebo-controlled study of nortriptyline in depressed children using a “fixed plasma level” design. Psychopharmacology Bulletin, 25(1): 101–8.
Glaser, D. (2000). Child abuse and neglect and the brain—a review. Journal of Child Psychology & Psychiatry and Allied Disciplines, 41(1): 97–116.
Gladstone, T.R., & Kaslow, N.J. (1995). Depression and attributions in children and adolescents: A meta-analytic review. Journal of Abnormal Child Psychology, 23(5): 597–606.
Goodman, S.H., & Brumley, H.E. (1990). Schizophrenic and depressed mothers: Relational deficits in parenting. Developmental Psychology, 26(1): 31–39.
Goodman, S.H., & Gotlib, I.H. (1999). Risk for psychopathology in the children of depressed mothers: A developmental model for understanding mechanisms of transmission. Psychological Review, 106(3): 458–90.
Goodyer, I. M., Herbert, J., Tamplin, A., Secher, S.M., & Pearson, J. (1997). Short-term outcome of major depression: II. Life events, family dysfunction, and friendship difficulties as predictors of persistent disorder. Journal of the American Academy of Child and Adolescent Psychiatry, 36(4): 474–80.
Gotlib, I.H., Lewinsohn, P.M., Seeley, J.R., Rohde, P., & Redner, J.E. (1993). Negative cognitions and attributional style in depressed adolescents: An examination of stability and specificity. Journal of Abnormal Psychology, 102(4): 606–15.
Gould, M.S. (1990). Teenage suicide clusters. Journal of the American Medical Association, 263(15): 2051–2.
Gould, M.S., Fisher, P., Parides, M., Flory, M., & Shaffer, D. (1996). Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry, 53(12): 1155–62.
Gould, M.S., & Shaffer, D. (1986). The impact of suicide in television movies. Evidence of imitation. New England Journal of Medicine, 315(11): 690–4.
Greenberg, R.P., Bornstein, R.F., Zborowski, M.J., Fisher, S., & Greenberg, M.D. (1994). A meta-analysis of fluoxetine outcome in the treatment of depression. The Journal of Nervous and Mental Disease, 182(10): 547–51.
Gunnar, M.R. (1998). Quality of early care and buffering of neuroendocrine stress reactions: Potential effects on the developing human brain. Preventive Medicine, 27(2): 208–11.
Hammen, C. (1992). Life events and depression: the plot thickens. American Journal of Community Psychology, 20(2): 179–93.
Hammen, C., Burge, D, Burney, E., & Adrian, C. (1990). Longitudinal study of diagnoses in children of women with unipolar and bipolar affective disorder. Archives of General Psychiatry, 47(12): 1112–7.
Hammen, C., & Zupan, B.A. (1984). Self-schemas, depression, and the processing of personal information in children. Journal of Experimental Child Psychology, 37(3): 598–608.
Hammen, C., & Rudolph, K.D. (1996). Childhood depression. In: Marsh, E.J., & Barkley, R.A. (Eds.) Child Psychopathology, pp. 153–195. New York: Guilford Press.
Hammen, C., Rudolph, K., Weisz, J., Rao, U., & Burge, D. (1999). The context of depression in clinic-referred youth: Neglected areas in treatment. Journal of the American Academy of Child & Adolescent Psychiatry, 38(1): 64–71.
Handley, S.L., Dunn, T.L., Waldron, G., & Baker J.M. (1980). Tryptophan, cortisol and puerperal mood. British Journal of Psychiatry, 136: 498–508.
Harrington, R.C. (2001). Childhood depression and conduct disorder: Different routes to the same outcome? Archives of General Psychiatry, 58: 237–240.
Harrington, R., Fudge, H., Rutter, M., Pickles, A., & Hill, J. (1990). Adult outcomes of childhood and adolescent depression. I. Psychiatric status. Archives of General Psychiatry, 47(5): 465–73.
Harrington, R., Rutter, M., Weissman, M., Fudge, H., Groothues, C., Bredenkamp, D., Pickles, A., Rende, R., & Wickramaratne, P. (1997). Psychiatric disorders in the relatives of depressed probands. I. Comparison of prepubertal, adolescent and early adult onset cases. Journal of Affective Disorders, 42(1): 9–22.
Harter, S. (1988). Developmental and dynamic changes in the nature of the self-concept: Implications for child psychotherapy. In: Shirk, S.R., et al. (Eds.). Cognitive Development and Child Psychotherapy. Perspectives in Developmental Psychology. pp. 119–160. New York, NY,: Plenum Press.
Hetherington, E.M. (1999). Should we stay together for the sake of the children? In: Hetherington, E.M. (Ed.), et al. Coping with Divorce, Single Parenting, and Remarriage: A Risk and Resiliency Perspective. pp. 93–116. Mahwah, NJ: Lawrence Erlbaum Associates, Inc., Publishers.
Hilsman, R., & Garber, J. (1995). A test of the cognitive diathesis-stress model of depression in children: Academic stressors, attributional style, perceived competence, and control. Journal of Personal Social Psychology, 69: 370–380.
Hoar, W. (1998). Prozac Rx for children jumps 500%. Mental Health News Alert, September 29, 1998, pp. 13.
Hughes, C.W., Emslie, G.J., Crismon, M.L., Wagner, K.D., Birmaher, B., Geller, B., Pliszka, S.R., Ryan, N.D., Strober, M., Trivedi, M.H., Toprac, M.G., Sedillo, A., Llana, M.E., Lopez, M., & Rush, A.J. (1999). The Texas children’s medication algorithm project: Report of the Texas consensus conference panel on medication treatment of childhood major depressive disorder. Review. Journal of the American Academy of Child and Adolescent Psychiatry, 38(11): 1442–54.
Hughes, C.W., Preskorn, S.H., Wrona, M., Hassanein, R., & Tucker, S. (1990). Follow-up of adolescents initially treated for prepubertal-onset major depressive disorder with imipramine. Psychopharmacology Bulletin, 26(2): 24–8.
Kagan, J., & Snidman, N. (1999). Early childhood predictors of adult anxiety disorders. Biological Psychiatry, 46(11): 1536–1541.
Kahn, J.S., Kehle, T.J., Jenson, W.R., & Clark, E. (1990). Comparison of cognitive-behavioral, relaxation, and self-modeling interventions for depression among middle-school students. School Psychology Review, 19: 196–211.
Kashani, J.H., Shekim, W.O., & Reid, J.C. (1984). Amitriptyline in children with major depressive disorder: A double-blind crossover pilot study. Journal of the American Academy of Child Psychiatry, 23(3): 348–51.
Kaslow, N.J., Deering, C.G., & Ash, P. (1996). Handbook of Relational Diagnosis and Dysfunctional Family Patterns, 171–85. New York, N.Y.: John Wiley and Sons.
Kaslow, N.J., Deering, C.G., & Racusin, G.R. (1994). Depressed children and their families. Clinical Psychology Review, 14: 39–59.
Kaslow, N.J., McClure, E.B., & Connell, A.M. (in press). Treatment of Depression in Children and Adolescents. In: Gotlib, I.H., & Hammen, C.L. (Eds.) Handbook of Depression and its Treatment. New York, NY: Guilford Press.
Kazdin, A.E., French, N.H., & Unis, A.S. (1983). Child, mother, and father evaluations of depression in psychiatric inpatient children. Journal of Abnormal Child Psychology, 11: 167–179.
Keating, D.P., & Hertzman, C. (Eds.) (1999). Development Health and the Wealth of Nations: Social, Biological, and Educational Dynamics. New York, NY: Guilford Press.
Keller, M.B., McCullough, J.P., Klein, D.N., Arnow, B., Dunner, D.l., Gelenberg, A.J., Markowitz, J.C., Nemeroff, C.B., Russell, J.M., Thase, M.E., Trivedo, M.H., & Zajecka, J. (2000). A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. New England Journal of Medicine, 342(20): 1462–70.
Keller, M.B., Ryan, N.D., & Birmaher, B. (1998). Paroxetine and imipramine in the treatment of adolescent depression. In: New Research Program Abstracts, Annual Meeting of the American Psychiatric Association, No. 123.
Kelly, J.B. (2000). Children’s adjustment in conflicted marriage and divorce: A decade review of research. Journal of American Academy of Child & Adolescent Psychiatry, 39(8): 963–73.
Kendall, P.C., Kortlander, E., Chansky, T.E., & Brandy, E.U. (1992). Comorbidity of anxiety and depression in youth: Treatment implications. Journal of Consulting and Clinical Psychology, 60(6): 869–80.
Kendler, K.S. (1996). Major depression and generalized anxiety disorder. Same genes (partly) different environments—revisited. British Journal of Psychiatry, 168: 68–75.
Kessler, R.C., DuPont, R.L., Berglund, P., & Wittchen, H. (1999). Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. American Journal of Psychiatry, 156(12): 1915–1923.
Kim, K., & Smith, P.K. (1998). Childhood stress, behavioral symptoms and mother-daughter pubertal development. Journal of Adolescence, 21(3): 231–40.
Kline, M., Tschann, J.M., Johnston, J.R., & Wallerstein, J.S. (1989). Children’s adjustment in joint and sole physical custody families. Developmental Psychology, 25(3): 430–438.
Kovacs, M., Feinberg, T.L., Crouse-Novak, M.A., Paulauskas, S.L., & Finkelstein, R. (1984a). Depressive disorders in childhood. I. A longitudinal prospective study of characteristics and recovery. Archives of General Psychiatry, 41(3): 229–37.
Kovacs, M., Feinberg, T.L., Crouse-Novak, M.A., Paulauskas, S.L., Pollock, M., & Finkelstein, R. (1984b). Depressive disorders in childhood. II. A longitudinal study of the risk for a subsequent major depression. Archives of General Psychiatry, 41(7): 643–9.
LeDoux, J. (1998). Fear and the brain: where have we been, and where are we going? Biological Psychiatry, 44: 1229–1238.
Laurent, J., & Stark, K.D. (1993). Testing the cognitive content-specificity hypothesis with anxious and depressed youngsters. Journal of Abnormal Psychology, 102(2): 226–37.
Lewinsohn, P.M., & Clarke, G.N. (1999). Psychosocial treatments for adolescent depression. Clinical Psychology Review, 19: 329–342.
Lewinsohn, P.M., Clarke, G.N., Hops, H., & Andrews, J. (1990). Cognitive-behavioral treatment for depressed adolescents. Behavior Therapy, 21: 385-401.
Lewinsohn, P.M., Rohde, P., Klein, D.N., & Seeley, J.R. (1999). Natural course of adolescent major depressive disorder: I. Continuity into young adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 38(1): 56–63.
Lewinsohn, P.M., Rohde, P., Seeley, J.R., Klein, D.N., & Gotlib, I.H. (2000). Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry, 157(10): 1584–1591.
Lieberman, A.F., & Van Horn, P. (1998). Attachment, trauma, and domestic violence. Implications for child custody. Child & Adolescent Psychiatric Clinics of North America, 7(2): 423–43.
Lovejoy, M.C., Graczyk, P.A., O’Hare, E., & Neuman, G. (2000). Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review, 20(5): 561–92.
Luthar, S.S., & Cicchetti, D. (2000). The construct of resilience: Implications for interventions and social policies. Developmental Psychopathology, 12(4): 857–85.
Lyon, G.R. (1996). Learning disabilities: the future of children. Special Education for Students with Disabilities, 6(1): 54–76.
Lyons-Ruth, K., & Zeanah, C.H., Jr. (1993). The family context of infant mental health: I. Affective development in the primary caregiving relationship. In: Zeanah, C.H., Jr., et al. (Eds.). Handbook of Infant Mental Health, pp. 14–37. New York, NY: Guilford Press. xvi, 501 pp.
Lyons-Ruth, K., Connell, D,B., Grunebaum, H.U., & Botein, S. (1990). Infants at social risk: Maternal depression and family support services as mediators of infant development and security of attachment. Child Development, 61(1): 85–98.
Manson, S.M., Ackerson, L.M., Dick, R.W., & Baron, A.E. (1990). Depressive symptoms among American Indian adolescents: Psychometric characteristics of the Center for Epidemiologic Studies Depression Scale (CESD). Psychological Assessment, 2(3): 231–237.
Marsella, A.J. (1987). The measurement of depressive experience and disorder across cultures. In: Marsella, A.J. & Hirschfeld, R.M.A., et al. (Eds.). The Measurement of Depression, pp. 376–397. New York, NY: The Guilford Press. xvi, 411 pp.
Martin, G., & Waite, S. (1994). Parental bonding and vulnerability to adolescent suicide. Acta Psychiatrica Scandinavica, 89(4): 246–54.
Marton, P., & Kutcher, S. (1995). The prevalence of cognitive distortion in depressed adolescents. Journal of Psychiatry & Neuroscience, 20(1): 33–38.
Masten, A., Best, K., & Garmezy, N. (1990). Resilience and development: Contributions from the study of children who overcome adversity. Development and Psychopathology, 2: 425–444.
McFarlane, A. H., Bellissimo, A., & Norman, G.R. (1995). The role of family and peers in social self-efficacy: Links to depression in adolescence. American Journal of Orthopsychiatry, 65(3): 402–410.
Meaney, M.J., Diorio, J., Francis, D., Widdowson, J., LaPlante, P., Caldji, C., Sharma, S., Seckl, J.R., & Plotsky, P.M. (1996). Early environmental regulation of forebrain glucocorticoid receptor gene expression: Implications for adrenocortical responses to stress. Developmental Neuroscience, 18: 49–72.
Merikangas, K.R., Risch, N.J., & Weissman, M.M. (1994). Comorbidity and co-transmission of alcoholism, anxiety and depression. Psychological Medicine, 24(1): 69–80.
Mitchell, J., McCauley, E., Burke, P.M., & Moss, S.J. (1988). Phenomenology of depression in children and adolescents. Journal of the American Academy of Child & Adolescent Psychiatry, 27(1): 12–20.
Mufson, L., Weissman, M.M., Moreau, D., & Garfinkel, R. (1999). Efficacy of interpersonal psychotherapy for depressed adolescents. Archives of General Psychiatry, 56: 573–579.
Murrin, L.C., Gibbens, D.L., & Ferrer, J.R. (1985). Ontogeny of dopamine, serotonin and spirodecanone receptors in rat forebrain—an autoradiographic study. Brain Research, 355(1): 91–109.
Nolen-Hoeksema, S., Larson, J., & Grayson, C. (1999). Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology, 77(5): 1061–72.
O’Hara, M. NIMH Grant Number MH50524, Interpersonal Psychotherapy for Postpartum Depression.
Petersen, A.C., Compas, B.E., Brooks-Gunn, J., Stemmler, M., Ey, S., & Grant, K.E. (1993). Depression in adolescence. The American Psychologist, 48(2): 155–68.
Petti, T.A., & Law, W. 3rd. (1982). Imipramine treatment of depressed children: A double-blind pilot study. Journal of Clinical Psychopharmacology, 2(2): 107–10.
Phillips, D.P., & Carstensen, L.L. (1986). Clustering of teenage suicides after television news stories about suicide. New England Journal of Medicine, 315(11): 685–9.
Pine, D.S., Cohen, P., Gurley, D., Brook, J., & Ma, Y. (1998). The risk of early-adulthood anxiety and depressive disorders in adolescents with anxiety and depressive disorders. Archives of General Psychiatry, 55: 56–64.
Pine, D.S., & Grun, J. J. (1999). Childhood anxiety: Integrating developmental psychopathology and affective neuroscience. Child and Adolescent Psychopharmacology, 9: 1–12.
Poznanski, E.O. (1982). The clinical phenomenology of childhood depression. American Journal of Orthopsychiatry, 52(2): 308–13.
Preskorn, S.H., Weller, E.B., Hughes, C.W., Weller, R.A., & Bolte, K. (1987). Depression in prepubertal children: dexamethasone nonsuppression predicts differential response to imipramine vs. placebo. Psychopharmacology Bulletin, 23(1): 128–33.
Pruett, K.D., & Pruett, M.K. (1999). “Only God decides”: Young children’s perceptions of divorce and the legal system. Journal of the American Academy of Child & Adolescent Psychiatry, 38(12): 1544–50.
Puig-Antich, J., Lukens, E., Davies, M., Goetz, D., Brennan-Quattrock, J., & Todak, G. (1985). Psychosocial functioning in prepubertal major depressive disorders. II. Interpersonal relationships after sustained recovery from affective episode. Archives of General Psychiatry, 42(5): 511–7.
Puig-Antich, J., Perel, J.M., Lupatkin, W., Chambers, W.J., Tabrizi, M.A., King, J., Goetz, R., Davies, M., & Stiller, R.L. (1987). Imipramine in prepubertal major depressive disorders. Archives of General Psychiatry, 44(1): 81–89.
Radke-Yarrow, M., Cummings, E.M., Kuczynski, L., & Chapman, M. (1985). Patterns of attachment in two-and three-year-olds in normal families and families with parental depression. Child Development, 56(4): 884–893.
Rajkowska, G., Miguel-Hidalgo, J.J., Wei, J., Dilley, G., Pittman, S.D., Meltzer, H.Y., Overholser, J.C., Roth, B.L., & Stockmeier, C.A. (1999). Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biological Psychiatry, 45(9): 1085–98.
Raleigh, M.J., McGuire, M.T., Brammer, G.L., & Yuwiler, A. (1984). Social and environmental influences on blood serotonin concentrations in monkeys. Arch Gen Psychiatry, Apr; 41(4): 405–10.
Rao, U., Ryan, N.D., Birmaher, B., Dahl, R.E., Williamson, D.E., Kaufman, J., Rao, R., & Nelson, B. (1995). Unipolar depression in adolescents: clinical outcome in adulthood. Journal of the American Academy of Child & Adolescent Psychiatry, 34(5): 566–78.
Rao, U., Dahl, R.E., Ryan, N.D., Birmaher, B, Williamson, D.E., Giles, D.E., Rao, R., Kaufman, J., & Nelson, B. (1996). The relationship between longitudinal clinical course and sleep and cortisol changes in adolescent depression. Biological Psychiatry, 40(6): 474–84.
Rehm, L.P., & Sharp, R.N. (1996). Strategies for childhood depression. In: Reinecke, M.A., & Dattilio, F.M., et al. (Eds.). Cognitive Therapy with Children and Adolescents: A Casebook for Clinical Practice, pp. 103–123. New York, NY: Guilford Press. xxiv, 416 pp.
Reinecke, M.A. (2000). Suicide and depression. In: Dattilio, F.M., & Freeman, A. (Eds.) Cognitive-behavioral Strategies in Crisis Intervention (2nd ed.), pp. 84–125. New York, NY: The Guilford Press. xxii, 470 pp.
Reinherz, H.Z., Giaconia, R.M., Hauf, A.M., Wasserman, M.S., & Paradis, A.D. (2000). General and specific childhood risk factors for depression and drug disorders by early adulthood. Journal of the American Academy of Child and Adolescent Psychiatry, 39: 223–231.
Reinherz, H.Z., Giaconia, R.M., Pakiz, B., Silverman, A.B., Frost, A.K., & Lefkowitz, E.S. (1993). Psychosocial risks for major depression in late adolescence: A longitudinal community study. Journal of the American Academy of Child and Adolescent Psychiatry, 32: 1155–1163.
Reynolds, W.M., & Coats, K.I. (1986). A comparison of cognitive-behavioral therapy and relaxation training for the treatment of depression in adolescents. Journal of Consulting and Clinical Psychology, 54(5): 653–60.
Riley, A. NIMH Grant Number MH58384, Effects on Children of Treating Maternal Depression.
Rogeness, G.A., & McClure, E.B. (1996). Development and neurotransmitter-environmental interactions. Development & Psychopathology, 8(1): 183–199.
Rossello, J., & Bernal, G. (1999). The efficacy of cognitive behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology, 67(5):734–745.
Rotheram-Borus, M.J., Piacentini, J., Miller, S., Graae, F., Dunne, E., Cantwell, C. (1996). Toward improving treatment adherence among adolescent suicide attempters. Clinical Child Psychology & Psychiatry, 1(1): 99–108.
Rotheram-Borus, M.J., & Trautman, P.D. (1988). Hopelessness, depression, and suicidal intent among adolescent suicide attempters. Journal of the American Academy of Child & Adolescent Psychiatry, 27(6): 70–4.
Rudolph, K.D., Hammen, C., & Burge, D. (1994). Interpersonal functioning and depressive symptoms in childhood: Addressing the issues of specificity and comorbidity. Journal of Abnormal Child Psychology, 22(3): 355–71.
Rueter, M.A., Scaramella, L., Wallace, L.E., & Conger, R.D. (1999). First onset of depressive or anxiety disorders predicted by the longitudinal course of internalizing symptoms and parent-adolescent disagreements. Archives of General Psychiatry, 56: 726–32.
Rutter, M. (1979). Protective factors in children’s responses to stress and disadvantage. In: Kent, M.W., & Rolf, E. (Eds.) Primary Prevention in Psychopathology: Social Competence in Children, Volume 8, pp. 49–74. Hanover, NH: University Press of New England.
Rutter, M. (1990). Psychosocial resilience and protective mechanisms. In: Rolf, J.E., & Masten, A.S., et al., (Eds.) Risk and Protective Factors in the Development of Psychopathology, pp. 181–214. New York, NY: Cambridge University Press. xv, 554 pp.
Rutter, M. (1995). Maternal deprivation. In: Bornstein, M.H. (Ed.). Handbook of Parenting, Vol. 4: Applied and Practical Parenting. Mahwah, NJ: Lawrence Erlbaum Associates, Inc. xxvi, 596.
Ryan, N.D., Puig-Antich, J., Ambrosini, P., Rabinovich, H., Robinson, D., Nelson, B., Iyengar, S., & Twomey, J. (1987). The clinical picture of major depression in children and adolescents. Archives of General Psychiatry, 44(10): 854–61.
Sadowski, C., & Kelley, M.L. (1993). Social problem solving in suicidal adolescents. Journal of Consulting and Clinical Psychology, 61(1): 121–7.
Sameroff, A.J., Seifer, R., Barocas, R., Zax, M., & Greenspan, S. (1987). Intelligence quotient scores of 4-year-old children: Social-environmental risk factors. Pediatrics, 79(3): 343–50.
Sanford, M., Szatmari, P., Spinner, M., Munroe-Blum, H., Jamieson, E., Walsh, C., & Jones, D. (1995). Predicting the one-year course of adolescent major depression. Journal of the American Academy of Child and Adolescent Psychiatry, 34(12): 1618–28.
Sapolsky, R.M. (1996). Stress, glucocorticoids, and damage to the nervous system: The current state of confusion. Stress, 1(1): 1–19.
Sapolsky, R.M., Uno, H., Rebert, C.S., & Finch, C.E. (1990). Hippocampal damage associated with prolonged glucocorticoid exposure in primates. Journal of Neuroscience, 10(9): 2897–902.
Schraedley, P.K., Gotlib, I.H., & Hayward, C. (1999). Gender differences in correlates of depressive symptoms in adolescents. Journal of Adolescent Health, 25(2): 98–108.
Schwartz, C.E., Dorer, D.J., Beardslee, W.R., Lavori, P.W., & Keller, M.B. (1990). Maternal expressed emotion and parental affective disorder: Risk for childhood depressive disorder, substance abuse, or conduct disorder. Journal of Psychiatric Research, 23(3): 231–50.
Schwartz, C.E., Snidman, N., & Kagan, J. (1999). Adolescent social anxiety as an outcome of inhibited temperament in childhood. Journal of American Academy of Child & Adolescent Psychiatry, 38(8): 1008–15.
Sexson, S. B., Glanville, D. N., & Kaslow, N. J. (in press). Attachment and depression: Implications for family therapy. Child and Adolescent Psychiatric Clinics of North America.
Shain, B.N., Naylor, M., & Alessi, N. (1990). Comparison of self-rated and clinician-rated measures of depression in adolescents. American Journal of Psychiatry, 147: 793–795.
Siegel, J.M., Yancey, A.K., Aneshensel, C.S., & Schuler, R. (1999). Body image, perceived pubertal timing, and adolescent mental health. Journal of Adolescent Health, (2): 155–65.
Silberg, J., Pickles, A., Rutter, M., Hewitt, J., Simonoff, E., Maes, H., Carbonneau, R., Murrelle, L., Foley, D., & Eaves, L. (1999). The influence of genetic factors and life stress on depression among adolescent girls. Archives of General Psychiatry, 56(3): 225–32.
Simeon, J.G., Dinicola, V.F., Ferguson, H.B., & Copping, W. (1990). Adolescent depression: A placebo-controlled fluoxetine treatment study and follow-up. Progress in Neuropsychopharmacology & Biological Psychiatry, 14(5): 791–5.
Smyth, J., Stone, A., Hurewitz, A., & Kaell, A. (1999). Effects of writing about stressful experiences on symptom reduction in patients with asthma or rheumatoid arthritis. Journal of the American Medical Association, 281: 1304–1309.
Stark, K.D., Rouse, L.W., & Livingston, R. (1991). Treatment of depression during childhood and adolescence: Cognitive-behavioral procedures for the individual and family. In: Kendall, P.C., et al. (Eds.). Child and Adolescent Therapy: Cognitive-behavioral Procedures, pp. 165–206. New York, NY: Guilford Press. xviii, 361 pp.
Stowe, Z.N., Calhoun, K., Ramsey, C., Sadek, N., & Newport, J. (2001). Mood disorders during pregnancy and lactation: Defining issues of exposure and treatment, CNS Spectrums, 6: 150–166.
Strunk R. (1987). Deaths from asthma in childhood: Patterns before and after professional intervention. Pediatric Asthma, Allergy, Immunology, 1: 5–13.
Stubbe, D.E., Zahner, G.E., Goldstein, M.J., & Leckman, J.F. (1993). Diagnostic specificity of a brief measure of expressed emotion: A community study of children. Journal of Child Psychology and Psychiatry and Allied Disciplines, 34(2): 139-54.
Summerville, M.B., Abbate, M.F., Siegel, A.M., Serravezza, J., & Kaslow, N.J. (1992). Psychopathology in urban female minority adolescents with suicide attempts. Journal of the American Academy of Child & Adolescent Psychiatry, 31(4): 663–8.
Szigethy, E., & Wisner, K. (2000). Psychopharmacological treatment of mood and anxiety disorders during pregnancy. In: Steiner, M., Yonkers, K.A., & Eriksson, E. (Eds.) Mood Disorders in Women, pp. 295–312. London, England: Martin Dunitz.
U.S. Public Health Service. (2000). Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, D.C.
Wagner, K.D., Rouleau, M., & Joiner, T. (2000). Cognitive factors related to suicidal ideation and resolution in psychiatrically hospitalized children and adolescents. American Journal of Psychiatry, 157(12): 2017–2021.
Warren, M.P., & Brooks-Gunn., J. (1989). Mood and behavior at adolescence: Evidence for hormonal factors. Journal of Clinical Endocrinology and Metabolism, 69(1): 77–83.
Weinshilboum, R.M. (1983). Biochemical genetics of catecholamines in humans. Mayo Clinic Procedures, 58(5): 319–30.
Weiss, B., Weisz, J.R., Politano, M., Carey, M., Nelson, W.M., & Finch, A.J. (1992). Relations among self-reported depressive symptoms in clinic-referred children versus adolescents. Journal of Abnormal Psychology, 101(3): 391–7.
Weissenberger, J., & Rush, J. (1983). Biology and cognitions in depression: Does the mind know what the brain is doing? In: Salkovskis, P. (Ed.) Frontiers of Cognitive Therapy, 114–134. New York, NY: Guilford Press.
Weissman, M.M., Wolk, S., Goldstein, R.B., Moreau, D., Adams, P., Greenwald, S., Klier, C.M., Ryan, N.D., Dahl, R.E., & Wickramaratne, P. (1999a). Depressed adolescents grown up. Journal of the American Medical Association , 281: 1707–1713.
Weissman, N.M., Warner, V., Wickramaratne, P., Moreau, D., & Olfson, M. (1997). Offspring of depressed parents: 10 years later. Archives of General Psychiatry, 54: 932–940.
Weissman, M.M., Wolk, S., Wickramaratne, P., Goldstein, R.B., Adams, P., Greenwald, S., Ryan, N.D., Dahl, R.E., & Steinberg, D. (1999b). Children with prepubertal-onset major depressive disorder and anxiety grown up. Archives of General Psychiatry, 56: 794–801.
Weisz, J.R. (1997). Community Clinic Test of Youth Anxiety and Depression Treatments. Bethesda, MD: National Institutes of Health, National Institute of Mental Health.
Weisz, J.R., Rudolph, K.D., Ranger, D.A., & Sweeney, L. (1992). Cognition, competence, and coping in childhood and adolescent depression: Research findings, developmental concerns, and therapeutic implications. Development and Psychopathology, 4: 627–653.
Weller, R.A., Weller, E.B., Fristad, M.A., & Bowes, J.M. (1991). Depression in recently bereaved prepubertal children. American Journal of Psychiatry, 148: 1536–1540.
Wells, K.C, Epstein, J.N., Hinshaw, S.P., Conners, C.K., Klaric, J., Abikoff, H.B., Abramowitz, A., Arnold, L.E., Elliott, G., Pelham, W., Pfiffner, L., Severe, J., Swanson, J.M., Vitiello, B., & Wigal, T. (2000). Parenting and family stress treatment outcomes in attention deficit hyperactivity disorder (ADHD): An empirical analysis in the MTA study. Journal of Abnormal Child Psychology, 28(6): 543–553.
Wells, unpublished data. (2000). Data presented at the Surgeon Generals Conference on Children’s Mental Health (see U.S. Public Health Service, 2000 reference).
Williamson, D.E., Birmaher, B., Anderson, B.P., al-Shabbout, M., & Ryan, N.D., (1995). Stressful life events in depressed adolescents: The role of dependent events during the depressive episode. Journal of the American Academy of Child and Adolescent Psychiatry, 34: 591–598.
Wolraich, M.L., Felice, M.E., & Drotar, D. (Eds.) (1996). The Classification of Child and Adolescent Mental Diagnoses in Primary Care, Child and Adolescent Version. Elk Grove Village, IL: American Academy of Pediatrics.
Zayas, L. NIMH Grant Number MH57936-02, Reducing Perinatal Depression and Enhancing Parenting.
Appendix C
Respondents, Training Recommendations From Major Professional Associations
Cynthia Belar, Ph.D.
American Psychological Association
Pamela High, M.D.
Chair, Education Committee
Society for Developmental and Behavioral Pediatrics
Peter Jensen, M.D.
American Academy of Child and Adolescent Psychiatry
Center for the Advancement of Child and Adolescent Mental Health
Columbia University
Ellen C. Perrin, M.D.
Chair, American Board of Pediatrics Society for Developmental and Behavioral Pediatrics
Enola K. Proctor, Ph.D.
National Association of Social Workers
Director, Center for Mental Health Services Research
Washington University
Appendix D
National Advisory Mental Health Council
Chairperson
Steven E. Hyman, M.D.
Director
National Institute of Mental Health
Bethesda, Maryland
Executive Secretary
Jane A. Steinberg, Ph.D.
Director, Division of Extramural Activities
National Institute of Mental Health
Bethesda, Maryland
Members
Robert Boorstin
Vice President
Greenberg Quinlan Research, Inc.
Washington, DC
Mary L. Durham, Ph.D.
Kaiser Foundation Hospitals
Mary Jane England, M.D.
President
Washington Business Group on Health
Washington, DC
Javier I. Escobar, M.D.
Professor and Chairman,
University of Medicine and Dentistry of New Jersey,
Robert Wood Johnson Medical School
Piscataway, New Jersey
Susan Folkman, Ph.D.
Professor and Co-Director
Department of Medicine
Center for AIDS Prevention Studies (CAPS)
UCSF Prevention Sciences Group
San Francisco, California
Ellen Frank, Ph.D.
Professor of Psychiatry and Psychology
Department of Psychiatry
School of Medicine
University of Pittsburgh
Pittsburgh, Pennsylvania
Henry Lester, Ph.D.
California Institute of Technology
Division of Biology 16-29
Pasadena, California
Jeffrey A. Lieberman, M.D.
Professor and Vice Chairman
Department of Psychiatry
School of Medicine
University of North Carolina, Chapel Hill
Chapel Hill, North Carolina
James L. McClelland, Ph.D.
Co-Director
Center for the Neural Basis of Cognition
Carnegie Mellon University
Pittsburgh, Pennsylvania
James P. McNulty
President
Manic Depressive and Depressive Association of Rhode Island
Providence, Rhode Island
Charles B. Nemeroff, M.D., Ph.D.
Reunette W. Harris Professor and Chair
Department of Psychiatry and Behavioral Sciences
Emory University School of Medicine
Atlanta, Georgia
Anne C. Petersen, Ph.D.
Senior Vice President for Programs
W. K. Kellogg Foundation Battle Creek, Michigan
Elaine Sanders-Bush, Ph.D.
Professor, Department of Pharmacology
Vanderbilt University School of Medicine
Nashville, Tennessee
Edward Scolnick, M.D.
President
Merck Research Laboratories
West Point, Pennsylvania
Larry R. Squire, Ph.D.
Professor and Research Career Specialist
Department of Psychiatry
University of California School of Medicine
Veterans Affairs Medical Center
San Diego, California
James G. Townsel, Ph.D.
Professor and Director
Center for Molecular and Behavioral
Neuroscience
School of Medicine
Meharry Medical College
Nashville, Tennessee
Ming T. Tsuang, M.D., Ph.D.
Professor and Director
Department of Psychiatry
Harvard Medical School
Massachusetts Mental Health Center
Boston, Massachusetts
Roy C. Wilson, M.D.
Director
Missouri Department of Mental Health
Jefferson City, Missouri
Ex Officio Members
U.S. Department of Health and Human Services (DHHS)
Tommy G. Thompson, J.D.
Secretary, Department of Health and Human Services
Washington, DC
National Institutes of Health
Ruth Kirschstein, M.D.
Acting Director
National Institutes of Health
Bethesda, Maryland
Department of Defense
Elspeth Cameron Ritchie, M.D., LTC, MC, USA
Program Director
Mental Health Policy and Women’s Issues, OSD/HA
Falls Church, Virginia
Department of Veterans Affairs
Robert Freedman, M.D.
Medical Director
Center for Basic and Clinical Studies in Schizophrenia
Colorado Veterans Administration Hospital
Professor of Psychiatry/Pharmacology
University of California Health Sciences Center
Denver, Colorado
Liaison Representative
Center for Mental Health Services
Michael J. English, J.D., Director
Division of Knowledge Development and Systems Change
Center for Mental Health Services
Substance Abuse and Mental Health Services Administration
Rockville, Maryland
VII. References
Achenbach, T.M., & Howell, C.T. (1993). Are American children’s problems getting worse? A 13-year comparison. Journal of the American Academy of Child and Adolescent Psychiatry, 32(6): 1145–1154.
American Academy of Child and Adolescent Psychiatry. (1998). Practice parameter. Journal of the American Child and Adolescent Psychiatry , 37 (10). Special Issue.
American Academy of Pediatrics, Task Force on Minority Children’s Access to Pediatric Care. (1994). Report of the AAP Task Force on Minority Children’s Access to Pediatric Care. Elk Grove Village, Ill: American Academy of Pediatrics.
American Psychiatric Association (1980). Diagnostic and Statistical Manual of Mental Disorders, Third Edition. Washington, DC: American Psychiatric Association.
Armbruster, P., & Fallon, T. (1994). Clinical, sociodemographic, and systems risk factors for attrition in a children’s mental health clinic. American Journal of Orthopsychiatry, 64(4): 577–85.
Baro, L.A., Grilli, R., Grimshaw, J.M., Harvey, E., Oxman, A.D., & Thomson, M.A. (1998). Closing the gap between research and practice: An overview of systematic reviews of interventions to promote the implementation of research findings. The Cochrane Effective Practice and Organization of Care Review Group. British Medical Journal, 317(7156): 465–8.
Baxter, L.R., Schwartz, J.M., Bergman, K.S., Szuba, M.P., Guze, B.H., Mazziotta, J.C., Alazraki, A., Selin, C.E., Ferng, H.K., & Munford, P. (1992). Caudate glucose metabolic rate changes with both drug and behavior therapy for obsessive-compulsive disorder. Archives of General Psychiatry, 49(9): 681–689.
Bickman, L. (1996a). The evaluation of a children’s mental health managed care demonstration. Journal of Mental Health Administration, 23(1): 7–15.
Bickman, L. (1996b). Implications of a children’s mental health managed care demonstration evaluation. Journal of Mental Health Administration, 23(1): 107–17.
Bickman, L. (2000). The Fort Bragg continuum of care for children and adolescents: Mental health outcomes over 5 years. Journal of Consulting and Clinical Psychology, 68(4): 710–6.
Bickman, L., Noser, K., & Summerfelt, W.T. (1999). Long-term effects of a system of care on children and adolescents. Journal of Behavioral Health Services and Research, 26(2): 185–202.
Brestan, E.V., & Eyberg, S.M. (1998). Effective psychosocial treatments of conduct-disordered children and adolescents: 29 years, 82 studies, and 5,272 kids. Journal of Clinical Child Psychology, 27(2): 180–189.
Bronfenbrenner, U. (1979). The Ecology of Human Development. Cambridge, MA: Harvard University Press.
Brown, C.H., & Liao, J. (1999). Principles for designing randomized preventive trials in mental health: an emerging developmental epidemiology paradigm. American Journal of Community Psychology, 27(5): 673–710.
Brunk, M., Henggeler, S.W., & Whelan, J.P. (1987). Comparison of multisystemic therapy and parent training in the brief treatment of child abuse and neglect. Journal of Consulting and Clinical Psychology, 55: 171–178.
Burns, B.J. (1999). A call for a mental health services research agenda for youth with serious emotional disturbance. Mental Health Services Research, 1: 5–20.
Burns, B.J. (1991). Mental health service use by adolescents in the 1970s and 1980s. Journal of the American Academy of Child and Adolescent Psychiatry, 30: 144–150.
Burns, B.J., Costello, J.E., Angold, A., Tweed, D., Stangl, D., Farmer, E.M.Z., & Erkanli, A. (1995). Children’s mental health service use across service sectors. Health Affairs, 14(3): 148–159.
Burns, B.J., & Hoagwood, K. (in press). Evidence-Based Community Interventions for Youth with Severe Emotional and Behavioral Disorders. New York: Oxford Press.
Burns, B.J., Hoagwood, K., & Mrazek, P.J. (1999). Effective treatment for mental disorders in children and adolescents. Clinical Child and Family Psychology Review, 2(4): 199–254.
Canino, G., Costello, E.J., & Angold, A. (1999). Assessing functional impairment and social adaptation for child mental health services research. Mental Health Services Research, 1: 93–108.
Carskadon, M.A. (1999). Adolescent Sleep Patterns: Biological, Social and Psychological Influences. New York: Cambridge University Press.
Carskadon, M.A., Vieira, C., & Acebo, C. (1993). Association between puberty and delayed phase preference. Sleep, 16(3): 258–262.
Casey R.J., & Berman, J.S. (1985). The outcome of psychotherapy with children. Psychological Bulletin, 98: 388–400.
Catron, T., Weiss, B., & Bahr, M.W. (1994). The Vanderbilt School-based Counseling Program: An interagency, primary-care model of mental health services. Journal of Emotional & Behavioral Disorders, 2(4): 247–253.
Chamberlain, P., & Reid, J.B. (1991). Using a specialized foster care treatment model for children and adolescents leaving the state mental hospital. Journal of Community Psychology, 19: 266–276.
Chambless, D.L., Baker, M.J., Baucom, D.H., Beutler, L.E., Calhoun, K.S., Crits-Christoph, P., Daiuto, A., DeRubeis, R., Detweiler, J., Haaga, D.A.F., Johnson, S.B., McCurry, S., Mueser, K.T., Pope, K.S., Sanderson, W.C., Shoham, V., Stickle, T., Williams, D.A., & Woody, S.R. (1998). Update on empirically validated therapies, II. Clinical Psychology, 27: 138–145.
Child Mental Health Foundations and Agencies Network (FAN). (2000). A Good Beginning: Sending America’s Children to School With the Social and Emotional Competence They Need to Succeed. Chapel Hill, N.C.: University of North Carolina, Frank Porter Graham Child Development Center.
Clarke, G.N., Hawkins, W., Murphy, M., Sheeber, L.B., Lewinsohn, P.M., & Seeley, J.R. (1995). Targeted prevention of unipolar depressive disorder in an at-risk sample of high school adolescents: A randomized trial of a group cognitive intervention. Journal of the American Academy of Child and Adolescent Psychiatry, 34: 312–321.
Clarke, G.N., Rohde, P., Lewinsohn, P.M., Hops, H., & Seeley, J.R. (1999). Cognitive-behavioral treatment of adolescent depression: Efficacy of acute group treatment and booster sessions. Journal of the American Academy of Child and Adolescent Psychiatry, 38(3): 272–9.
Cole, David A., & McPherson, Antoinette E. (1993). Relation of family subsystems to adolescent depression: Implementing a new family assessment strategy. Journal of Family Psychology, 7(1): 119–133.
Conduct Problems Research Group (1999). Initial impact of the Fast Track prevention trial for conduct problems. I. The high-risk sample. Journal of Consulting and Clinical Psychology, 67(5): 1–15.
Crandall, D.P. (1989). Implementation aspects of dissemination: Reflections toward an immodest proposal. Knowledge and Policy: The International Journal of Knowledge Transfer and Utilization, 2: 79–106.
Curran, P.J., & Muthen, B.O. (1999). The application of latent curve analysis to testing developmental theories in intervention research. American Journal of Community Psychology, 27(4): 567–95.
Dahl, R.E. (1999). The consequences of insufficient sleep for adolescents: Links between sleep and emotional regulation. Phi Delta Kappan, 80: 354–359.
Dishion, T.J., McCord, J., & Poulin, F. (1999). When interventions harm: Peer groups and problem behavior. American Psychologist, 54(9): 755–64.
Durlak, J.A., Wells, A.M., Cotton, J.K., & Johnson, S. (1995). Analysis of selected methodological issues in child psychotherapy research. Journal of Clinical Child Psychology, 24: 141–148.
Emslie, G.J., Rush, A.J., Weinberg, W.A., Kowatch, R.A., Carmody, T., & Mayes, T.L. (1998). Fluoxetine in child and adolescent depression: Acute and maintenance treatment. Depression and Anxiety, 7(1): 32–9.
English, M. (In press). Policy Implications Relevant to Implementing Evidence-Based Treatment. In: Burns, B.J., & Hoagwood, K. (Eds.) Evidence-Based Community Interventions for Youth with Severe Emotional and Behavioral Disorders. New York: Oxford Press.
Field, T.M. (1998). Early interventions for infants of depressed mothers. Pediatrics, 102(5E): 1305–1310.
Findling, R.L., McNamara, N.K., & Gracious, B.L. (2000). Paediatric uses of atypical antipsychotics. Expert Opinions in Pharmacotherapy, 1(5): 935–45.
Fogel, A. NIMH Grant Number R01MH57669, Development of Emotion and Attention.
Forness, S.R., & Hoagwood, K. (1993). Where angels fear to tread: issues in sampling, design, and implementation of school-based mental health services research. School Psychology Quarterly, 8(4): 291–300.
Freemantle, N., Harvey, E.L., Wolf, F., Grimshaw, J.M., Grilli, R., & Bero, L.A. (2000). Printed educational materials: Effects on professional practice and health care outcomes. Cochrane Database of Systematic Reviews, (2): CD000172.
Friedman, R.M. (1992). Mental health and substance abuse services for adolescents: Clinical and service system issues. Administration & Policy in Mental Health, 19(3): 159–178.
Friedman, R.M. (2001). The practice of psychology with children, adolescents, and their families: A look to the future. In Hughes, J., Conoley, J. & La Greca, A. (Eds.). Handbook of Psychological Services for Children and Adolescents. New York, NY: Oxford Press.
Fuchs, D., Fuchs, L.S., & Bahr, M.W. (1990). Mainstream assistance teams: A scientific basis for the art of consultation. Exceptional Child, 57(2): 128–39.
Glisson, C., & Hemmelgarn, A. (1998). The effects of organizational climate and interorganizational coordination on the quality and outcomes of children’s service systems. Child Abuse and Neglect, 22(5): 401–21.
Gordon, R.S. (1983). An operational classification of disease prevention. Public Health Reports, 98(2): 107–9.
Gordon, R.S. (1987). An operational definition of disease prevention. In: Steinberg, J.A., & Silverman, M.M. (Eds.) Preventing Mental Disorders, pp. 20–36. Rockville, MD: U.S. Department of Health and Human Services.
Greenbaum, P.E., Dedrick, R.F., Friedman, R.M., Kutash, K., Brown, E.C., Lardieri, S.P., & Pugh, A.M. (1998). National Adolescent and Child Treatment Study (NACTS): Outcomes for children with serious emotional and behavioral disturbance. In: Epstein, M.H., Kutash, K., et al. (Eds.) Outcomes for Children and Youth With Emotional and Behavioral Disorders and Their Families: Programs and Evaluation Best Practices, pp. 21–54. Austin, TX: Pro-Ed, Inc. xviii, 738 pp.
Hammen, C., Henry, R., & Daley, S.E. (2000). Depression and sensitization to stressors among young women as a function of childhood adversity. Journal of Consulting and Clinical Psychology, 68(5): 782–787.
Hann, D.M., & Borek, N.T. (Eds.). (In press). Taking Stock of Risk Factors for Child/Youth Externalizing Behavior Problems. Washington, DC:
U.S. Government Printing Office.
Harachi, T., Ayers, C.D., Hawkins, J.D., & Catalano, R. (1996). Empowering communities to prevent adolescent substance abuse: Process evaluation results from a risk- and protection-focused community mobilization effort. Journal of Primary Prevention, 16: 233–254.
Henggeler, S.W., Cunningham, P.B., Pickrel, S.G., Schoenwald, S.K., & Brondino, M.J. (1996). Multisystemic therapy: An effective violence prevention approach for serious juvenile offenders. Journal of Adolescence, (1): 47–61.
Henggeler, S.W., Rowland, M.D., Pickrel, S.G., Miller, S.L., Cunningham, P.B., Santos, A.B., Schoenwald, S.K., Randall, J., & Edwards, J.E. (1997). Investigating family-based alternatives to institution-based mental health services for youth: Lessons learned from the pilot study of a randomized field trial. Journal of Clinical Child Psychology, 26(3): 226–33.
Henggeler, S.W., Rowland, M.D., Randall, J., Ward, D.M., Pickrel, S.G., Cunningham, P.B., Miller, S.L., Edwards, J., Zealberg, J.J., Hand, L.D., & Santos, A.B. (1999). Home-based multisystemic therapy as an alternative to the hospitalization of youths in psychiatric crisis: Clinical outcomes. Journal of the American Academy of Child & Adolescent Psychiatry, 38 (11): 1331–1339.
Henggeler, S.W., Schoenwald, S.K., Borduin, C.M., Rowland, M.D., & Cunningham, P.B. (1998). Multisystemic Treatment of Antisocial Behavior in Children and Adolescents. New York: Guilford Press.
Hetherington, E.M., & Stanley-Hagan, M. (1999). The adjustment of children with divorced parents: A risk and resiliency perspective. Journal of Child Psychology & Psychiatry and Allied Disciplines, 40(1): 129–40.
Hinshaw, S.P., Owens, E.B., Wells, K.C., Kraemer, H.C., Abikoff, H.B, Arnold, E.L., Conners, C.K., Elliott, G., Greenhill, L.L., Hechtman, L., Hoza, B., Jensen, P.S., March, J.S., Newcorn, J.H., Pelham, W.E, Swanson, J.M., Vitiello, B., & Wigal, T. (2000). Family processes and treatment outcome in the MTA: negative/ineffective parenting practices in relation to multimodal treatment. Journal of Abnormal Child Psychology, 28(6): 555–568.
Hoagwood, K. (2000). Commentary: The dose effect in children’s mental health services. Journal of the American Academy of Child & Adolescent Psychiatry, 39(2): 172–175.
Hoagwood, K., Hibbs, E., Brent, D., & Jensen, P. (1995). Efficacy and effectiveness in studies of child and adolescent psychotherapy. Journal of Consulting and Clinical Psychology, 63(5): 683–687.
Hoagwood, K. (1997). Interpreting nullity. The Fort Bragg experiment—a comparative success or failure? The American Psychologist, 52(5): 546–50.
Hoagwood, K., Jensen, P., Petti, T., & Burns, B. (1996). Outcomes of care for children and adolescents: A conceptual model. Journal of the American Academy of Child and Adolescent Psychiatry, 35(8): 1055–1063.
Hohmann, A.A. (1999). A contextual model for clinical mental health effectiveness research. Mental Health Services Research, 1(2): 83–91.
Ialongo, N.S., Werthamer, L., Kellam, S.G., Brown, C.H., Wang, S., & Lin, Y. (1999). Proximal impact of two first-grade preventive interventions on the early risk behaviors for later substance abuse, depression, and antisocial behavior. American Journal of Community Psychology, 27(5): 599–641.
Institute of Medicine (IOM). (1989). Research on Children and Adolescents with Mental, Behavioral, and Developmental Disorders: Mobilizing a National Initiative. Report of a study by a committee of the Institute of Medicine. Washington, DC: National Academy Press.
Institute of Medicine (IOM). (2000). Report on Bridging Disciplines in the Brain, Behavioral, and Clinical Sciences. Pellmar, T.C., & Eisenberg, L. (Eds.). Committee on Building Bridges in the Brain, Behavioral, and Clinical Sciences, Division of Neuroscience and Behavioral Health.
Jaycox, L.H., Reivich, K.J., Gillham, J., & Seligman, M.E. (1994). Prevention of depressive symptoms in school children. Behavioral Research Therapy, 32(8): 801–16.
Jensen, P.S., Bhatara, V., Vietello, B., Hoagwood, K., Feil, M., & Burke, L. (1999). Psychoactive medication prescribing practices for U.S. children: Gaps between research and clinical practice. Journal of the American Academy of Child and Adolescent Psychiatry, 38: 557–565.
Jensen, P.S., Hoagwood, K., & Petti, T. (1996). Outcomes of mental health care for children and adolescents: II. Literature review and application of a comprehensive model. Journal of the American Academy of Child and Adolescent Psychiatry, 35: 1064–77.
Jensen, P.S., Hoagwood, K., & Trickett, E.J. (1999). Ivory towers or earthen trenches? Community collaborations to foster real-world research. Applied Developmental Science, 3: 206–212.
Journal of the American Academy of Child and Adolescent Psychiatry (1999), 38 (5). Special section on current knowledge and unmet needs in pediatric psychopharmacology, pp. 501–565.
Journal of Clinical Child Psychology (1998), 27 (2). Special issue on empirically supported psychosocial intervention.
Kanner, L. (1935). Child Psychiatry. Springfield, IL: C.C. Thomas.
Karoly, L., Greenwood, P., Everingham, S., Hoube, J., Kilburn, M.R., Rydell, C.P., Sanders, M., & Chiesa, J. (1998). Investing In Our Children. Santa Monica, C.A.: RAND.
Kazdin, A.E., & Mazurick, J.L. (1994). Dropping out of child psychotherapy: Distinguishing early and late dropouts over the course of treatment. Journal of Consulting & Clinical Psychology, 62(5): 1069–74.
Kazdin, A.E. NIMH Grant Number MH59029, New Treatment Delivery Model for Antisocial Children.
Kazdin, A.E. (1999). Current (lack of) status of theory in child and adolescent psychotherapy research. Journal of Clinical Child Psychology, 28:533–543.
Kazdin, A.E. (2000a). Developing a research agenda for child and adolescent psychotherapy. Archives of General Psychiatry, 57(9): 829–35.
Kazdin, A.E. (2000b). Psychotherapy for children and adolesecents. New York, NY: Oxford University Press.
Kazdin, A.E., & Weisz, J.R. (1998). Identifying and developing empirically supported child and adolescent treatments. Journal of Consulting and Clinical Psychology, 66(1): 19–36.
Kazdin A.E., Bass, D., Ayers, W.A., & Rodgers, A. (1990). Empirical and clinical focus of child and adolescent psychotherapy research. Journal of Consulting Clinical Psychology, 58(6): 729–40.
Kazdin, A.E., Holland, L., & Crowley, M. (1997). Family experience of barriers to treatment and premature termination from child therapy. Journal of Consulting Clinical Psychology, 65(3): 453–63.
Kellam, S.G., Koretz, D., & Moscicki, E.K. (1999). Core elements of developmental epidemiologically based prevention research. American Journal of Community Psychology, 27(4): 463–82.
Kelly, J.A., St. Lawrence, J., Diaz, Y.E., & Stevenson, L.Y. (1993). HIV risk behavior reduction following intervention with key opinion leaders of population: An experimental analysis. American Journal of Public Health, 81(2): 168–171.
Kendler, K.S., Karkowski, L.M., & Prescott, C.A. (1999). Causal relationships between stressful life events and the onset of major depression. American Journal of Psychiatry, 156: 837–841.
Kendler, K.S., Kessler, R.C., Walters, E.E., MacLean, C., Neale, M.C., Heath, A.C., Phil, D., & Eaves, L.J. (1995). Stressful life events, genetic liability, and onset of an episode of major depression in women. American Journal of Psychiatry, 152: 833–842.
Kendler, K.S., Kessler, R.C., Neale, M.C., Heath, A.C., & Eaves, L.J. (1993). The prediction of major depression in women: An integrated etiologic model. American Journal of Psychiatry, 150: 1139–1148.
Kendler, K.S., Thornton, L.M., Gardner, C.O. (2000). Stressful life events and previous episodes in the etiology of major depression in women: An evaluation of the kindling hypothesis. American Journal of Psychiatry, 157: 1243–1251.
Kessler, R.C. (1997). The effects of stressful life events on depression. Ann Rev Psychology, 48: 191–214.
Kirigin, K.A., Braukmann, C.J., Atwater, J.D., & Wolf, M.M. (1982). An evaluation of Teaching-Family (Achievement Place) group homes for juvenile offenders. Journal of Applied Behavior Analysis, 15(1): 1–16.
Kirk, S.A., & Kutchins, H. (1992). The Selling of DSM: The Rhetoric of Science in Psychiatry. Hawthorne, NY: Aldine De Gruyter.
Knitzer, J. (1982). Unclaimed Children: The Failure of Public Responsibility to Children and Adolescents in Need of Mental Health Services. Washington, DC: Children’s Defense Fund.
Kumra, S., Frazier, J., Jacobsen, L., McKenna, K, Gordon, C., Lenane, M., Hamburger, S., Smith, A., Albus, K., Alghband-Rad, J., & Rapaport J. (1996). Childhood onset schizophrenia: A double blind clozapine-haloperidol comparison. Archives of
General Psychiatry, 53: 1090–1097.
Kutash, K., & Rivera, V.R. (1995). Effectiveness of children’s mental health services: A review of the literature. Education & Treatment of Children, 18(4): 443–477.
Lambert, E.W., & Guthrie, P. (1996). Clinical outcomes of a children’s mental health managed-care demonstration. The Journal of Mental Health Administration, 23 (1): 51–68.
Lambert, M.J., & Bergin, A. (1994). The effectiveness of psychotherapy. In: Garfield, S.L., & Bergin, A.E. (Eds.) Handbook of Psychotherapy and Behavior Change, 3rd Edition. pp. 157–211. New York, NY: Wiley and Sons.
Laughren, T. (2000). Presentation at the Surgeon General’s Conference on Children’s Mental Health. In the Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, DC: U.S. Public Health Service.
Lewinsohn, P.M., Rohde, P., Seeley, J.R., Klein, D.N., & Gotlib, I.H. (2000). Natural course of adolescent major depressive disorder in a community sample: Predictors of recurrence in young adults. American Journal of Psychiatry, 157(10): 1584–91.
Lewinsohn, P.M., Clarke, G.N., Seeley, J.R., Rohde, P. (1994). Major depression in community adolescents: Age at onset, episode duration, and time to recurrence. Journal of the American Academy of Child & Adolescent Psychiatry, 33(6): 809–18.
Lonigan, C.J., Elbert, J.C., & Johnson, S.B. (1998). Empirically supported psychosocial interventions for children: An overview. Journal of Clinical Child Psychology, 27(2): 138–145.
McKay, M.M., McCadam, K., & Gonzales, J.J. (1996). Addressing the barriers to mental health services for inner city children and their caretakers. Community Mental Health Journal, 32(4): 353–61.
McKay, M.M., Stoewe, J., McCadam, K., & Gonzales, J. (1998). Increasing access to child mental health services for urban children and their caregivers. Health & Social Work, (1): 9–15.
McLeod, J.D., & Shanahan, M.J. (1996). Trajectories of poverty and children’s mental health. Journal of Health and Social Behavior, 37 (3): 207–220.
Meaney, M. (1999). Nongenomic transmission across generations of maternal behavior and stress responses in the rat. Science, 286(5442): 1155–1158.
Miklowitz, D.J., & Clarkin, J.F. (1999). Balancing internal and external validity. Prevention and Treatment, 2, article 0004c.
Mrazek, P.J., & Haggerty, R.J. (Eds.) (1994). Committee on Prevention of Mental Disorders, Institute of Medicine. Reducing Risks for Mental Disorders: Frontiers for Preventive Intervention Research. Washington, DC: National Academy Press.
Murray, C.J.L., & Lopez, A.D.L. (Eds.) (1996). Summary: The Global Burden of Disease. Cambridge, MA: Harvard University Press.
The MTA Cooperative Group. (1999a). Moderators and mediators of treatment response for children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 56: 1088–1096.
The MTA Cooperative Group. (1999b). A 14-month randomized clinical trial of treatment strategies for attention-deficit/hyperactivity disorder. Archives of General Psychiatry, 56: 1073–1086.
National Advisory Mental Health Council (NAMHC). (1990). National Plan for Research on Child and Adolescent Mental Disorders. Washington, DC: National Institutes of Health, National Institute of Mental Health. DHHS Publication No. ADM90-1683.
National Advisory Mental Health Council. (1995). Basic Behavioral Science Research for Mental Health: A National Investment. Bethesda, MD: National Institutes of Health/National Institute of Mental Health. NIH Publication No. 96-3682.
National Advisory Mental Health Council’s Clinical Treatment and Services Research Workgroup. (1999). Bridging Science to Service. Rockville, MD: National Institute of Mental Health. NIH Publication No. 99-4353.
National Advisory Mental Health Council’s Behavioral Science Workgroup. (2000). Translating Behavioral Science into Action. Bethesda, MD: National Institutes of Health, National Institute of Mental Health. NIH Publication No. 00-4699.
National Advisory Mental Health Council Workgroup on Mental Disorders Prevention Research. (1998). Priorities for Prevention Research at NIMH. Bethesda, MD: National Institutes of Health/National Institute of Mental Health. NIH Publication No. 98-4321.
National Center for the Dissemination of Disability Research (NCDDR). (1996). A Review of the Literature on Dissemination and Knowledge Utilization. Austin, TX: NCDDR.
National Institute of Mental Health. (2001). Draft Strategic Plan for Reducing Health Disparities. Rockville, MD: U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health.
National Institute of Mental Health Research Roundtable on Prepubertal Bipolar Disorder (in press). Journal of the American Academy of Child and Adolescent Psychiatry.
National Institute of Mental Health Prevention Research Steering Committee. (1993). The Prevention of Mental Disorders: A National Research Agenda. Washington, DC: National Institutes of Health, National Institute of Mental Health.
National Institute of Mental Health Prevention Research Steering Committee and the Institute of Medicine Committee on the Prevention of Mental Disorders. (1996). A Plan for Prevention Research for the National Institute of Mental Health: A Report to the National Advisory Mental Health Council. Washington, DC: National Institutes of Health, National Institute of Mental Health. NIH Publication No. 96-4093.
National Research Council and Institute of Medicine (2000). Shonkoff, J., & Phillips, D., (Eds.) From Neurons to Neighborhoods: The Science of Early Childhood Development. Committee on Integrating the Science of Early Childhood Development. Board on Children, Youth, and Families, Commission on Behavioral and Social Sciences and Education. Washington, DC: National Academy Press.
Norquist, G., Lebowitz, B., & Hyman, S. (1999). Expanding the frontier of treatment research. Prevention and Treatment, 2, article 0001a.
Olds, D.L., Eckenrode, J., Henderson, C.R., Kitzman, H., Powers, J., Cole, R., Sidora, K., Morris, P., Pettitt, L.M., & Luckey, D. (1997). Long-term effects of home visitation on maternal life course and child abuse and neglect. Fifteen-year follow-up of a randomized trial. Journal of the American Medical Association, 278(8): 637–43.
Olds, D.L., Henderson, C.R., Chamberlin, R., & Tatelbaum, R. (1986). Preventing child abuse and neglect: a randomized trial of nurse home visitation. Pediatrics, 78(1): 65–78.
Olds, D., Henderson, C,R. Jr., Cole, R., Eckenrode, J., Kitzman, H., Luckey, D., Pettitt, L., Sidora, K., Morris, P., & Powers, J. (1998). Long-term effects of nurse home visitation on children’s criminal and antisocial behavior: 15-year follow-up of a randomized controlled trial. Journal of the American Medical Association, 280(14): 1238–44.
Olds, D.L., Henderson, C.R. Jr., Kitzman, H.J., Eckenrode, J.J., Cole, R.E., & Tatelbaum, R.C. (1999). Prenatal and infancy home visitation by nurses: Recent findings. Future Child, 9(1): 44–65; 190–1.
Olds, D.L., Henderson, C.R., Phelps, C., Kitzman, H., & Hanks, C. (1993). Effect of prenatal and infancy nurse home visitation on government spending. Medical Care, 31(2): 155–74.
Pearson, J.L., & Koretz, D. (in press). Opportunities in prevention research at NIMH: Integrating prevention with treatment research. Prevention and Treatment.
Pelham, W.E., Wheeler, T., & Chronis, A. (1998). Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. Journal of Clinical Child Psychology, 27(2): 190–205.
Pfeiffer, S.I., & Strzelecki, S.C. (1990). Inpatient psychiatric treatment of children and adolescents: A review of outcome studies. Journal of the American Academy of Child & Adolescent Psychiatry, 29(6): 847–53.
Phaire, T. (1544-originally published). In: Neale, A.V., & Wallis, H.R.E. (Eds.) The Boke of Children. Edinburgh, Scotland: E & S Livingstone.
Pomerantz, E.M., & Ruble, D.N. (1998). The role of maternal control in the development of sex differences in child self-evaluative factors. Child Development, 69(2): 458–78.
Postman, N. (1994). The Disappearance of Childhood. New York, NY: Vintage Books.
Reid, J.B., Eddy, J.M., Fetrow, R.A., & Stoolmiller, M. (1999). Description and immediate impacts of a preventive intervention for conduct problems. American Journal of Community Psychology, 27(4): 483–517.
Roberts, R.E., Attkisson, C.C., & Rosenblatt, A. (1998). Prevalence of psychopathology among children and adolescents. American Journal of Psychiatry, 155: 715–725.
Rogers, E.M. (1995). Diffusion of Innovations. New York: The Free Press.
Rones, M., & Hoagwood, K. (2000). School-based mental health services: a research review. Clinical Trial and Family Psychology Review, 3(4): 223–41.
Rothbart, M.K. NIMH grant number R01MH43361, University of Oregon. Early Development of Temperamental Self-Regulation.
Rovee-Collier, C. (1997). Dissociations in infant memory: Rethinking the development of implicity and explicit memory. Psychology Review, 104(3): 467–98.
Rutter, M., Shaffer, D., & Shepherd, M. (1975). A Multi-Axial Classification of Child Psychiatric Disorders. Geneva, Switzerland: World Health Organization.
Samaan, R.A. (2000). The influences of race, ethnicity, and poverty on mental health of children. Journal of Health Care for the Poor and Underserved, 11(1): 100–110.
Santisteban, D.A., Szapocznik, J., Perez-Vidal, A., Kurtines, W.M., Murray, E.J., & LaPerriere, A. (1996). Efficacy of intervention for engaging youth and families into treatment and some variables that may contribute to differential effectiveness. Journal of Family Psychology, 10(1): 35–44.
Sanua, V.D. (1990). Leo Kanner, 1894–1981: The man and the scientist. Child Psychiatry and Human Development, 21(1): 3–23.
Schoenwald, S.K. (1999). NIMH Grant Number MH59138. Transportability of New Treatments: MST as a Test Case.
Schoenwald, S.K., Henggeler, S.W., Brondino, M.J., & Rowland, M.D. (2000a). Multisystemic therapy: Monitoring treatment fidelity. Family Process, 39(1): 83–103.
Schoenwald, S.K., Ward, D.H., Henggeler, S.W., Rowland, M.D. (2000b). Multisystemic therapy versus hospitalization for crisis stabilization of youth: Placement outcomes and months post-referral. Mental Health Services, 2(1): 3–12.
Schoenwald, S.K., Brown, T.L., & Henggeler, S.W. (2000c). Inside multisystemic therapy: Therapist, supervisory, and program practices. Journal of Emotional and Behavioral Disorders, 8: 113–127.
Schoenwald, S.K., & Hoagwood, K. (2001). Effectiveness and dissemination research: Overlap, distinctions, & relevance to improving mental health services for children & adolescents. Under Review.
Schwartz, J.M., Stoessel, P.W., Baxter, L.R., Martin, K.M., & Phelps, M.E. (1996). Systematic changes in cerebral glucose metabolic rate after successful behavior modification treatment of obsessive-compulsive disorder. Archives of General Psychiatry, 53(2): 109–113.
Shaffer, D., Fisher, P., Dulcan, M.K., Davis, M., Piacentini, J., Schwab-Stone, M.E., Lahey, B.B., Bourdon, K., Jensen, P.S., Bird, H.R., Canino, G., & Regier, D.A. (1996). The NIMH Diagnostic Interview Schedule for Children Version 2.3 (DISC-2.3): Description, Acceptability, Prevalence Rates, and Performance in the MECA Study. Journal of the American Academy of Child & Adolescent Psychiatry, 35(7): 865–877.
Smith, R., Cubis, J., Brinsmead, M., Lewin, T., Singh, B., Owens, P., Chan, E.C., Hall, C., Adler, R., & Lovelock, M., et al. (1990). Mood changes, obstetric experience and alterations in plasma cortisol, beta-endorphin and corticotrophin releasing hormone during pregnancy and the puerperium. Journal of Psychosomatic Research, 34 (1): 53–69.
Smith, M.L., & Glass, G.V. (1977). Meta-analysis of psychotherapy outcomes studies. American Psychologist, 32: 752–760.
Snodgrass, J. (1984). William Healy, 1869–1963: pioneer child psychiatrist and criminologist. Journal of the History of the Behavioral Sciences, 20(4): 332–9.
Stroul, B.A., & Friedman, R.M. (1988). Caring for severely emotionally disturbed children and youth. Principles for a system of care. Child Today, 17(4): 15–7.
Sturm, R., Ringel, J., Bao, C., Stein, B., Kapur, K., Zhang, W., & Zeng, F. (in press). National Estimates of Mental Health Utilization and Expenditures for Children in 1998. Journal of Behavioral Health Services and Research.
Sullivan, P.F., Neale, M.C., & Kendler, K.S. (2000). Genetic epidemiology of major depression: Review and meta-analysis. American Journal of Psychiatry, 157(10): 1552–62.
Swenson, C. NIMH Grant 60663, Community-based Treatment for Child Physical Abuse.
Szapocznik, J., Perez-Vidal, A., Brickman, A.L., Foote, F.H., Santisteban, D., Hervis, O., & Kurtines, W.M. (1988). Engaging adolescent drug abusers and their families in treatment: A strategic structural systems approach. Journal of Consulting and Clinical Psychology, 56(4): 552–61.
Takeuchi, D.T., Uehara, E., & Maramba, G. (1999). Cultural diversity and mental health treatment. In: Horwitz, A.V., Scheid, T.L. (Eds.). A Handbook for the Study of Mental Health: Social Contexts, Theories, and Systems. New York, NY: Cambridge University Press.
The UNOCCAP Oversight Board Report to the National Advisory Mental Health Council. (1998). Charting the Mental Health Status and Service Needs of Children: Recommendations from the UNOCCAP Oversight Board. Bethesda, MD: National Institutes of Health, National Institute of Mental Health.
U.S. Public Health Service. (1999). Mental Health: A Report of the Surgeon General. Rockville, MD: U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Mental Health Services, National Institutes of Health, National Institute of Mental Health.
U.S. Public Health Service. (1999). The Surgeon General’s Call to Action to Prevent Suicide. Washington, D.C.
U.S. Public Health Service. (2000). Report of the Surgeon General’s Conference on Children’s Mental Health: A National Action Agenda. Washington, D.C.
U.S. Public Health Service (2001). Youth Violence: A Report of the Surgeon General. Washington, D.C. Van den Boom, D.C. (1994). The influence of temperament and mothering on attachment and exploration: an experimental manipulation of sensitive responsiveness among lower-class mothers with irritable infants. Child Development, 65(5): 1457–77.
Van den Boom, D.C. (1994). The influence of temperament and mothering on attachment and exploration; an experimental manipulation of sensitive responsiveness among lower-class mothers with irritable infants. Child Development, 65(5): 1457–77.
Van den Boom, D.C. (1995). Do first-year intervention effects endure? Follow-up during toddlerhood of a sample of Dutch irritable infants. Child Development, 66(6): 1798–816.
Vera, M., Alegria, M., Freeman, D.H., Jr., Robles, R., Pescosolido, B., & Pena, M. (1998) Help seeking for mental health care among poor Puerto Ricans: Problem. Medical Care, 36(7): 1047–1056.
Von Bertalanffy, L. (1968). General Systems Theory. New York: Braziller.
Wahlstrom, K.L., Carskadon, M.A., Dahl, R.E., Wrobel, G.D., & Kubow, P.K. (1999). Adolescent Sleep Needs and School Starting Times, Vol. 80. Bloomington, In: Phi Delta Kappan – A Kappan Special Section.
Weisz, J.R. (2000). Agenda for child and adolescent psychotherapy research: on the need to put science into practice. Archives of General Psychiatry, 57(9): 837–8.
Weisz, J.R. (1997). Community Clinic Test of Youth Anxiety and Depression Treatments. Bethesda, MD: National Institutes of Health, National Institute of Mental Health.
Weisz, J.R., Donenberg, G.R., Han, S.S., & Weiss, B. (1995). Bridging the gap between laboratory and clinic in child and adolescent psychotherapy. Journal of Consulting and Clinical Psychology, 63: 688–701.
Weisz, J.R. & Hawley, K.M. (1998). Finding, evaluating, refining and applying empirically supported treatments for children and adolescents. Journal of Clinical Child Psychology, 27: 206–216.
Weisz, J.R., Huey, S.J., & Weersing, V.R. (1998). Psychotherapy outcome research with children and adolescents: The state of the art. In: Ollendick, T.H., & Prinz, R.J. (Eds.) Advances in Clinical Trial Psychology. 20: 49–91.
Weisz, J.R., & Jensen, P.S. (1999). Efficacy and effectiveness of child and adolescent psychotherapy and pharmacotherapy. Mental Health Services Research, 1(3): 125–57.
Weisz, J.R., & Weiss, B. (1993). Effects of psychotherapy with children and adolescents. Newbury Park, CA: Sage.
Weisz, J.R., Weiss B., & Langmeyer, D.B. (1987). Giving up on child psychotherapy: Who drops out? Journal of Consulting and Clinical Psychology, 55: 916–918.
Weisz, J.R., Weiss B., & Langmeyer, D.B. (1989). On “dropouts” and “refusers” in child psychotherapy: Reply to Garfield. Journal of Consulting and Clinical Psychology, 57: 170–171.
Weisz, J.R., Weiss, B., Alicke, M.D., & Klotz, M.L. (1987). Effectiveness of psychotherapy with children and adolescents: A meta-analysis for clinicians. Journal of Consulting and Clinical Psychology, 55(4): 542–549.
Weisz, J.R., Weiss, B., & Donenberg, G.R. (1992). The lab versus the clinic: Effects of child and adolescent psychotherapy. American Psychologist, 47, 1578–1585.
Weisz, J.R., Weiss, B., Han, S.S., Granger, D.A., & Morton, T. (1995). Effects of psychotherapy with children and adolescents revisited: A meta-analysis of treatment outcome studies. Psychological Bulletin, 117: 450–468.
White House Conference. (2000). Meeting on the Safe Use of Medication to Treat Young Children.
Zito, J.M., Safer, D.J., dosReis, S., Gardner, J.F., Boles, M., & Lynch, F. (2000). Trends in the prescribing of psychotropic medications to preschoolers. Journal of the American Medical Association, 283(8): 1025–30.
NIH Publication Number 01-4985 Printed 2001
Footnote
- Treatment manuals provide a way to specify the intervention procedures, and can range from those that are highly prescriptive (with specific session-by-session activities) to those that provide a general framework for a treatment approach.
