New Gene Delivery Method Paves the Way for Advanced Brain Therapies
• Research Highlight
A new study, funded by the National Institute of Mental Health and the National Institute of Neurological Disorders and Stroke, describes a promising way to carry genetic material into the brain to reach cellular targets. The researchers developed a delivery vehicle that can effectively transport genes across the blood-brain barrier by latching onto a human protein and distributing its genetic cargo to cells in the brain. Although the researchers have not yet tested the approach in people, this study brings us closer to making many life-saving treatments a reality.
What is the treatment?
Gene therapies use genes to treat, prevent, or cure diseases and disorders. Small viruses called adeno-associated viruses (AAVs) are a main way of delivering gene therapies throughout the body, including the brain. AAVs have tremendous potential to expand gene therapies by safely delivering genetic material to cells and tissues to treat disorders at their root genetic cause.
However, a difficulty in developing AAV therapies has been the need to deliver genes to specific cells and organs; otherwise, they may cause unwanted effects elsewhere in the body. While researchers have identified the genes underlying many brain disorders, a strict gatekeeper known as the blood-brain barrier has presented an obstacle to effective treatment. The barrier protects us from toxins and other harmful things by filtering what comes in and goes out of the human brain. However, this barrier can sometimes work too well, keeping out gene therapies that could help treat or cure diseases.
Unfortunately, many existing AAVs can’t efficiently cross the blood-brain barrier. Although some AAVs successfully crossed the barrier in animal studies, few have shown success when tested in humans. These challenges have stalled the development of treatments for many disorders, driving researchers to look for more effective ways of delivering gene therapies.
A team of researchers at the Broad Institute of MIT and Harvard University, led by Benjamin Deverman, Ph.D. , set out to engineer an AAV that could effectively cross the blood-brain barrier to deliver genes into the human brain. The study had funding through The Brain Research Through Advancing Innovative Neurotechnologies® Initiative, or The BRAIN Initiative® , and the NIH Common Fund’s Somatic Cell Genome Editing program .
What did researchers do in the study?
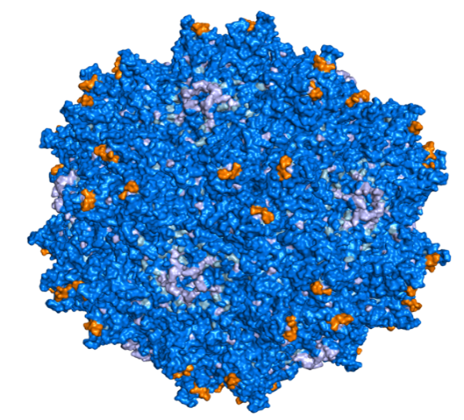
The researchers started by looking for an AAV with a high chance of reaching the human brain. In previous work, Deverman’s lab had already developed an efficient way of engineering new AAVs by looking for ones that bind to specific proteins on the surface of target cells or organs.
They used that method to create and screen a library of different AAVs to see if any would bind to a protein called human transferrin receptor (TfR1), which brings iron into the brain. TfR1 is highly expressed on the human blood-brain barrier and has been shown to shuttle large molecules across that barrier to reach the brain in studies with humans.
This step narrowed down the candidate AAVs to one, named BI-hTFR1, that could attach itself to the TfR1 protein. With a promising AAV identified, the researchers next tested the AAV in human cells and in mice modified to express the human form of the TfR1 protein. They also examined whether the new AAV could transport genetic material into the brain, comparing it with one of the few currently existing AAVs able to deliver genes to the human central nervous system.
What were the study results?
First, the researchers found that the TfR1-bound AAV successfully crossed the blood-brain barrier in the human cell model. Moreover, in a head-to-head comparison with the existing AAV used in nervous system gene therapies, significantly more of the new AAV actively traveled across the brain cell barrier.
This finding was further supported when the researchers injected the AAV into the bloodstream of mice expressing the human form of TfR1. Results showed that the new AAV successfully entered the brain and spinal cord of the mice and did so at much higher levels than the existing AAV, showing 6–12 times greater amounts across the brain. Importantly, this effect was not found for other organs, demonstrating the new AAV’s enhanced entry into the central nervous system. The AAV also affected brain cells with critical functions, reaching up to 92% of astrocytes and 71% of neurons , which play important roles in how cells develop and communicate.
Last, the researchers examined the AAV’s ability to deliver the human gene GBA1 into the mouse brain. Mutations in the GBA1 gene are linked to several neurodegenerative disorders, including Gaucher disease and Parkinson’s disease. The new AAV delivered the GBA1 gene throughout the brain. Once again, the results emphasized the enhanced effectiveness of the new AAV, which delivered 30 times more copies of GBA1 compared to the existing AAV. Together, the results showed that the AAV can effectively enter the brain at a large scale and carry with it healthy copies of genetic material.
What do the results mean?
These findings confirm that AAVs can be targeted to specific proteins to create powerful, minimally invasive gene delivery vehicles. The researchers in this study engineered an AAV that, by directly binding to a human receptor protein, crossed the blood-brain barrier to reach critical cells and deliver a disease-relevant gene throughout the brain.
Importantly, the new AAV was more effective and efficient than the main AAV currently used for nervous system gene therapies. Another critical advantage was its human-specific binding. Because the AAV binds to a well-studied human protein found at the blood-brain barrier, the researchers think it has strong potential to work for human gene therapies. Using mice that express the human form of the Tfr1 receptor also provides strong evidence that this therapy could show success in people.
Although exciting, the results require further testing in human studies. The researchers will also need to address common challenges that face any AAV gene therapy, including limits on the size of the gene it can deliver, potential off-target impacts on other genes or gene pathways, and the risk of an overactive immune system response. Despite these hurdles, with further testing and development, the gene delivery method could open up new therapeutic avenues and revolutionize treatment for a range of neurological and mental disorders.
Reference
Huang, Q., Chan, K. Y., Lou, S., Keyes, C., Wu, J., Botticello-Romero, N. R., Zheng, Q., Johnston, J., Mills, A., Brauer, P. P., Clouse, G., Pacouret, S., Harvey, J. W., Beddow, T., Hurley, J. K., Tobey, I. G., Powell, M., Chen, A. T., Barry, A. J., Eid, F.-E., Chan, Y. A., & Deverman, B. E. (2024). An AAV capsid reprogrammed to bind human transferrin receptor mediates brain-wide gene delivery. Science, 384(6701), 1220–1227. https://www.doi.org/10.1126/science.adm8386
Grants
Brain Research Through Advancing Innovative Neurotechnologies® Initiative and The BRAIN Initiative® are registered trademarks of the U.S. Department of Health and Human Services.
