FY 2024 Budget - Congressional Justification
National Institute of Mental Health
CONGRESSIONAL JUSTIFICATION FY 2024
National Institutes of Health
Department of Health and Human Services
- Director’s Overview
- IC Fact Sheet
- Major Changes
- Budget Mechanism Table
- Appropriations Language
- Summary of Changes
- Budget Graphs
- Organization Chart
- Budget Authority by Activity Table
- Justification of Budget Request
- Appropriations History
- Authorizing Legislation
- Amounts Available for Obligation
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
General Notes
- FY 2023 Enacted levels cited in this document include the effects of the FY 2023 HIV/AIDS transfer, as shown in the Amounts Available for Obligation table.
- Detail in this document may not sum to the subtotals and totals due to rounding
Director’s Overview

M.D., Ph.D.,
Director of NIMH
The National Institute of Mental Health (NIMH) is the lead federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
In the United States, an estimated 52.9 million adults struggle with a mental illness, which may be significantly impairing and life-threatening.1 Mental illnesses are the fifth leading cause of disability in the United States, accounting for 6.6 percent of all disability-adjusted life years.2 One of the most tragic outcomes of untreated mental illness is suicide. Suicide accounted for the loss of over 45,000 American lives in 2020 alone; it is the second leading cause of death in youth and young adults aged 10-34, and the twelfth leading cause of death overall.3 NIMH recognizes that the country is in the midst of an unprecedented mental health crisis,4 which disproportionately impacts various populations such as youth, veterans, marginalized communities, and individuals with existing mental illnesses – and supports the Administration’s efforts to address and respond to the needs of all Americans. NIMH is committed to confronting this crisis by supporting and conducting research that could transform how mental health is understood, and how mental health treatments and services are accessed, both in and out of healthcare settings.
As a key player in implementing the White House Report on Mental Health Research Priorities,5 NIMH is pursuing an ambitious and collaborative mission-focused research agenda, comprising a diverse portfolio of basic, translational, and clinical research, with the potential to improve clinical care over the short-, medium-, and long-term. By building upon and leveraging existing research and new initiatives, NIMH will continue to provide the evidence to accelerate scientific progress. In July 2022, NIMH published an update to its Strategic Plan for Research,6 expanding on Institute-wide diversity, equity, inclusion, and accessibility (DEIA) efforts and adding information about NIMH’s Approach to Mental Health Disparities Research7 and the new NIH-wide Climate Change and Health Initiative.8 NIMH also released the 2022 Progress Report on the Strategic Plan for Research,9 which highlights significant accomplishments made during FY 2021 toward achieving the goals described in the Strategic Plan. These accomplishments reflect NIMH’s sustained commitment to ensuring the relevance, timeliness, and real-world impact of the research that NIMH supports.
Enhancing the impact, reach, and accessibility of mental health services
Therapeutic and service delivery interventions to reduce suicide. NIMH supports research to evaluate the effectiveness of interventions to prevent or treat mental illnesses, improve the quality and outcomes of care, enhance service delivery, and communicate and implement evidence-based treatments across care settings. In 2021, NIMH launched the Practice-based Suicide Prevention Research Centers program, which is focused on developing, testing, and refining effective and scalable interventions at key intercepts in the chain of care.10 NIMH currently supports four Centers in various settings where suicide risk might be identified and addressed, such as health care systems, mental health and primary care practice and networks, and other systems and settings that serve individuals at risk for suicide (e.g., community settings, criminal justice systems).11,12,13,14 Researchers at one Center aim to develop and adapt practice-based and other suicide prevention interventions for underserved groups. Further, these researchers aim to design and test implementation strategies to optimize how evidence-based practices can be brought to scale effectively.10 NIMH also plans to support research on therapeutic and service delivery interventions that use interpersonal treatment strategies to reduce risk among individuals at risk for suicide following acute care.15 Many evidence-based strategies focus on intrapersonal factors (e.g., hopelessness, emotion dysregulation) and related coping strategies; however, interventions focused on interpersonal factors (e.g., social disconnection, perceived burdensomeness, few reasons for living) may help promote sustained remission and relapse prevention, as well as adherence to and engagement in care.
Protecting youth mental health. As detailed in the September 2021 NIMH Report to Congress “Addressing Youth Mental Health Disparities,”16 the NIMH Office for Disparities Research and Workforce Diversity has developed a Strategic Framework to guide research to address and reduce mental health disparities among underserved and underrepresented youth by 2031. The NIMH Strategic Framework for Addressing Youth Mental Health Disparities17 is structured to align with and supplement the NIMH Strategic Plan for Research,18 the NIH Minority Health and Health Disparities Strategic Plan,19 and the priorities of collaborating NIH Institutes, Centers, and Offices. The Framework provides a conceptual approach to help guide research and related activities on the mental health needs of youth impacted by racial and ethnic health disparities. The Framework describes NIMH’s plans for potential funding opportunities, as well as plans for outreach to stakeholders, including people with mental illnesses and their families, patient advocates and advocacy groups, health care providers, researchers, and state, local, and federal government partners. The Framework also identifies appropriate outcomes, metrics, and actions that will enable targeted research and accountability in the arena of youth mental health disparities. Through 2031, NIMH may periodically update the Framework based on stakeholder feedback, emerging challenges and opportunities, and research advances.
Personalized, early detection and screening for autism. Research shows that children who receive early screening for signs of autism spectrum disorder (ASD) and early intervention tend to have better daily functioning and well-being over the long-term. However, many families may not receive early screening and diagnosis due to disparities in access to care. Researchers in the NIMH-funded ASD Pediatric, Early Detection, Engagement and Services Research (PEDS) Network examined whether implementing an evidence-based, multistage screening procedure at federally funded early intervention sites could help address site-to-site variation and reduce disparities in ASD screening and diagnosis.20 The researchers developed a three-part screening and diagnosis process that included both clinicians and caregivers as key decision-makers, and found that ASD multistage screening was associated with a 60 percent increase in diagnoses compared with standard care. The most significant improvements in diagnoses occurred among Spanish-speaking families, compared with English-speaking families. These findings indicate that personalized early detection approaches can play a pivotal role in reducing existing health disparities.
Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY). Novel and transdisciplinary approaches are needed to develop, deliver, and improve mental health services to transform the care for individuals with severe psychiatric disorders. With support from the NIMH Division of Services and Intervention Research, the ALACRITY program focuses on practice-based research with potential for near-term impact, prioritizing a deployment-focused approach to speed the translation of research into practice, thus improving intervention effectiveness and service delivery.21 Since its establishment, the ALACRITY program has supported 14 research centers around the country which: focus on a variety of target populations and practice settings; cover a range of science, spanning intervention refinement and optimization through implementation and services research; and, incorporate a variety of transdisciplinary collaborations. Many of the centers leverage digital health platforms and data science methods to learn about mental illness onset and progression in clinical populations, improve diagnosis, monitor the course of illness, and deliver targeted interventions via mobile health technologies. Insights gained from ALACRITY Centers offer promise to advance innovation in practice-relevant research and offer resources that can be shared and adopted more broadly by the scientific community.
Extending the reach of NIMH research globally. NIMH-funded mental health research spans the globe, including projects in low- and middle-income countries (LMICs) funded through the NIMH Center for Global Mental Health Research (CGMHR).22 CGMHR focuses on strengthening the sustainable research capacity of LMICs and enhancing the potential for research advancements and multidirectional knowledge exchange.
Developing mental health interventions that are effective within and across diverse communities
Research along the autism spectrum: diverse research to meet diverse needs. To help all individuals with autism, NIMH is continuing efforts to diversify the autism research portfolio, including the full breadth of needs, across the lifespan.23 In addition to research on developing tools that can help identify autism in infants and toddlers as early as possible, NIMH supports efforts to improve the efficacy and availability of interventions. NIMH is funding research to understand how best to support paraprofessionals and other school-based care providers who work with children with autism with high service needs in elementary school settings. This research team seeks to determine the best way to help children better engage in academic tasks and will also measure the efficacy and practicality of this training in real-world educational settings.24 Other NIMH-funded researchers are testing the efficacy of theater-based programs to enhance social abilities and peer interactions in youth with autism.25 Tailored interventions like these have potential to address the issues that individuals on the autism spectrum and their families care deeply about, such as maximizing educational and social opportunities.
Personalizing deep brain stimulation (DBS) for treatment-resistant depression. The effectiveness of DBS as a treatment for neurological disorders such as Parkinson’s disease has led researchers to investigate whether it could also work for psychiatric disorders, such as treatment-resistant depression. However, since depression varies significantly among individuals, DBS treatment also needs to be personalized. Recently, researchers supported by NIMH examined whether they could personalize DBS to treat depression based on how an individual’s brain networks regulated mood and responded to stimulation.26 In this study, the researchers coupled stereo-electroencephalography, a method of placing recording electrodes within the brain to analyze brain network activity, with implantation of DBS leads to stimulate specific brain regions. The researchers used a holographic augmented reality platform to plan the placement of the DBS leads. One individual with severe treatment-resistant depression received eight months of treatment with personalized DBS stimulation parameters and demonstrated remission of depression-related symptoms and a dramatic improvement in quality of life. Significantly, the research team was able to access the relevant brain networks in ways that were never previously possible. These findings show initial evidence that this novel platform is feasible for performing personalized DBS and accessing brain networks in an unprecedented way. Although more research is needed, individuals that do not respond to conventional DBS as a treatment for treatment-resistant depression or a multitude of other neurological or psychiatric disorders may find this personalized approach to be more effective in improving health outcomes.
Enhancing technologies for noninvasive brain recording and stimulation. Transcranial magnetic stimulation (TMS) is a highly precise and noninvasive brain stimulation tool approved by the U.S. Food and Drug Administration for the treatment of major depression and other disorders. A research team led by investigators in the NIMH Intramural Research Program tested whether they could activate deep brain structures by stimulating connected surface-level structures.27 First, the researchers used imaging to map brain connections in each participant and identify the nearest TMS-accessible brain area that was connected to a deeper brain structure thought to be involved in depression. Next, they delivered a series of TMS pulses to the superficial region and measured participants’ brain activity in the hard-to-reach region through imaging. TMS pulses to the accessible region increased activity in the deep brain region, with more intense pulses resulting in even higher activity. This new approach to TMS offers a promising tool for precise, noninvasive stimulation of deep brain targets and could yield insights into neurocircuitry that advance both research and treatment.
Novel assays to address translational gaps in treatment development. Over the last decade, NIMH has aimed to improve the drug and device development pipeline by emphasizing the use of the experimental therapeutics approach, in which preclinical and clinical studies are designed to not only identify effective treatments, but also, critically, to gain knowledge about the biological mechanisms underlying mental illnesses. In alignment with this approach, NIMH is supporting research to objectively measure changes in brain physiology that reflect clinically relevant domains of function, such as cognitive function, impulsivity, and motivation.28 This research will include initial proof of concept studies focused on identifying objective measures, which researchers can then use to evaluate novel drug and device candidates and their targets in the brain, both in healthy humans and in preclinical animal species. Results from this research could significantly improve the efficiency of the therapeutic development process.
Embracing diversity and complexity in basic research on mental illnesses
Precision Psychiatry Initiative. Effective treatments for mental illnesses exist, yet tailoring treatment for individuals is often a trial-and-error process that can lead to unacceptable delays in receiving effective treatment. To address this pressing challenge, NIMH plans to launch a new Precision Psychiatry Initiative, an ambitious research program that will focus on two parallel areas of need: biomarker development and precision diagnostics. The goal of the biomarker development effort is to deliver highly sensitive and specific biomarkers to guide treatment decisions for major depression. This effort will be milestone-based, meaning that only projects demonstrating promising results will continue to be funded. The biomarker development effort will be divided into three phases, culminating in a large-scale prospective clinical trial with a focus on generalizability for underserved populations and populations experiencing health disparities. Meanwhile, the precision diagnostics effort will support studies that follow large (100,000+), diverse cohorts of individuals over time using novel behavioral and physiological methods to better predict patient prognosis and optimize treatment. These studies will combine innovative methods for assessing behavior (such as mobile device-based measurement of cognition and activity) with detailed clinical information from electronic health records to identify longitudinal relationships among symptoms of mental illnesses, biological systems, behavior, and day-to-day functioning. Research conducted as part of the precision diagnostics effort will also focus on developing and testing quantitative, clinically relevant tools for use by clinicians in making treatment recommendations for individual patients, leading to better understanding and more effective treatments for mental illnesses.
COVID-19 risks for people with serious mental illness (SMI). As we learn more about COVID-19 illness, recovery, and the effectiveness of vaccination, public health experts are turning their attention from the general public to those most at risk from infection. One major risk factor is SMI. Researchers have documented that people with SMI are not only more likely to get COVID-19 compared to the general population, they are also more likely to suffer from severe COVID-19, require hospitalization, and die. A recent study examining electronic health records and COVID-19 outcomes among American adults showed that adults with a recent diagnosis of depression or schizophrenia had a seven-fold increased likelihood of COVID-19 infection.29 These individuals died at nearly twice the rate of those without a mental disorder, and the risks were even greater for African Americans with SMI. Additionally, although vaccines are a highly effective tool to mitigate COVID-19 risk, research shows that vaccinated people with SMI remain at increased risk of SARS-CoV-2 infection compared to vaccinated people without SMI.30 NIMH is supporting research to address urgent mental health research questions related to COVID-19, including broader secondary impacts of the pandemic as well as research on the intersection of mental health, COVID-19, and HIV.31 Research focused on vulnerable populations, including those who experienced disparities in health outcomes prior to the pandemic and report increased symptoms of mental illnesses during the pandemic, will be of great importance.
Novel approaches to eliminate HIV from the central nervous system. HIV attacks the immune system by infecting a type of white blood cell in the body that is vital to fighting off infection. New therapies to treat and cure HIV are difficult to develop as HIV can enter a dormant-like state in the brain, evading detection and treatment only to reactivate at a later date. In a new study supported by NIMH, researchers used exosomes, tiny nanoparticles capable of being taken up by cells, to deliver a novel HIV-repressing protein into the cells of mice infected with HIV.32 The exosomes can cross the blood-brain barrier to enter into the brain, enabling the treatment to effectively target this notoriously hard-to-reach organ. When researchers administered this exosome-based treatment to mice infected with HIV, they found that the novel protein attached to HIV’s genetic material and prevented it from replicating, resulting in reduced levels of HIV in the bone marrow, spleen, and brain. This innovative technology could be used in the future as a delivery method to treat various other diseases of the brain such as Parkinson’s disease, Alzheimer’s disease, and addiction.
Understanding the genetic basis of mental illnesses. Examining common genetic variations in the genomes (or complete set of DNA) of people with bipolar disorder is a way that scientists can hone in on the genetic factors that are likely to play a causal role in the disorder. In the largest genome-wide association study (GWAS) of bipolar disorder to date, NIMH-funded researchers analyzed genomic data from participants across Europe, North America, and Australia, including over 40,000 individuals with bipolar disorder and over 370,000 individuals without bipolar disorder. The researchers identified common genetic variations that are more likely to occur in people with bipolar disorder — about twice as many genetic locations as reported in previous studies.33 The two diagnostic subtypes of bipolar disorder shared substantial but incomplete genetic overlap with each other, with one subtype showing a stronger genetic correlation with schizophrenia and the other subtype showing a stronger genetic correlation with major depressive disorder. The study also found genetic correlations between bipolar disorder and certain traits such as alcohol use, smoking, and sleep impairments. These and other genome-wide findings could help improve the understanding of the biological origins of bipolar disorder and suggest some genes promising for further research.
Identifying biomarkers for mental illnesses and neurodevelopmental disorders. NIMH supports a wide range of compelling science through its Small Business Innovation Research (SBIR) program.34 One area of NIMH-supported SBIR research that has become particularly interesting in recent years is biomarker development.35 As one example, NIMH is supporting a biomarker project focused on the early identification of ASD.36 This project aims to optimize a powerful brain imaging technique for easier and wider use by clinicians in real-world settings. In another project, NIMH-supported researchers are using a virtual reality-based tool to develop behavioral biomarkers of cognitive function in people with schizophrenia.37 By simulating everyday activities, this approach could help to ensure that new treatments aimed at improving cognition do so in ways that matter in the real world.
Understanding the functions of non-neuronal cell types. Glial cells (i.e., astrocytes, oligodendrocytes, and microglia) are cells in the central nervous system that support and complement the functions of neurons. For example, astrocytes may regulate cognitive functions by releasing gliotransmitters that activate hundreds of neuronal synapses at once. There are major gaps in the understanding of how neurons and glial cells function collectively, and neuroscience research to date has focused heavily on neurons. However, recent advances in technology have enabled powerful new experimental approaches to understanding glial cells, such as selectively expressing designer proteins in glial cells to precisely locate and count these cells, record their activity, and manipulate their functions. NIMH is supporting research that combines these novel experimental approaches with computational modeling to rigorously test mechanistic hypotheses on how neurons and glia function together to enable cognition, emotion, and social behaviors.38 Advances in this area of research could provide new perspectives on how neuro-glia interactions enable complex behavior, and how they become altered in mental illnesses.
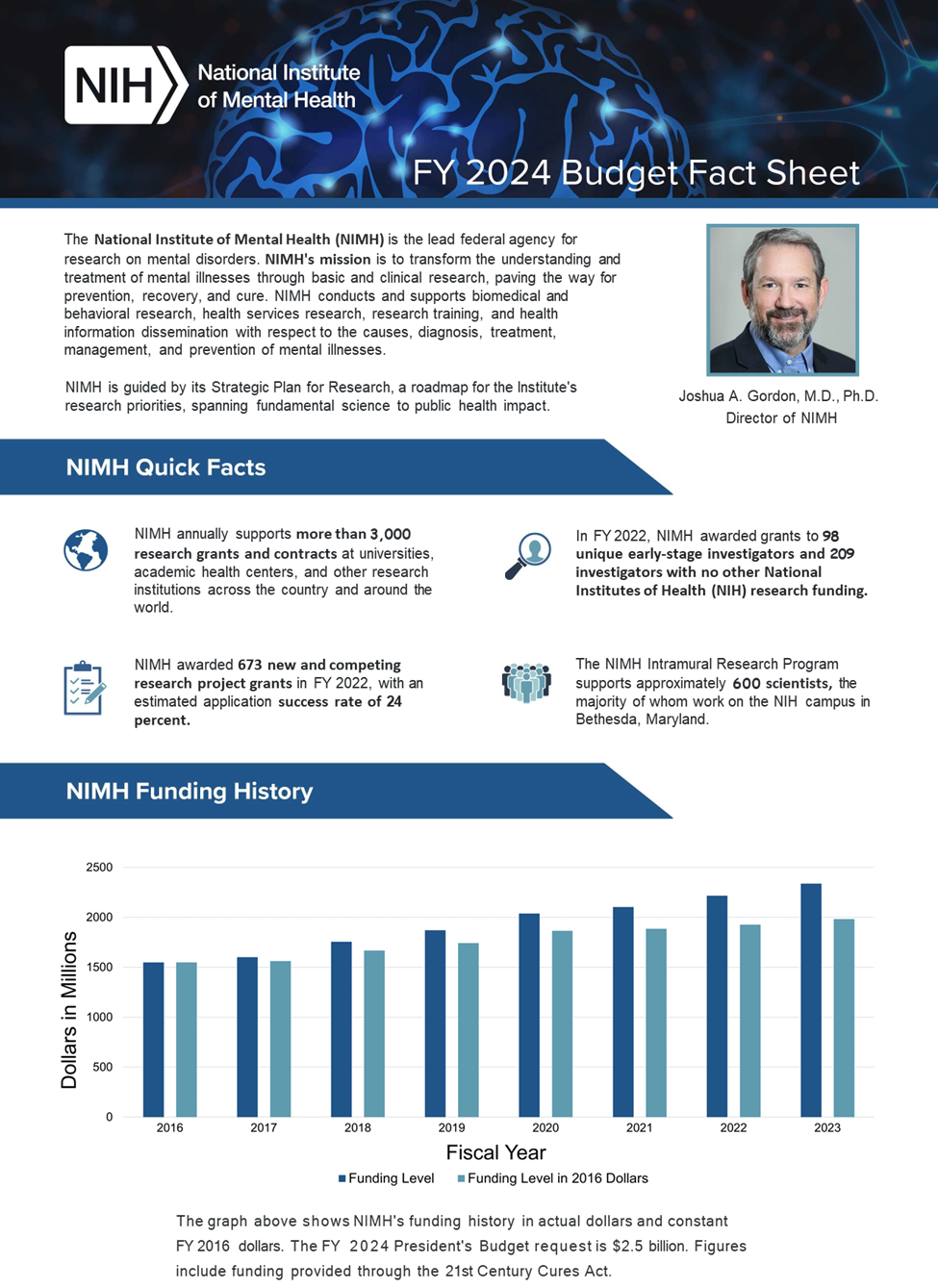

Find an accessible version of the FY 2024 Budget Fact Sheet.
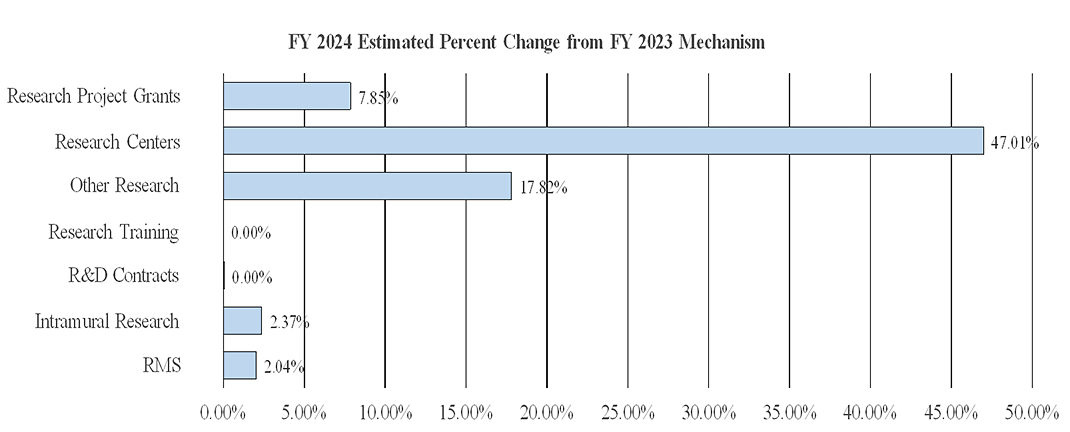
Major Changes
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity details and these highlights will not sum to the total change for the FY 2024 President’s Budget request for NIMH. The FY 2024 President’s Budget request is $2,541.7 million, an increase of $200.0 million compared to the FY 2023 Enacted level. The request includes $86.0 million provided through the 21st Century Cures Act.
Research Project Grants (+$127.1 million; total $1,745.5 million)
NIMH expects to increase funding for non-competing Research Project Grants by $45.2 million to fund projects receiving competing awards in prior years. Competing Research Project Grants are expected to increase by 200 grants or $74.6 million. This increase is distributed across all programmatic areas and basic, translational, or clinical research.
Research Centers (+$43.9 million; total $137.3 million)
NIMH expects to increase funding for Research Centers by $43.9 million to support additional ALACRITY Centers, Practice Based Suicide Prevention Research Centers, and additional Centers supporting therapeutic and service delivery interventions.
Other Research (+$21.3 million; total $140.6 million)
NIMH expects to increase funding in Other Research by $21.3 million to support coordinating research projects in support of the Precision Psychiatry Initiative.
Intramural Research Programs (+$5.6 million; total $241.6 million)
NIMH expects to increase funding for Intramural Research by $5.6 million, and will accelerate innovative research studies conducted by the Institute’s intramural scientists.
Research Management and Support (+$2.2 million; total $109.5 million)
NIMH expects to increase funding for Research Management and Support by $2.2 million and will continue to support the oversight and management of scientific programs critical to fulfilling the Institute’s mission.
Budget Mechanism Table
| Mechanism | FY 2022 Final3 | FY 2022 Enacted | FY 2024 Presidents Budget | FY 2024 +/- FY 2023 | ||||
|---|---|---|---|---|---|---|---|---|
| Number | Amount | Number | Amount | Number | Amount | Number | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 1,629 | $941,126 | 1,756 | $1,082,893 | 1,708 | $1,128,104 | -48 | $45,211 |
| Administrative Supplements | (143) | $18,680 | (135) | $17,840 | (135) | $17,840 | (0) | $0 |
| Competing: | ||||||||
| Renewal | 60 | $43,006 | 53 | $37,454 | 54 | $33,103 | 1 | -$4,351 |
| New | 613 | $468,859 | 575 | $407,926 | 774 | $486,917 | 199 | $78,991 |
| Supplements | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Subtotal Competing | 673 | $511,865 | 628 | $445,380 | 828 | $520,020 | 200 | $74,640 |
| Subtotal RPGs | 2,302 | $1,471,670 | 2,384 | $1,546,113 | 2,536 | $1,665,964 | 152 | $119,851 |
| SBIR/STTR | 90 | $68,560 | 98 | $72,341 | 105 | $79,544 | 7 | $7,203 |
| Research Project Grants | 2,392 | $1,540,231 | 2,482 | $1,618,454 | 2,641 | $1,745,508 | 159 | $127,054 |
| Research Centers | ||||||||
| Specialized/Comprehensive | 39 | $82,676 | 43 | $93,116 | 63 | $137,028 | 20 | $43,912 |
| Clinical Research | 0 | $0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Comparative Medicine | 0 | $299 | 0 | $299 | 0 | $299 | 0 | $0 |
| Research Centers in Minority Institutions | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers | 39 | $82,975 | 43 | $93,415 | 63 | $137,327 | 20 | $43,912 |
| Other Research | ||||||||
| Research Careers | 379 | $65,348 | 377 | $65,803 | 377 | $65,083 | 0 | $0 |
| Cancer Education | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Cooperative Clinical research | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Biomedical Research Support | 3 | $1,388 | 0 | $0 | 0 | $0 | 0 | $0 |
| Minority Biomedical Research Support | 0 | $701 | 0 | $701 | 0 | $701 | 0 | $0 |
| Other | 70 | $53,548 | 66 | $53,513 | 93 | $74,766 | 27 | $21,254 |
| Other Research | 452 | $120,985 | 443 | $119,297 | 470 | $140,550 | 27 | $21,254 |
| Total Research Grants | 2,883 | $1,744,190 | 2,968 | $1,831,165 | 3,174 | $2,023,385 | 206 | $192,220 |
| Ruth L. Kirschstein Training Awards | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 282 | $13,431 | 287 | $13,687 | 281 | $13,687 | -6 | $0 |
| Institutional Awards | 475 | $29,739 | 524 | $32,853 | 513 | $32,853 | -11 | $0 |
| Total Research Training | 757 | $43,169 | 811 | $46,540 | 794 | $46,540 | -17 | $0 |
| Research and Develop Contracts | 128 | $104,190 | 133 | $120,594 | 133 | $120,594 | 0 | $0 |
| (SBIR/STTR)(non-add) | (0) | ($715) | (0) | ($715) | (0) | ($721) | (0) | ($5) |
| Intramural Research | 288 | $226,553 | 300 | $236,023 | 300 | $241,613 | 0 | $5,590 |
| Res. Management and Support | 291 | $102,568 | 289 | $107,331 | 297 | $109,522 | 8 | $2,191 |
| (SBIR Admin) (non-add) | ($0) | ($135) | ($135) | ($0) | ||||
| Construction | $0 | $0 | $0 | $0 | ||||
| Buildings and Facilities | $0 | $0 | $0 | $0 | ||||
| Total NIMH | 579 | $2,220,670 | 589 | $2,341,653 | 597 | $2,541,653 | 8 | $200,000 |
1 All items in italics and brackets are non-add entries.
2 Of which $76.0 million in FY 2022, $225.0 million in FY 2023, and $86.0 million in FY 2024 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
3 Includes 21st Century Cures Act funding not obligated in FY 2022 and carried into FY 2023.
Appropriations Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, [$2,112,843,000]$2,455,653,000.
NIH INNOVATION ACCOUNT, CURES ACT
(INCLUDING TRANSFER OF FUNDS)
For necessary expenses to carry out the purposes described in section 1001(b)(4) of the 21st Century Cures Act, in addition to amounts available for such purposes in the appropriations provided to the NIH in this Act, [$1,085,000,000] $407,000,000, to remain available until expended: Provided, That such amounts are appropriated pursuant to section 1001(b)(3) of such Act, are to be derived from amounts transferred under section 1001(b)(2)(A) of such Act, and may be transferred by the Director of the National Institutes of Health to other accounts of the National Institutes of Health solely for the purposes provided in such Act: Provided further, That upon a determination by the Director that funds transferred pursuant to the previous proviso are not necessary for the purposes provided, such amounts may be transferred back to the Account: Provided further, That the transfer authority provided under this heading is in addition to any other transfer authority provided by law.
[Top]
Summary of Changes
| FY 2023 Enacted | $2,341,653 |
|---|---|
| FY 2024 President's Budget | $2,541,653 |
| Net Change | $200,000 |
| CHANGES | FY 2023 Enacted | FY 2024 President's Budget | Built in change from FY 2023 Enacted | |||
|---|---|---|---|---|---|---|
| FTE's | Budget Authority | FTE's | Budget Authority | FTE's | Budget Authority | |
| A. Built-in: | ||||||
| 1. Intramural Research: | ||||||
| a. Annualization of FY 2023 pay & benefits increase | $83,162 | $87,698 | $923 | |||
| b. FY 2024 pay & benefits increase | $83,162 | $87,698 | $3,189 | |||
| c. Paid days adjustment | $83,162 | $87,698 | $320 | |||
| d. Differences attributable to change in FTE | $83,162 | $87,698 | $0 | |||
| e. Payment for centrally furnished services | $37,338 | $38,223 | $884 | |||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs |
$115,523 | $115,692 | $2,525 | |||
| Subtotal | $7,842 | |||||
| 2. Research Management and Support: | ||||||
| a. Annualization of FY 2023 pay & benefit increase | $52,275 | $56,555 | $578 | |||
| b. FY 2024 pay & benefits increase | $52,275 | $56,555 | $2,001 | |||
| c. Paid days adjustment | $52,275 | $56,555 | $201 | |||
| d. Differences attributable to change in FTE | $52,275 | $56,555 | $1,499 | |||
| e. Payment for centrally furnished services | $6,,950 | $7,062 | $111 | |||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs |
$48,105 | $45,905 | $1,030 | |||
| Subtotal | $5,420 | |||||
| Subtotal, Built-in | $13,262 | |||||
| CHANGES | FY 2023 Enacted | FY 2024 President's Budget | Program change from FY 2023 Enacted | |||
| No. | Amount | No. | Amount | No. | Amount | |
| B. Program: | ||||||
| 1. Research Project Grants: | ||||||
| a. Noncompeting | 1,756 | $1,100,733 | 1,708 | $1,145,944 | -48 | $45,211 |
| b. Competing | 628 | $445,380 | 828 | $520,020 | 200 | $74,640 |
| c. SBIR/STTR | 98 | $72,341 | 105 | $79,544 | 7 | $7,203 |
| Subtotal, RPGs | 2,482 | $1,618,454 | 2,641 | $1,745,508 | 159 | $127,054 |
| 2. Research Centers | 43 | $93,415 | 63 | $137,327 | 20 | $43,912 |
| 3. Other Research | 443 | $119,297 | 470 | $140,550 | 27 | $21,254 |
| 4. Research Training | 811 | $46,540 | 794 | $46,540 | -17 | $0 |
| 5. Research and development contracts | 133 | $120,594 | 133 | $120,594 | 0 | $0 |
| Subtotal, Extramural | $1,998,299 | $2,190,519 | $192,220 | |||
| FTEs | FTEs | FTEs | ||||
| 6. Intramural Research | 300 | $236,023 | 300 | $241,613 | 0 | -$2,252 |
| 7. Research Management and Support | 289 | $107,331 | 297 | $109,522 | 8 | -$3,230 |
| 8. Construction | $0 | $0 | $0 | |||
| 9. Buildings and Facilities | $0 | $0 | $0 | |||
| Subtotal, Program | 589 | $2,341,653 | 597 | $2,541,653 | 8 | $186,738 |
| Total built-in and program changes | $200,000 | |||||
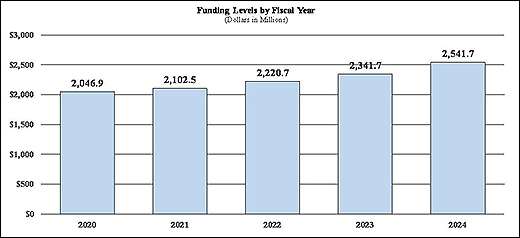
Budget Graphs
History of Budget Authority and FTEs:
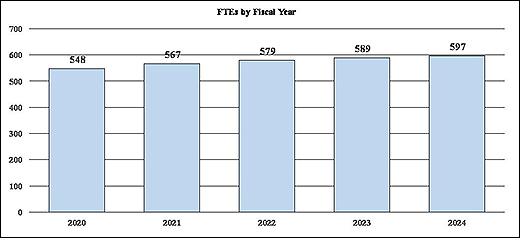
Distribution by Mechanism:
Change by Selected Mechanism:
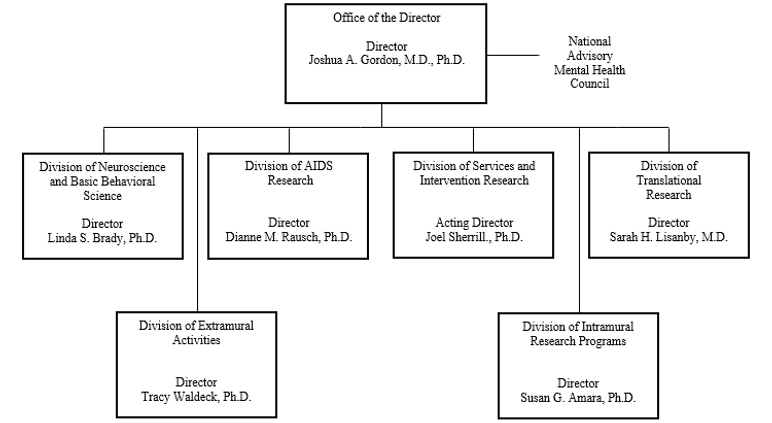
Organization Chart
National Institutes of Health
National Institute of Mental Health
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
Budget Authority by Activity
| Extramural Research | FY 2022 Final | FY 2023 Enacted | FY 2024 President's Budget | FY 2024 +/- FY 2023 Enacted | ||||
|---|---|---|---|---|---|---|---|---|
| FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount | |
| Detail | ||||||||
| Neuroscience & Basic Behavioral Science | $817,824 | $873,490 | $961,343 | $87,853 | ||||
| Services & Intervention Research | $239,362 | $255,654 | $271,245 | $15,591 | ||||
| Translational Research | $539,912 | $576,662 | $648,641 | $71,979 | ||||
| AIDS Research | $183,132 | $173,598 | $176,028 | $2,430 | ||||
| Office of the Director | $111,318 | $118,895 | $133,261 | $14,366 | ||||
| Subtotal, Extramural | $1,891,549 | $1,998,299 | $2,190,519 | $192,220 | ||||
| Intramural Research | 288 | $226,553 | 300 | $236,023 | 300 | $241,613 | 0 | $5,590 |
| Research Management & Support | 291 | $102,568 | 289 | $107,331 | 297 | $109,522 | 8 | $2,191 |
| Total | 579 | $2,220,670 | 589 | $2,341,653 | 597 | $2,541,653 | 8 | $200,000 |
1Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
Justification of Budget Request
National Institute of Mental Health
Authorizing Legislation: Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2022 Final | FY 2023 Enacted | FY 2024 President’s Budget | FY 2024 +/- FY 2023 | |
|---|---|---|---|---|
| BA | $2,220,670,00 | $2,314,653,000 | $2,541,653,000 | +$200,000,000 |
| FTE | 579 | 589 | 597 | +8 |
[Top]
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Overall Budget Policy: The FY 2024 President’s Budget request is $2,541.7 million, an increase of $200.0 million or 8.5 percent compared to the FY 2023 Enacted level. The $200.0 million increase includes $20.0 million to increase studies of the social media impact on mental health, $50.0 million to support the Precision Psychiatric Initiative, and $130.0 million to accelerate better diagnostics, improved treatments, and enhanced precision of mental health care.
Program Descriptions
Office of the Director
The NIMH Office of the Director (OD) leads the Institute in carrying out the NIMH mission to transform the understanding and treatment of mental illnesses. The OD provides scientific leadership, sets programmatic priorities, coordinates cross-cutting programs, determines Institute policies, directly funds several research projects, and provides overall administrative and operational coordination for the Institute. The OD houses nine offices: Office on AIDS; Office of Autism Research Coordination; Office of Clinical Research; Office of Genomics Research Coordination; Office for Disparities Research and Workforce Diversity; Office of Management; Office of Rural Mental Health Research; Office of Science Policy, Planning, and Communications; and Office of Technology Development and Coordination. Each of the offices within the OD plays an important role in supporting the Institute.
As an example of research that the OD prioritizes, NIMH is supporting research to better understand factors that confer risk and resilience for suicide among Black youth,39 whose rates of suicide have risen sharply in recent years.40 Understanding how social determinants of health interact with biological and behavioral risk and protective factors is a necessary step in identifying underlying mechanisms that can inform the development of effective suicide prevention strategies for Black youth. In alignment with the National Action Alliance for Suicide Prevention, NIMH continues to pursue the goal of reducing the rate of suicide in the United States by 20 percent by the year 2025.41 Suicide is the second leading cause of death for youth aged 10-24 years, and certain subgroups of youth are at significantly elevated risk, so focusing research efforts on high-risk youth is critical to achieving this goal. Similarly, NIMH is supporting research to understand risk and resilience for mental illnesses in Asian American, Native Hawaiian, and Pacific Islander subpopulations.42
Budget Policy: The FY 2024 President’s Budget request is $133.3 million, an increase of $14.4 million or 12.1 percent compared with the FY 2023 Enacted level.
Program Portrait – Social Media Impacts on Youth Mental Health.
In December 2021, the U.S. Surgeon General issued an Advisory on Youth Mental Health, which highlighted the urgent need to address the nation’s youth mental health crisis.43 The advisory called special attention to the need for rigorous research on how youth engage with social media, gaming, and a wide variety of online images and content. As youth technology use has become ubiquitous, there is growing evidence that social media use can contribute to poor health outcomes, including risks to mental and behavioral health. Recognizing these risks, NIMH is working to identify research gaps and opportunities for understanding relationships among social media behavior, social media engagement, social context, and youth mental health.44 Evolving methods for digital data collection, including keystroke logging, image and voice analysis, GPS, and accelerometer data, as well as advances in bioinformatics and computational approaches, have made research on digital behaviors more tractable, and these methods are ready for use in social media research. Further insight is needed to understand the role of digital social interactions in youth social development and their contributions to risk and resilience for psychopathology, as well as how social media behaviors may interact with the efficacy and effectiveness of mental health interventions. The research spurred by this concept could lead to identification of risk and protective factors for social media use in youth that in turn could inform potential targets for novel and improved interventions
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) supports research in the areas of basic molecular and cellular neuroscience, genetics, integrative neuroscience, research training, and drug discovery. In cooperation with other NIMH programs and the wider research community, the Division ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, could be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance understanding of the basic neurobiology underlying mental illnesses. Looking forward, DNBBS plans to support a broad, coordinated effort to understand how genetic alterations found in individuals with a mental illness act in brain cells to cause changes in cellular and circuit function and ultimately behavior. In addition, DNBBS will build on a portfolio of research to understand the development of brain circuits underlying cognitive, affective, and social behavior.
Budget Policy: The FY 2024 President’s Budget request is $961.3 million, an increase of $87.9 million or 10.1 percent compared with the FY 2023 Enacted level.
Program Portrait – Suicide Prevention Research
Suicide is a major public health concern, claiming over 45,000 American lives in 2020 alone.45 NIMH-funded researchers are developing and testing the effectiveness of service-ready tools to prevent suicide, including strategies to improve suicide risk detection. In one study, researchers are examining the effectiveness of a suicide risk model that combines data from health records and self-report screening questionnaires to improve risk detection among adults in three large healthcare systems.46 Further, the researchers aim to provide implementation guidance so that the suicide risk model can be adopted and sustained in other healthcare and community settings.
Improving risk detection is particularly important for Black youth, as suicide rates are on the rise for these individuals.47 NIMH is supporting research to understand suicide risk and protective factors among Black youth, including research aimed at optimizing suicide risk detection and interventions. NIMH-funded researchers are testing the effectiveness of a systems-level approach, WeCare, to assessing and intervening in emergency departments with Black youth identified as being at risk for suicide.48 WeCare combines the NIMH-supported computerized adaptive screen for suicidal youth (CASSY) with Safe Alternative for Teens and Youth – Acute, a family-oriented suicide prevention intervention that includes Safety Planning, referral to outpatient mental health care, and culturally-adapted text messages to youth and caregivers across a 4-week period.49 A system of care that links Black youth at risk for suicide with quality mental health services has the potential to increase risk identification, treatment referral and engagement, and, in turn, reduce suicide.
Translational Research
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science to discover the causes, mechanisms, and trajectories of mental illnesses, and to develop effective interventions for individuals across the lifespan. DTR supports research using innovative forms of scientific analysis, including computational psychiatry and machine learning, to elucidate the characteristics of, and risk factors for, mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and, the design and testing of innovative treatments and interventions. As such, DTR-supported research efforts may have intermediate-term impact and pave the way towards effective treatment and prevention for mental illnesses.
One area of high priority for DTR is to fund research to improve outcomes for individuals at clinical high risk (CHR) for psychosis. A major knowledge gap has been the lack of a means to reliably predict which individuals with CHR will develop schizophrenia or other adverse outcomes. Such knowledge could enable the implementation of effective prevention strategies. To address this gap, NIMH and the Foundation for NIH launched a major public-private partnership to develop the tools that are needed for early therapeutic interventions for people at risk of developing schizophrenia and other outcomes of CHR associated with significant disability.
The Accelerating Medicines Partnership® – Schizophrenia (AMP® SCZ)50 brings together the NIH, the Food and Drug Administration, and numerous private and non-profit organizations to join forces in an unprecedented effort to prevent the development of schizophrenia and other outcomes of CHR. AMP SCZ seeks to achieve this goal by developing a set of validated biomarkers that can identify individuals at risk for schizophrenia, and identify novel targets for treatment development. This flagship study builds upon the successes of prior investments to identify biomarkers of risk for progression to schizophrenia, including the North American Prodrome Longitudinal Study (NAPLS) which identified promising biomarkers of risk 51,52 and developed a risk calculator to predict conversion to psychosis.53 In addition, DTR, in collaboration with the Department of Defense, private foundations, and industry, supports the Advancing Understanding of RecOvery afteR traumA (AURORA) Study,54 a landmark study to understand the consequences of trauma, as well as research using advanced digital techniques, including natural language processing,55 machine learning, and predictive coding,56 that aim to predict mental health outcomes, such as risk for suicide. DTR also supports work harnessing the latest advances in artificial intelligence to advance mechanistic understanding of how circuits in the brain shape behavior.57
Budget Policy: The FY 2024 President’s Budget request is $648.6 million, an increase of $72.0 million or 12.5 percent compared with the FY 2023 Enacted level.
Services and Intervention Research
The Division of Services and Intervention Research (DSIR) supports research that evaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental illnesses. DSIR refines and evaluates interventions for children, adolescents, and adults, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research to improve the quality and outcomes of care; organization- and system-level interventions to enhance service delivery; and, strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings.
DSIR initiatives encourage practice-based research with near-term potential for improving intervention effectiveness and service delivery, as illustrated by key research programs. For example, the Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Centers aim to advance clinical practice and generate knowledge that will fuel transformation of mental health care in the United States (for additional details, see the above Program Portrait and Director’s Overview). A related Center program supports “Practice-Based Suicide Prevention Research Centers,” that address NIMH suicide prevention research priorities and goals to reduce the national suicide rate (for additional details, see the Director’s Overview).63,64
Budget Policy: The FY 2024 President’s Budget request is $271.2 million, an increase of $15.6 million or 6.1 percent compared with the FY 2023 Enacted level.
Program Portrait – Improving the Quality of Services for Serious Mental Illness.
The Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Center program aims to support innovative research ideas and transdisciplinary collaborations that could transform the care of children, adolescents, and adults with severe psychiatric disorders.58,59 ALACRITY-funded researchers seek to increase the effectiveness of existing interventions; improve the delivery and quality of evidence-based services; and accelerate the implementation and continuous improvement of new practices among key populations and in diverse health care settings. Since 2020, NIMH has begun funding six new ALACRITY Centers, which focus on a range of populations and settings.
The Early Psychosis Intervention Network (EPINET) is a learning health system for early psychosis, aimed at enhancing effective coordinated specialty care delivery to people with symptoms of early psychosis, and promoting new research to improve diagnosis, interventions, and outcomes in the early stages of serious mental illness. EPINET’s eight scientific hubs, which include more than 100 coordinated specialty care clinics in 17 states, and its National Data Coordinating Center, support practice-based research to improve early identification, diagnosis, clinical assessment, intervention effectiveness, service delivery, and health outcomes in clinics offering evidence-based specialty care to persons in the early stages of psychotic illness.60,61,62 Through coordinated efforts including the use of common data elements, data sharing, and a unified informatics approach, EPINET’s research network aims to drive continuous improvement and innovation in care delivery and scientific discovery.
The Division of AIDS Research (DAR) supports research and research training that addresses the priority areas outlined in the NIH Strategic Plan for HIV and HIV-Related Research65 and the HHS National HIV/AIDS Strategy.66 DAR-supported research includes behavioral, social, data, and communications science studies aimed at reducing HIV/AIDS incidence through the development, testing, and implementation of new and improved prevention strategies, and improving health outcomes and reducing health disparities of those living with HIV through improved linkage to care and adherence to effective treatments. DAR also supports research to understand, prevent, and treat the neurological and mental disorders associated with living with HIV. DAR is participating in cure research by supporting studies to eradicate or silence HIV from biological reservoirs in the central nervous system (CNS), where the virus may evade detection and treatment. HIV latency in the CNS is critically important to consider in studies of eradication and reactivation. Many drugs designed to eradicate the virus are unable to penetrate the blood-brain barrier of the CNS, thus providing a protective reservoir for HIV. DAR places a strong emphasis on targeted research to understand the mechanisms underlying HIV-induced neuronal pathology and the resulting motor, cognitive, and psychiatric dysfunction that results, with the goal of identifying preventive and therapeutic interventions.
DAR research also places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for contracting HIV or negatively impact the health outcomes of those living with HIV. Additionally, DAR engages with multidisciplinary expertise in NIH-wide planning efforts to ensure effective integration of behavioral and biomedical approaches to help achieve an AIDS-free generation.
Budget Policy: The FY 2024 President’s Budget request is $176.0 million, an increase of $2.4 million or 1.4 percent compared with the FY 2023 Enacted level.
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research using unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of basic, translational, and clinical scientists.
IRP researchers are developing new and improved methods in functional magnetic resonance imaging (fMRI)67 and exploring advanced computational methods to evaluate brain function and mental illnesses. The IRP supports research to combine neuroimaging and recording modalities such as fMRI and electroencephalography (EEG), magnetoencephalography and EEG, and simultaneous positron emission tomography (PET)-MRI. Many IRP researchers use fMRI and behavioral tasks to investigate differences in brain circuitry underlying key brain functions such as learning, perception, and attention, which are affected in mental illnesses. For example, researchers are combining fMRI with electrophysiological techniques in an animal model to understand how the brain recognizes faces, which is relevant to social anxiety and autism.68
IRP investigators have contributed to the NIMH Healthy Research Volunteer Dataset, an in-depth and reliable collection of phenotypic clinical data, including blood and urine assays, five different modes of neuroimaging, mental health assessments, cognitive functioning, and more69. Sharing this dataset in publicly available repositories, which will be added to regularly, will facilitate new secondary research questions and increase the scientific yield from this intramural effort. IRP scientists are also exploring novel medications and other treatments for depression in adults, including ketamine and other experimental fast-acting antidepressant medications, transcranial magnetic stimulation (TMS), and next generation seizure therapy. Using clinical assessments, brain imaging, and sleep studies, these researchers aim to better understand suicide.70 IRP researchers also developed the Ask Suicide-Screening Questions (ASQ) tool for use among both youth and adults, and they continue to validate the tool in different languages, health systems, and settings, including a clinical pathway for suicide screening in adult primary care settings.71,72
Budget Policy: The FY 2024 President’s Budget request is $241.6 million, an increase of $5.6 million or 2.4 percent compared with the FY 2023 Enacted level.
Research Management and Support
Research Management and Support (RMS) activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research and training grants, and research and development contracts. RMS functions include strategic planning, coordination, and evaluation of NIMH programs, regulatory compliance, coordination of global mental health efforts, and liaising with other Federal agencies, Congress, and the public. Through RMS activities, NIMH continues to provide accountability and administrative support for meritorious basic, clinical, and translational research and continues to promote health information dissemination, education, and outreach activities. RMS also supports outreach activities to connect the public with evidence-based mental health information. For example, in recognition of National Suicide Prevention Awareness Month (September), NIMH promoted brochures, fact sheets, and graphics;73 highlighted the new 988 Suicide & Crisis Lifeline;74 and, co-hosted a Facebook Live event with the National Institute on Drug Abuse on the intersection of suicide and substance use.75 Information is presented in plain language and suitable for a lay audience, and many materials are available in Spanish language to reach a broader audience.
Budget Policy: The FY 2024 President’s Budget request is $109.5 million, an increase of $2.2 million or 2.0 percent compared with the FY 2023 Enacted level.
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2015 | $1,440,076,000 | $1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017 1 | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,601,931,000 |
| Rescission | $0 | |||
| 2018 2 | $1,244,901,000 | $1,668,461,000 | $1,724,568,000 | $1,754,775,000 |
| Rescission | $0 | |||
| 2019 2 | $1,612,192,000 | $1,790,231,000 | $1,871,250,000 | $1,870,296,000 |
| Rescission | $0 | |||
| 2020 2 | $1,630,422,000 | $1,961,704,000 | $2,076,244,000 | $2,038,374,000 |
| Rescission | $0 | |||
| 2021 2 | $1,844,865,000 | $2,060,303,000 | $2,139,491,000 | $2,103,708,000 |
| Rescission | $0 | |||
| 2022 2 | $2,213,574,000 | $2,223,085,000 | $2,218,900,000 | $2,216,976,000 |
| Rescission | $0 | |||
| 2023 2 | $2,210,828,000 | $2,428,775,000 | $2,332,672,000 | $2,337,843,000 |
| Rescission | $0 | |||
| 2024 2 | $2,541,653,000 |
1 Budget Estimate to Congress includes mandatory financing.
2 Includes funds derived by transfer from the NIH Innovation Account under the 21st Century Cures Act
[Top]
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2023 Amount Authorized | FY 2023 Enacted | 2024 Amount Authorized | FY 2024 President’s Budget | |||
|---|---|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | $2,341,653,000 | Indefinite | $2,541,653,000 | ||
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total Budget Authority | $2,341,653,000 | $2,541,653,000 | ||||||
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2022 Final |
FY 2023 Enacted |
FY 2024 President's Budget |
| Appropriation | $2,216,976 | $2,337,843 | $2,541,653 |
| OAR HIV/AIDS Transfers | $3,694 | $3,810 | $0 |
| Subtotal, adjusted budget authority | $2,220,670 | $2,341,653 | $2,541,653 |
| Unobligated balance, start of year | $2,338 | $10,270 | $0 |
| Unobligated balance, end of year (carryover) | -$10,270 | $0 | $0 |
| Subtotal, adjusted budget authority | $2,212,738 | $2,351,923 | $2,541,653 |
| Unobligated balance lapsing | -$18 | $0 | $0 |
| Total obligations | $2,212,720 | $2,351,923 | $2,541,653 |
1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2022 - $6,871 FY 2023 - $10,050 FY 2024 - $10,050
[Top]
Budget Authority by Object Class
(Dollars in Thousands)
| FY 2023 Enacted | FY 2024 President's Budget | FY 2024 +/ - FY 2023 | |
| Total compensable workyears: | |||
| Full-time equivalent | 589 | 597 | 8 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $212 | $217 | $5 |
| Average GM/GS grade | 13.0 | 13.0 | 0.0 |
| Average GM/GS salary | $133 | $137 | $4 |
| Average salary, Commissioned Corps (42 U.S.C. 207) | $0 | $0 | $0 |
| Average salary of ungraded positions | $140 | $146 | $6 |
| OBJECT CLASSES | FY 2023 Enacted | FY 2024 President's Budget | FY 2024 +/ - FY 2023 |
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | $57,013 | $61,153 | $4,141 |
| 11.3 Other Than Full-Time Permanent | $27,618 | $29,124 | $1,506 |
| 11.5 Other Personnel Compensation | $3,206 | $3,380 | $175 |
| 11.7 Military Personnel | $0 | $0 | $0 |
| 11.8 Special Personnel Services Payments | $14,351 | $15,133 | $783 |
| 11.9 Subtotal Personnel Compensation | $102,187 | $108,791 | $6,605 |
| 12.1 Civilian Personnel Benefits | $33,251 | $35,461 | $2,211 |
| 12.2 Military Personnel Benefits | $0 | $0 | $0 |
| 13.0 Benefits to Former Personnel | $0 | $0 | $0 |
| Subtotal Pay Costs | $135,437 | $144,253 | $8,815 |
| 21.0 Travel & Transportation of Persons | $1,283 | $1,256 | -$27 |
| 22.0 Transportation of Things | $259 | $256 | -$3 |
| 23.1 Rental Payments to GSA | $0 | $0 | $0 |
| 23.2 Rental Payments to Others | $2 | $2 | $0 |
| 23.3 Communications, Utilities & Misc. Charges | $1,118 | $1,081 | -$37 |
| 24.0 Printing & Reproduction | $3 | $3 | $0 |
| 25.1 Consulting Services | $88,602 | $88,188 | -$415 |
| 25.2 Other Services | $52,422 | $50,060 | -$1,762 |
| 25.3 Purchase of Goods and Services from Government Accounts | $150,722 | $152,142 | $1,149 |
| 25.4 Operation & Maintenance of Facilities | $860 | $845 | -$14 |
| 25.5 R&D Contracts | $16,985 | $16,979 | -$6 |
| 25.6 Medical Care | $37 | $37 | $0 |
| 25.7 Operation & Maintenance of Equipment | $4,633 | $4,569 | -$64 |
| 25.8 Subsistence & Support of Persons | $0 | $0 | $0 |
| 25.0 Subtotal Other Contractual Services | $314,260 | $313,419 | -$841 |
| 26.0 Supplies & Materials | $5,250 | $5,207 | -$42 |
| 31.0 Equipment | $4,845 | $4,769 | -$76 |
| 32.0 Land and Structures | $1,476 | $1,469 | -$7 |
| 33.0 Investments & Loans | $0 | $0 | $0 |
| 41.0 Grants, Subsidies and Contributions | $1,877,705 | $2,069,925 | $192,220 |
| 42.0 Insurance Claims and Indemnities | $0 | $0 | $0 |
| 43.0 Interest & Dividends | $15 | $14 | -$1 |
| 44.0 Refunds | $0 | $0 | $0 |
| Subtotal Non-Pay Costs | $2,206,216 | $2,397,400 | $191,185 |
| Total Budget Authority by Object Class | $2,341,653 | $2,541,653 | $200,000 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2023 Enacted | FY 2024 President's Budget | FY 2024 +/ - FY 2023 |
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $57,013 | $61,153 | $4,141 |
| Other Than Full-Time Permanent (11.3) | $27,618 | $29,124 | $1,506 |
| Other Personnel Compensation (11.5) | $3,206 | $3,380 | $175 |
| Military Personnel (11.7) | $0 | $0 | $0 |
| Special Personnel Services Payments (11.8) | $14,351 | $15,133 | $783 |
| Subtotal Personnel Compensation (11.9) | $102,187 | $108,791 | $6,605 |
| Civilian Personnel Benefits (12.1) | $33,251 | $35,461 | $2,211 |
| Military Personnel Benefits (12.2) | $0 | $0 | $0 |
| Benefits to Former Personnel (13.0) | $0 | $0 | $0 |
| Subtotal Pay Costs | $135,437 | $144,253 | $8,815 |
| Travel & Transportation of Persons (21.0) | $1,283 | $1,256 | -$27 |
| Transportation of Things (22.0) | $259 | $256 | -$3 |
| Rental Payments to Others (23.2) | $2 | $2 | $0 |
| Communications, Utilities & Misc. Charges (23.3) | $1,118 | $1,081 | -$37 |
| Printing & Reproduction (24.0) | $3 | $3 | $0 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | $54,980 | $55,392 | $412 |
| Other Services (25.2) | $52,422 | $50,660 | -$1,762 |
| Purchase of Goods and Services from Government Accounts (25.3) | $89,263 | $89,030 | -$234 |
| Operation & Maintenance of Facilities (25.4) | $860 | $845 | -$14 |
| Operation & Maintenance of Equipment (25.7) | $4,663 | $4,569 | -$64 |
| Subsistence & Support of Persons (25.8) | $0 | $0 | $0 |
| Subtotal Other Contractual Services | $202,157 | $200,496 | -$1,662 |
| Supplies & Materials (26.0) | $5,250 | $5,207 | -$42 |
| Subtotal Non-Pay Costs | $210,072 | $208,301 | -$1,771 |
| Total Administrative Costs | $345,509 | $352,553 | $7,044 |
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2022 Final | FY 2023 Enacted | FY 2024 President's Budget | ||||||
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of Extramural Activities | |||||||||
| Direct: | 45 | - | 45 | 45 | - | 45 | 45 | - | 45 |
| Total: | 45 | - | 45 | 45 | - | 45 | 45 | - | 45 |
| Division of Translational Research | |||||||||
| Direct: | 31 | - | 31 | 31 | - | 31 | 34 | - | 34 |
| Total: | 31 | - | 31 | 31 | - | 31 | 34 | - | 34 |
| Office of the Director | |||||||||
| Direct: | 142 | - | 142 | 140 | - | 140 | 140 | - | 140 |
| Reimbursable: | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 |
| Total: | 152 | - | 152 | 150 | - | 150 | 150 | - | 150 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 30 | - | 30 | 30 | - | 30 | 33 | - | 33 |
| Total: | 30 | - | 30 | 30 | - | 30 | 33 | - | 33 |
| Division of AIDS Research | |||||||||
| Direct: | 17 | - | 17 | 17 | - | 17 | 17 | - | 17 |
| Total: | 17 | - | 17 | 17 | - | 17 | 17 | - | 17 |
| Division of Services and Intervention Research | |||||||||
| Direct: | 16 | - | 16 | 16 | - | 16 | 18 | - | 18 |
| Total: | 16 | - | 16 | 16 | - | 16 | 18 | - | 18 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 288 | - | 288 | 300 | - | 300 | 300 | - | 300 |
| Reimbursable: | - | - | - | - | - | - | - | - | - |
| Total: | 288 | - | 288 | 300 | - | 300 | 300 | - | 300 |
| Total | 579 | - | 579 | 589 | - | 589 | 597 | - | 597 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTE's supported by funds from Cooperative Research and Development Agreements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GS Grade |
| 2020 | 12.8 |
| 2021 | 12.9 |
| 2022 | 13.0 |
| 2023 | 13.0 |
| 2024 | 13.0 |
[Top]
Detail of Positions
| Grade | FY 2022 Final Final |
FY 2023 Enacted |
FY 2024 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | $203,700 | $212,103 | $216,928 |
| GM/GS-15 | 81 | 87 | 87 |
| GM/GS-14 | 81 | 87 | 91 |
| GM/GS-13 | 120 | 129 | 133 |
| GS-12 | 88 | 94 | 94 |
| GS-11 | 25 | 27 | 27 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 23 | 25 | 25 |
| GS-8 | 4 | 4 | 4 |
| GS-7 | 2 | 2 | 2 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 1 | 1 | 1 |
| GS-3 | 2 | 2 | 2 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 427 | 458 | 466 |
| Commissioned Corps (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 0 | 0 | 0 |
| Ungraded | 181 | 181 | 181 |
| Total permanent positions | 430 | 430 | 430 |
| Total positions, end of year | 609 | 640 | 648 |
| Total full-time equivalent (FTE) employment, end of year | 579 | 589 | 597 |
| Average ES salary | $203,700 | $212,103 | $216,928 |
| Average GM/GS grade | 13.0 | 13.0 | 13.0 |
| Average GM/GS salary | $128,298 | $132,662 | $136,581 |
| 1Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
References:
1 Substance Abuse and Mental Health Services Administration. (2021). Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health (HHS Publication No. PEP21-07-01-003, NSDUH Series H-56).. Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from www.samhsa.gov/data/report/2020-nsduh-annual-national-report
2 Institute of Health Metrics and Evaluation. ghdx.healthdata.org/gbd-results-tool accessed October 2022.
3 Centers for Disease Control and Prevention. (2022). Web-based Injury Statistics Query and Reporting System (WISQARS). Atlanta, GA: National Centers for Injury Prevention and Control, Centers for Disease Control and Prevention. Retrieved from www.cdc.gov/injury/wisqars/index.html
4 https://www.whitehouse.gov/briefing-room/statements-releases/2023/02/07/fact-sheet-in-state-of-the-union-president-biden-to-outline-vision-to-advance-progress-on-unity-agenda-in-year-ahead/
5 https://www.whitehouse.gov/wp-content/uploads/2023/02/White-House-Report-on-Mental-Health-Research-Priorities.pdf
6 www.nimh.nih.gov/about/strategic-planning-reports
7 www.nimh.nih.gov/about/organization/od/odwd/nimhs-approach-to-mental-health-disparities-research
8 www.nih.gov/climateandhealth
9 www.nimh.nih.gov/about/strategic-planning-reports/2021-strategic-plan-progress-report
10 www.nimh.nih.gov/research/research-funded-by-nimh/research-initiatives/practice-based-suicide-prevention-research-centers
11 reporter.nih.gov/project-details/10294750
12 reporter.nih.gov/project-details/10435003
13 reporter.nih.gov/project-details/10436043
14reporter.nih.gov/project-details/10441870
15 grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-125.html
16 Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health, Report to Congress on Addressing Youth Mental Health Disparities (September 2021).
17 Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health, Report to Congress on Addressing Youth Mental Health Disparities: Post Conference Report (October 2022).
18 www.nimh.nih.gov/about/strategic-planning-reports
19 www.nimhd.nih.gov/about/strategic-plan/
20www.nimh.nih.gov/news/research-highlights/2022/multistage-autism-screening-in-early-intervention-settings-may-reduce-disparities
21 www.nimh.nih.gov/research/research-funded-by-nimh/research-initiatives/advanced-laboratories-for-accelerating-the-reach-and-impact-of-treatments-for-youth-and-adults-with-mental-illness-alacrity
22 www.nimh.nih.gov/about/organization/cgmhr
23 www.nimh.nih.gov/about/director/messages/2022/research-along-the-autism-spectrum-diverse-research-to-meet-diverse-needs
24 reporter.nih.gov/search/M0V2yQ80P06NrX4dWzsC_w/project-details/10285267
25 reporter.nih.gov/search/yUfCjJsTOUOqvb0tflFSJw/project-details/10063050
26 www.nimh.nih.gov/news/research-highlights/2022/personalizing-deep-brain-stimulation-for-treatment-resistant-depression
27 www.nimh.nih.gov/news/research-highlights/2022/new-approach-allows-magnetic-brain-stimulation-to-target-deep-brain-structures
28 grants.nih.gov/grants/guide/pa-files/PAR-22-169.html
30 jamanetwork.com/journals/jamanetworkopen/fullarticle/2791033
31 grants.nih.gov/grants/guide/pa-files/PAR-22-112.html
32 www.nimh.nih.gov/news/science-news/2021/researchers-use-exosome-based-strategy-to-block-hiv-in-mice
33 www.nimh.nih.gov/news/research-highlights/2021/genomic-data-from-more-than-41000-people-shed-new-light-on-bipolar-disorder
34 www.nimh.nih.gov/funding/sbir
35 nimh.nih.gov/about/director/messages/2022/bringing-innovation-to-the-search-for-biomarkers
36 reporter.nih.gov/search/ePHCQuWIIEqh4I9Kq6Wj7w/project-details/9680324
37 www.nimh.nih.gov/about/director/messages/2022/bringing-innovation-to-the-search-for-biomarkers
38 grants.nih.gov/grants/guide/notice-files/NOT-MH-22-090.htm l
39 grants.nih.gov/grants/guide/rfa-files/RFA-MH-22-140.html
40 theactionalliance.org/sites/default/files/ring_the_alarm-_the_crisis_of_black_youth_suicide_in_america_copy.pdf
41 theactionalliance.org/news/national-action-alliance-suicide-prevention-announces-goal-reduce-suicide-20-percent-2025
42 grants.nih.gov/grants/guide/notice-files/NOT-MH-22-175.html
43 hhs.gov/sites/default/files/surgeon-general-youth-mental-health-advisory.pdf
44 www.nimh.nih.gov/funding/grant-writing-and-application-process/concept-clearances/2022/understanding-social-media-and-youth-mental-health
46 reporter.nih.gov/project-details/10509346
47www.cdc.gov/nchs/data/hestat/suicide/rates_1999_2017.htm
48 reporter.nih.gov/project-details/10440864
49 www.nimh.nih.gov/news/science-news/2021/adaptive-screener-may-help-identify-youth-at-risk-of-suicide
50 nih.gov/news-events/news-releases/nih-public-private-partnership-advance-early-interventions-schizophrenia
51 pubmed.ncbi.nlm.nih.gov/33667856/
52pubmed.ncbi.nlm.nih.gov/29971330/
53 ncbi.nlm.nih.gov/pmc/articles/PMC5048498/
54reporter.nih.gov/search/QtpvyVCzBkyTL5sHY0n5Fw/project-details/10019595
55pubmed.ncbi.nlm.nih.gov/30710497/
56 pubmed.ncbi.nlm.nih.gov/30389840/
57 grants.nih.gov/grants/guide/pa-files/PAR-19-344.html
58 www.nimh.nih.gov/research/research-funded-by-nimh/research-initiatives/advanced-laboratories-for-accelerating-the-reach-and-impact-of-treatments-for-youth-and-adults-with-mental-illness-alacrity
59 grants.nih.gov/grants/guide/pa-files/PAR-20-293.htm l
60grants.nih.gov/grants/guide/rfa-files/rfa-mh-19-150.html
61 grants.nih.gov/grants/guide/rfa-files/RFA-MH-20-205.html
62 grants.nih.gov/grants/guide/rfa-files/RFA-MH-19-151.html
63grants.nih.gov/grants/guide/pa-files/PAR-20-286.html
64www.nimh.nih.gov/research/research-funded-by-nimh/research-initiatives/practice-based-suicide-prevention-research-centers
65 oar.nih.gov/hiv-policy-and-research/strategic-plan
66 www.hiv.gov/blog/hhs-and-the-national-hivaids-strategy
67 pubmed.ncbi.nlm.nih.gov/34974114/
68 pubmed.ncbi.nlm.nih.gov/36044550/
69pubmed.ncbi.nlm.nih.gov/36008415/
70 clinicaltrials.gov/ct2/show/NCT02543983
71 www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials
72 pubmed.ncbi.nlm.nih.gov/35618222/
73www.nimh.nih.gov/get-involved/digital-shareables/shareable-resources-on-suicide-prevention
75www.nimh.nih.gov/news/events/announcements/facebook-live-the-intersection-of-suicide-and-substance-use
