FY 2023 Budget - Congressional Justification
National Institute of Mental Health
CONGRESSIONAL JUSTIFICATION FY 2023
National Institutes of Health
Department of Health and Human Services
- Director’s Overview
- IC Fact Sheet
- Major Changes in Budget Request
- Budget Mechanism Table
- Appropriations Language
- Summary of Changes
- Budget Graphs
- Organization Chart
- Budget Authority by Activity
- Justification of Budget Request
- Appropriations History
- Authorizing Legislation
- Amounts Available for Obligation
- Budget Authority by Object Class
- Salaries and Expenses
- Detail of Full-Time Equivalent Employment (FTE)
- Detail of Positions
Director’s Overview

M.D., Ph.D.,
Director of NIMH
The National Institute of Mental Health (NIMH) is the lead federal agency for research on mental illnesses, with a mission to transform the understanding and treatment of mental illnesses through basic and clinical research, paving the way for prevention, recovery, and cure.
In the United States, an estimated 51.5 million adults suffer from a mental illness, which may be significantly impairing and life-threatening.1 Mental illnesses are the fifth leading cause of disability in the United States, accounting for 6.6 percent of all disability-adjusted life years in 2019.2 One of the most tragic outcomes of untreated mental illness is suicide. Suicide accounted for the loss of over 47,500 American lives in 2019 alone; it is the second leading cause of death in youth and young adults aged 10-34, and the tenth leading cause of death overall.3
NIMH supports a diverse portfolio of basic, translational, and clinical research, with the potential to improve clinical care over the short, medium, and long-term. NIMH is also expanding investment in global mental health research through the NIMH Center for Global Mental Health Research (CGMHR). CGMHR supports mental health research in low-resource settings worldwide in order to accelerate and enrich scientific advancements while helping to reduce mental health disparities globally and domestically. In the summer of 2021, NIMH published an annual update to its Strategic Plan for Research,4 which continues to emphasize investments in the research workforce and research on mental health disparities, while also highlighting new efforts, such as the Accelerating Medicines Partnership® in Schizophrenia (AMP® SCZ) and research on the mental health impacts of COVID-19. NIMH also developed a companion Progress Report,5 which highlights significant accomplishments made during FY 2020 toward achieving the goals described in the Strategic Plan. Updating the plan on an annual basis enables NIMH to adapt to new challenges and needs as they arise in order to maintain the relevance, timeliness, and real-world impact of the research that NIMH supports.
Responding to Emerging Mental Health Needs
Rapid-Acting Interventions for Severe Suicide Risk. Despite advances in the treatment of depression and other serious mental illnesses, there remain few evidence-based interventions that rapidly reduce suicide risk within health care settings. NIMH is supporting eight new research projects that focus on testing the safety, efficacy, and feasibility of several of the newest antidepressant interventions – intravenous ketamine and intranasal esketamine (medications known to rapidly reduce depressive symptoms in hours or days)6 as well as transcranial magnetic stimulation (TMS; a noninvasive treatment which uses magnets to activate specific parts of the brain) – to rapidly reduce suicidal thoughts and behaviors in adults and adolescents.7 For example, NIMH-funded researchers are investigating whether cognitive behavioral therapy can extend the effects of intranasal esketamine in reducing suicidality in people with major depressive disorder who are hospitalized for suicidal thoughts or a suicide attempt.8 Identifying and developing rapid-acting treatments may help “jumpstart” recovery and could reduce the likelihood of repeated hospitalizations and self-harming thoughts and behaviors.
Understanding and Mitigating the Mental Health Impacts of COVID-19.
The COVID-19 pandemic is an enormous source of stress and anxiety for many, both from the loss of loved ones and from the loss of economic, food, and housing security. Research to understand and mitigate the impacts of the pandemic on mental health remain a high priority for NIMH. For example, as part of a larger study on temperament and socioemotional development, researchers in the NIMH Intramural Research Program (IRP) examined data from individuals who had been followed from toddlerhood to young adulthood, and they were able to identify early risk factors that predicted heightened anxiety in young adults during the pandemic.9 NIMH has also been involved in several NIH-wide efforts, including the Social, Behavioral, and Economic Impacts of COVID-19 Working Group, which supports research focused on the secondary effects of the pandemic, such as financial hardship, reduced access to health care, and school closures.10 In addition, NIMH continues to engage directly with the public to help mitigate the mental health impacts of the pandemic by providing numerous messages and shareable resources on coping with trauma in general and the COVID-19 pandemic in particular.11,12 Through these research and outreach efforts, NIMH aims to support mental health during this pandemic, and also to prepare for future public health emergencies.
Addressing Mental Health Disparities
Individuals from racial, ethnic, sexual, and gender minority groups, socioeconomically disadvantaged populations, and underserved rural populations experience striking mental health disparities in burden of illness, access and engagement in care, and recovery. To make progress towards the Institute’s vision of a world in which mental illnesses are prevented and cured, health disparities must be addressed. NIMH issued two requests for information (RFIs) on innovative research strategies and priorities to improve mental health outcomes and reduce or eliminate mental health disparities in affected populations. Stakeholders were asked to provide input on a number of topics, including novel engagement strategies and culturally and linguistically appropriate service delivery approaches,13as well as approaches tailored to underserved rural populations.14 An essential element in promoting equity is to build a valid evidence base to ensure effective treatment and care. This requires an inclusive environment where populations with health disparities are represented in basic, translational, effectiveness, and services research studies. Furthermore, a diverse biomedical research workforce is needed to advance scientific progress and capitalize on innovative ideas and distinct perspectives that have the potential to improve health disparities research. In efforts to dismantle structural racism in policies and practices, the Institute is examining the composition of its applicant and awardee pools.15 Additionally, the NIMH Extramural Review Branch is working to develop strategies that enhance the diversity of perspectives among reviewers, and plans to join the NIH Center for Scientific Review’s ongoing efforts to identify and eliminate any potential systemic biases that could lead to disparities in grant application scores. NIMH also continues to expand training, mentoring, and career advancement opportunities for basic, translational, and clinical researchers across a range of career stages and from diverse backgrounds who can provide broad and unique perspectives to pressing research questions.
Expanding Access to Resources for Early Psychosis Treatment and Research
Psychosis encompasses a group of conditions that affect the brain and involve some loss of contact with reality. Each year, about 100,000 youth and young adults in the United States experience a first episode of psychosis (or early psychosis).16 Left untreated, early psychotic symptoms can disrupt school, work, and social relations, as well as lead to greater risk of additional problems such as developing a substance use disorder, having legal trouble, or becoming homeless.
However, effective early interventions, such as coordinated specialty care (CSC), are available. CSC promotes shared decision-making and leverages a team of specialists to work with individuals on personal treatment plans.17 NIMH-funded researchers established the effectiveness of CSC for early psychosis, with better clinical and functional outcomes for multi- disciplinary, person-centered treatment compared to usual care.18 In recent years, CSC programs have been established and expanded across the United States. To build on this momentum, the NIMH-supported Early Psychosis Intervention Network (EPINET)19 is a research initiative aimed at enhancing effective CSC delivery to people with symptoms of early psychosis, and promoting new research to improve diagnosis, interventions, and outcomes in early serious mental illness. EPINET continues to grow. Its national network of research hubs now includes 17 states with 101 clinics that provide CSC, and a national data coordinating center that supports and integrates the work of these hubs and clinics.20 EPINET has also launched a new web portal, a key feature of which is the EPINET Core Assessment Battery that clinicians can use to assesses key domains of early psychosis, recovery, and treatment.21 EPINET’s coordinated effort may accelerate advances in early psychosis care, recovery outcomes, and scientific discovery in real-world, community-based settings.
Translating Technologies into Mental Health Therapeutics
The Accelerating Medicines Partnership® Schizophrenia (AMP® SCZ) program. Schizophrenia is a serious mental illness that is associated with significant health, social, and economic concerns. Schizophrenia is one of the 15 leading causes of disability worldwide and individuals with the disorder are at increased risk of premature death relative to the general population.22 Detection and intervention before psychosis develops, when individuals are at clinical high risk for psychosis, could postpone or even prevent the transition to psychosis and improve individuals’ clinical and functional outcomes. To support efforts in developing early-stage interventions for patients who are at risk of developing schizophrenia, NIMH launched the Accelerating Medicines Partnership® Schizophrenia (AMP® SCZ) program in collaboration with the Foundation for the National Institutes of Health, the U.S. Food and Drug Administration, and multiple public and private partners.23,24 NIMH is currently supporting three research projects as part of the AMP® SCZ program. The Trajectories and Predictors in the Clinical High Risk for Psychosis Population: Prediction Scientific Global Consortium (PRESCIENT) grant and the Psychosis-Risk Outcomes Network (ProNET) grant will support the development of a 42-site, international research network.25,26 The Psychosis Risk Evaluation, Data Integration, and Computational Technologies (PREDICT): Data Processing, Analysis, and Coordination Center will serve as a coordinating hub for data aggregation, analysis, and sharing via the NIMH Data Archive.27 Researchers will assess individuals at clinical high risk for psychosis over a period of two years using measures of symptoms, brain structure and function, genomics, blood-based markers, cognition, speech samples, and data collection from digital devices. The overall aims of AMP® SCZ are to develop tools to predict individual outcomes, including the identification of biomarkers; to establish a global research network with an accessible data repository; and to help researchers design better clinical trials that may lead to early-stage interventions for individuals who are at risk of developing schizophrenia.
Using Mobile Technology to Improve Care for Teens with Depression
Mobile technology platforms have enormous potential to substantially improve and expand access to mental health services. In a project funded by the NIMH Small Business Technology Transfer program, researchers are investigating whether smartphone technology can be used to develop a passive monitoring system that can predict teens’ depressive symptoms and report to their parents and care team, thereby improving the availability and quality of care.28 By making symptom monitoring a part of routine medical care, the goal is that these new technologies will help improve teens’ depressive symptoms and overall functioning, decrease their need for acute and crisis services, and stem the demand for more intensive mental health services.
Early Detection and Personalized Interventions for Individuals with Autism
Because early treatment is so critical for children with autism spectrum disorder (ASD), efforts have been made to try to reduce the age of diagnosis by universally screening all children for signs of ASD. As part of these efforts, NIMH is partnering with other NIH Institutes to support seven research projects aimed at developing and validating screening tools to detect signs of ASD before 12 months of age.29 NIMH also supports research to improve the treatment of autism through the Autism Biomarkers Consortium for Clinical Trials (ABC-CT).30 This multisite study has enrolled children ages 6 to 11 with and without ASD, with the goal of developing biomarkers – specifically, patterns of brain activity or eye movement – that could be used to separate individuals with ASD into distinct subgroups for clinical trials, ultimately leading to more predictive and personalized treatment.31
Adaptive Screener May Help Identify Youth at Risk of Suicide
Suicide rates for youth have risen over the past 2 decades in the United States: in 2019, approximately 6,488 youth ages 10 to 24 died by suicide.32 Improved suicide risk detection through effective screening in health care settings is a key strategy to save lives. NIMH-supported researchers developed the Computerized Adaptive Screen for Suicidal Youth (CASSY) to increase suicide risk screening efficiency and precision among youth admitted to emergency departments for any reason.33 The tablet-administered CASSY relies on computerized adaptive testing technology, which uses an iterative algorithm to tailor the sequence of approximately 11 screening questions based on previous responses from the individual being screened. CASSY correctly identified 82.4 percent of youth who went on to attempt suicide in the three months following screening. The results suggest that CASSY is a valuable tool for identifying at-risk youth and may help emergency personnel link individuals to mental health and suicide prevention services. Moving forward, it will be important for researchers to collaborate with emergency personnel to identify optimal screening implementation strategies, particularly in low-resource settings.
Accelerating the Basic Understanding of Mental Illnesses
From Brain Mechanisms to Novel Therapies: Understanding and Treating Eating Disorders. Millions of Americans suffer from eating disorders, serious illnesses that cause severe disturbances in a person’s eating behaviors and sometimes death.34 NIMH continues to support research aimed at improving the understanding of eating disorders, developing new treatments, and improving the efficacy and availability of existing treatments.35 In a series of NIMH-funded studies, investigators have discovered differences in the reward signaling circuitry of the brain among individuals with anorexia nervosa compared to healthy control subjects.36,37 These differences could explain how maladaptive food avoidance behaviors arise in individuals diagnosed with anorexia nervosa, informing efforts to develop new treatments to prevent or reverse maladaptive food choice behaviors.38,39 Other NIMH-supported researchers are focused on improving existing interventions – for example, by leveraging digital technology to connect individuals with eating disorders to mental health services and support networks in real time,40,41 and by modifying cognitive behavioral therapy to more specifically target binge-eating disorder.42 Additionally, NIMH supports a large-scale genomics research project across three different eating disorder diagnoses, with the goal of better understanding the basic mechanisms – both shared and unique – underlying risk, outcomes, and connection to metabolic factors.43
NIH Brain Research through Advancing Innovative Neurotechnologies® (BRAIN) Initiative Cell Census Network (BICCN)
The human brain, with its nearly 100 billion neurons and nearly 100 trillion connections, is arguably the most complex object in the known universe.44 A critical step toward unraveling this complexity is to catalogue how many and what types of cells make up the brain. Focused on exactly this challenge, the BICCN is a collaboration of over 250 NIH- supported scientists at nearly 50 institutions across three continents.45 Recently the BICCN began publishing data derived from genetic analysis of 450,000 cells from the motor cortex of mice, monkeys, and humans.46 The data collected through this effort are available to all scientists through the BICCN Data Inventory.47 Already these data are enabling significant advances in our understanding of the locations and functions of the cell types, the differences and similarities among species, and the accuracy of the technologies used to acquire the data.48
Understanding Abnormal Neural Function in a Rare Genetic Disorder
Major advances in genetics research have accelerated progress toward understanding the genetic determinants of mental illnesses. For example, NIMH-supported researchers are studying tissue donated by people with 22q11.2 deletion syndrome (a genetic disorder caused by the deletion of a piece of genetic material at location q11.2 on chromosome 22) in an effort to better manage the psychiatric effects associated with this rare genetic condition, which include significantly elevated risks for ASD and psychosis.49 The researchers recently discovered how 22q11.2 deletion syndrome impacts the brain at the level of individual neurons, and demonstrated that the abnormalities in 22q11.2 deletion syndrome neurons could be partially restored by re-introducing one of the deleted genes. This progress in understanding neuronal development could help to identify new therapeutic approaches for 22q11.2 deletion syndrome, and is emblematic of NIMH’s larger goal to uncover the exact mechanisms linking genes to mental illnesses.
Research Domain Criteria (RDoC) at 10 Years
Traditionally, mental illnesses have been conceptualized as disorders that are diagnosed based on the number and type of symptoms, and the presence of distress or impairment. This approach presents several obstacles to understanding the development and treatment of mental illnesses – for example, the problem of heterogeneity, when two people are diagnosed with the same illness despite having few symptoms in common. Recognizing these obstacles, in 2010 NIMH launched the RDoC initiative: a flexible research framework focused on understanding the basic biological, emotional, and cognitive processes that lead to mental health and illness, unconstrained by traditional diagnostic categories.50 In its first 10 years, the RDoC transdiagnostic, dimensional approach has changed the conversation in mental health research, accelerating discovery of the neurobiology underlying mental illnesses, and highlighting the need for precision-medicine approaches.51 In the next 10 years, NIMH aims to build on this momentum by developing new tools and larger datasets with which to test and refine the RDoC framework, ultimately paving the way to precision psychiatry.52
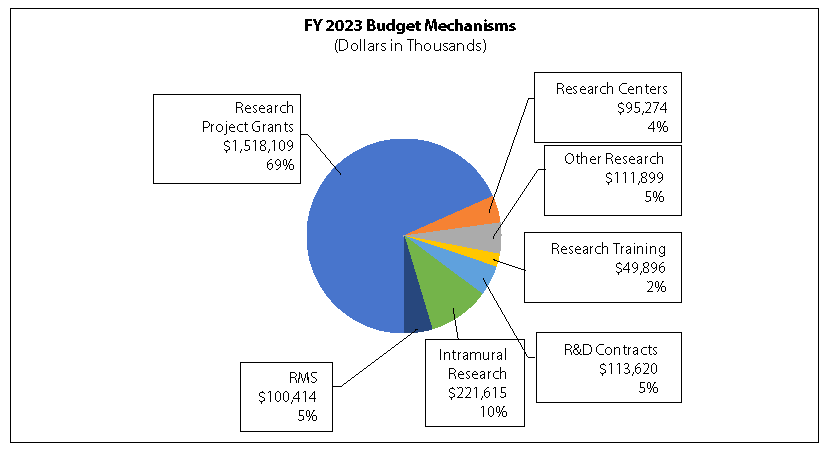
Major Changes in the Budget
Major changes by budget mechanism and/or budget activity detail are briefly described below. Note that there may be overlap between budget mechanism and activity details and these highlights will not sum to the total change for the FY 2023 President’s Budget request for NIMH. The FY 2023 President’s Budget request is $2,210.8 million, an increase of $107.1 million compared to the FY 2022 Continuing Resolution level. The request includes $225.0 million provided through the 21st Century Cures Act.
Research Project Grants (+$80.6 million; total $1,518.1 million)
NIMH expects to increase funding for non-competing Research Grants by $12.5 million to fund projects receiving competing awards in prior years. Competing Research Project Grants are expected to increase by 31 grants or $64.5 million. This increase is distributed across all programmatic areas and basic, translational, or clinical research.
Research Centers (+$8.7 million; total $95.3 million)
NIMH expects to increase funding for Research Centers by $8.7 million to support additional ALACRITY Centers and Practice Based Suicide Prevention Research Centers.
Research and Development Contracts (+$7.4 million; total $113.6 million)
NIMH expects to increase funding for Research and Development Contracts and will continue to support trans-NIH initiatives, including cybersecurity efforts, as well as continued implementation of the NIMH Strategic Plan.
Intramural Research Programs (+$6.3 million; total $221.6 million)
NIMH expects to increase funding for Intramural Research by $6.3 million, and will continue to fund innovative research studies conducted by the Institute’s intramural scientists.
Research Management and Support (+$2.8 million; total $100.4 million)
NIMH expects to increase funding for Research Management and Support by $2.8 million and will continue to support the oversight and management of scientific programs critical to fulfilling the Institute’s mission.
Budget Mechanism - Total
| Mechanism | FY 2021 Final3 | FY 2022 | FY 2023 Presidents Budget | FY 2023 +/- FY 2022 | ||||
|---|---|---|---|---|---|---|---|---|
| No. | Amount | No. | Amount | No. | Amount | No. | Amount | |
| Research Projects: | ||||||||
| Noncompeting | 1,537 | $946,786 | 1,647 | $933,238 | 1,578 | $945,689 | -69 | $12,452 |
| Administrative Supplements | (103) | $16,862 | (125) | $19,956 | (125) | $19,956 | (0) | $0 |
| Competing: | ||||||||
| Renewal | 44 | $26,223 | 39 | $25,994 | 39 | $20,306 | 0 | -$5,687 |
| New | 602 | $396,762 | 547 | $393,629 | 578 | $463,912 | 31 | $70,283 |
| Supplements | 1 | $277 | 1 | $275 | 1 | $215 | 0 | -$60 |
| Subtotal Competing | 647 | $423,262 | 587 | $419,898 | 618 | $484,433 | 31 | $64,536 |
| Subtotal RPGs | 2,184 | $1,386,910 | 2,234 | $1,373,091 | 2,196 | $1,450,078 | -38 | $76,988 |
| SBIR/STTR | 89 | $64,718 | 89 | $64,422 | 95 | $68,031 | 6 | $3,608 |
| Research Project Grants | 2,273 | $1,451,628 | 2,323 | $1,437,513 | 2,291 | $1,518,109 | -32 | $80,596 |
| Research Centers | ||||||||
| Specialized/Comprehensive | 39 | $75,261 | 39 | $86,213 | 43 | $94,928 | 4 | $8,715 |
| Clinical Research | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Biotechnology | 0 | $50 | 0 | $50 | 0 | $50 | 0 | $0 |
| Comparative Medicine | 0 | $296 | 0 | $296 | 0 | $296 | 0 | $0 |
| Research Centers in Minority Institutions | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Research Centers | 39 | $75,607 | 39 | $86,559 | 43 | $95,274 | 4 | $8,715 |
| Other Research | ||||||||
| Research Careers | 366 | $63,429 | 370 | $64,112 | 376 | $65,103 | 6 | $992 |
| Cancer Education | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Cooperative Clinical research | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Biomedical Research Support | 10 | $4,816 | 0 | $0 | 0 | $0 | 0 | $0 |
| Minority Biomedical Research Support | 0 | $0 | 0 | $0 | 0 | $0 | 0 | $0 |
| Other | 59 | $49,447 | 59 | $47,496 | 53 | $46,796 | -6 | -$700 |
| Other Research | 435 | $117,693 | 429 | $111,608 | 429 | $111,899 | 0 | $292 |
| Total Research Grants | 2,747 | $1,644,927 | 2,791 | $1,635,680 | 2,763 | $1,725,282 | -28 | $89,603 |
| Ruth L. Kirschstein Training Awards | FTTPs | FTTPs | FTTPs | FTTPs | ||||
| Individual Awards | 267 | $12,533 | 278 | $13,528 | 277 | $13,785 | -1 | $257 |
| Institutional Awards | 501 | $27,782 | 503 | $35,438 | 502 | $36,111 | -1 | $673 |
| Total Research Training | 768 | $40,315 | 781 | $48,966 | 779 | $49,896 | -2 | $930 |
| Research and Develop Contracts | 133 | $104,949 | 136 | $106,187 | 141 | $113,620 | 5 | $7,433 |
| (SBIR/STTR)(non-add) | (0) | (($749) | (0) | (($763) | (0) | ($793) | (0) | ($30) |
| Intramural Research | 289 | $212,800 | 300 | $215,301 | 300 | $221,615 | 0 | $6,315 |
| Res. Management and Support | 278 | $96,746 | 289 | $97,575 | 289 | $100,414 | 0 | $2,839 |
| (SBIR Admin) (non-add) | (0) | ($0) | (0) | ($135) | (0) | ($135) | (0) | ($0) |
| Construction | $0 | $0 | $0 | $0 | ||||
| Buildings and Facilities | $0 | $0 | $0 | $0 | ||||
| Total NIMH | 567 | $2,099,736 | 589 | $2,103,708 | 589 | $2,210,828 | 0 | $107,120 |
1 All items in italics and brackets are non-add entries
2 Of which $50.0 million in FY 2021, $50.0 million in FY 2022, and $225.0 million in FY 2023 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
3 Includes 21st Century Cures Act funding not obligated in FY 2021 and carried into FY 2022.
Appropriations Language
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
For carrying out section 301 and title IV of the PHS Act with respect to mental health, $1,985,828,000.
NIH INNOVATION ACCOUNT, CURES ACT
(INCLUDING TRANSFER OF FUNDS)
For necessary expenses to carry our the purposes described in section 1001(b)(4) of the 21st Century Cures Act, in addition to amounts available for such purposes in the appropriations provided to the NIH in this Act, $1,085,000,000, to remain available until expended: Provided, That such amounts are appropriated pursuant to section 1001(b)(3) of such Act, are to be derived from amounts transferred under section 1001(b)(2)(A) of such Act, and my be transferred by the Director of the National Institutes of Health to other accounts of the National Institutes of Health solely for the purposes provided in such Act: Provided further, That upon a determination by the Direct that funds transferred pursuant to the previous proviso are not necessary for the purposes provided, such amounts may be transferred back to the Account: Provided further, That the transfer authority provided under this heading is in addition to any other transfer authority provided by law.
[Top]
Summary of Changes
(Dollars in Thousands)
| FY 2022 CR | $2,103,708 |
|---|---|
| FY 2023 Presidents Budget | $2,210,828 |
| Net Change | $107,120 |
| CHANGES | FY 2022 CR | FY 2023 President's Budget | Built in change from FY 2022 CR | |||
|---|---|---|---|---|---|---|
| FTE's | Budget Authority | FTE's | Budget Authority | FTE's | Budget Authority | |
| A. Built-in: | ||||||
| 1. Intramural Research: | ||||||
| a. Annualization of January 2021 pay increase & benefits | $75,083 | $80,145 | $498 | |||
| b. January FY 2022 pay increase & benefits | $75,083 | $80,145 | $2,542 | |||
| c. Paid days adjustment | $75,083 | $80,145 | -$285 | |||
| d. Differences attributable to change in FTE | $75,083 | $80,145 | $0 | |||
| e. Payment for centrally furnished services | $41,816 | $42,652 | $836 | |||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs |
$98,402 | $98,818 | $1,423 | |||
| Subtotal | $5,014 | |||||
| 2. Research Management and Support: | ||||||
| a. Annualization of January 2021 pay increase & benefit | $51,725 | $52,821 | $342 | |||
| b. January FY 2022 pay increase & benefits | $51,725 | $52,821 | $1,748 | |||
| c. Paid days adjustment | $51,725 | $52,821 | -$197 | |||
| d. Differences attributable to change in FTE | $51,725 | $52,821 | $0 | |||
| e. Payment for centrally furnished services | $9,07 | $9,257 | $182 | |||
| f. Cost of laboratory supplies, materials, other expenses, and non-recurring costs |
$36,775 | $38,335 | $723 | |||
| Subtotal | $2,798 | |||||
| Subtotal, Built-in | $7,812 | |||||
| CHANGES | FY 2022 CR | FY 2023 President's Budget | Program change from FY 2022 CR | |||
| No. | Amount | No. | Amount | No. | Amount | |
| B. Program: | ||||||
| 1. Research Project Grants: | ||||||
| a. Noncompeting | 1,647 | $953,193 | 1,578 | $965,645 | -69 | $12,452 |
| b. Competing | 587 | $419,898 | 618 | $484,433 | 31 | $64,536 |
| c. SBIR/STTR | 89 | $64,422 | 95 | $68,031 | 6 | $3,608 |
| Subtotal, RPGs | 2,323 | $1,437,513 | 2,291 | $1,518,109 | -32 | $80,596 |
| 2. Research Centers | 39 | $86,559 | 43 | $95,274 | 4 | $8,715 |
| 3. Other Research | 429 | $111,608 | 429 | $111,899 | 0 | $292 |
| 4. Research Training | 781 | $48,966 | 779 | $49,896 | 2 | $930 |
| 5. Research and development contracts | 136 | $106,187 | 141 | $113,620 | 5 | $7,433 |
| Subtotal, Extramural | $1,790,833 | $1,888,799 | $97,966 | |||
| FTEs | FTEs | FTEs | ||||
| 6. Intramural Research | 300 | $215,301 | 300 | $221,615 | 0 | $1,301 |
| 7. Research Management and Support | 289 | $97,575 | 289 | $100,414 | 0 | $41 |
| 8. Construction | $0 | $0 | $0 | |||
| 9. Buildings and Facilities | $0 | $0 | $0 | |||
| Subtotal, Program | 589 | $2,103,708 | 589 | $2,210,828 | 0 | $99,308 |
| Total buil-in and program changes | $107,120 | |||||
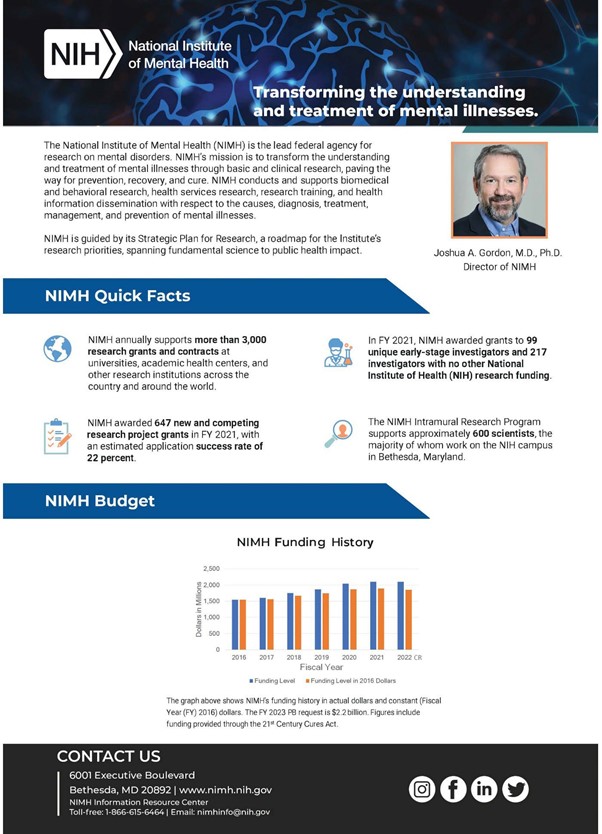
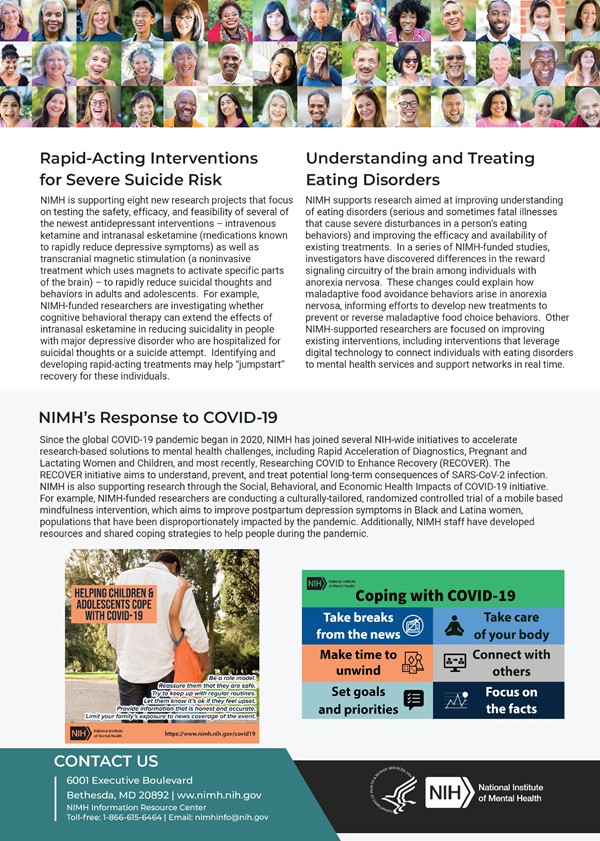
Budget Graphs
History of Budget Authority and FTEs:
Distribution by Mechanism:
Change by Selected Mechanism:

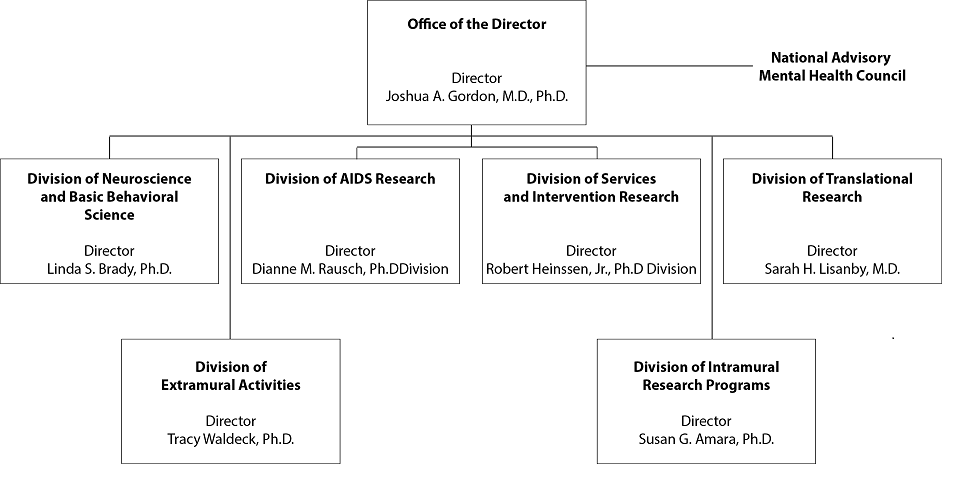
Organization Chart
National Institutes of Health
National Institute of Mental Health
NATIONAL INSTITUTES OF HEALTH
National Institute of Mental Health
Budget Authority by Activity1
(Dollars in Thousands)
| Extramural Research | FY 2021 Final | FY 2022 CR | FY 2023 President's Budget | FY 2023 +/- FY 2022 CR | ||||
|---|---|---|---|---|---|---|---|---|
| FTE | Amount | FTE | Amount | FTE | Amount | FTE | Amount | |
| Detail | ||||||||
| Neuroscience & Basic Behavioral Science | $786,159 | $787,236 | $833,863 | $46,627 | ||||
| Services & Intervention Research | $202,428 | $202,705 | $214,711 | $12,006 | ||||
| Translational Research | $515,027 | $515,732 | $546,278 | $30,546 | ||||
| AIDS Research | $175,403 | $173,834 | $176,028 | $2,194 | ||||
| Office of the Director | $111,173 | $111,325 | $117,919 | $6,594 | ||||
| Subtotal, Extramural | $1,790,190 | $1,790,833 | $1,888,799 | $97,966 | ||||
| Intramural Research | 289 | $212,800 | 300 | $215,301 | 300 | $221,615 | 0 | $6,315 |
| Research Management & Support | 278 | $96,746 | 289 | $97,575 | 289 | $100,414 | 0 | $2,839 |
| Total | 567 | $2,099,736 | 589 | $2,103,708 | 589 | $2,210,828 | 0 | $107,120 |
1Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
Justification of Budget Request
National Institute of Mental Health
Authorizing Legislation: Section 301 and title IV of the Public Health Service Act, as amended.
Budget Authority (BA):
| FY 2021 Final | FY 2022 CR | FY 2023 President’s Budget | FY 2023 +/- FY 2022 | |
|---|---|---|---|---|
| BA | $2,099,736,000 | $2,103,708,000 | $2,210,828,000 | +$107,120,000 |
| FTE | 567 | 589 | 589 | 0 |
[Top]
Program funds are allocated as follows: Competitive Grants/Cooperative Agreements; Contracts; Direct Federal/Intramural and Other.
Overall Budget Policy: The FY 2023 President’s Budget request is $2,210.8 million, an increase of $107.1 million or 5.1 percent compared to the FY 2022 Continuing Resolution (CR) level. The request includes $25.0 million in funding to increase research on the impact of the COVID- 19 pandemic on mental health. This will be done in part by utilizing participants in existing cohort studies, who will be surveyed on the effect of the pandemic and various mitigation measures on their physical and mental health. In addition, the request includes an increase of $5.0 million to support studies of the social media impact on mental health and another $5.0 million to support studies to inform mental health treatment approaches, service delivery, and system transformation.
Program Descriptions
Office of the Director
The NIMH Office of the Director (OD) leads the Institute in carrying out the NIMH mission to transform the understanding and treatment of mental illnesses. The OD provides scientific leadership, sets programmatic priorities, coordinates cross-cutting programs, determines Institute policies, directly funds several research projects, and provides overall administrative and operational coordination for the Institute. The OD houses nine offices: Office on AIDS; Office of Autism Research Coordination; Office of Clinical Research; Office of Genomics Research Coordination; Office for Disparities Research and Workforce Diversity; Office of Management; Office of Rural Mental Health Research; Office of Science Policy, Planning, and Communications; and Office of Technology Development and Coordination. Each of the offices within the OD play an important role in supporting the Institute.
As an example of research that OD funds, NIMH is currently supporting the development and testing of systems-level interventions directed toward high-risk youth to reduce or prevent suicide and suicidal behavior.53 Systems- level strategies enable effective suicide prevention interventions to be rapidly scaled up, making these interventions more broadly available, more easily accessed, and more effectively delivered. In alignment with the National Action Alliance for Suicide Prevention, NIMH continues to pursue the goal of reducing the rate of suicide in the United States by 20 percent by the year 2025.54 Suicide is the second leading cause of death for youth aged 10 to 24 years, and certain subgroups of youth are at significantly elevated risk, so focusing research efforts on high-risk youth is critical to achieving this goal.
Budget Policy: The FY 2023 President’s Budget request is $117.9 million, an increase of $6.6 million or 5.9 percent compared with the FY 2022 CR level.
Aggregating Data to Address Mental Health Disparities Research Gaps
NIMH supports a research agenda aimed at understanding and reducing mental health disparities and increasing health equity. Mental health disparities are significant and well documented: for example, deaths by suicide are much more common in American Indians and Alaska Natives compared to the general population,55 and Black and Hispanic children may be diagnosed with autism at a later age compared to White children, delaying their access to services and supports.56 However, understanding the underlying mechanisms and identifying strategies to address these and other mental health disparities has proven elusive, in part because many studies do not have enough individuals from different populations with health disparities to characterize differences between subgroups and explore associated mechanisms. Recognizing this research gap, NIMH has announced support for research focused on aggregating existing data sets to better understand risk and protective factors, causes and trajectories, and effective interventions associated with mental health disparities.57 Aggregating data sets is an approach that has proven successful in previous research initiatives,58-61demonstrating the potential for this new initiative to contribute information that ultimately reduces health disparities and increases health equity.
Neuroscience and Basic Behavioral Science
The Division of Neuroscience and Basic Behavioral Science (DNBBS) supports research in the areas of basic molecular and cellular neuroscience, genetics, integrative neuroscience, research training, and drug discovery. In cooperation with other NIMH programs and the wider research community, the Division ensures that relevant basic scientific knowledge is generated and used in pursuit of improved methods that, in the long term, could be used to diagnose, treat, and prevent mental illnesses.
DNBBS funds grants across a range of research topics to enhance understanding of the basic neurobiology underlying mental illnesses. In FY 2023, DNBBS plans to expand research into how glia, an understudied class of cells in the brain, contribute to neural circuits and ultimately behavior. DNBBS is also planning a broad, coordinated effort to understand how genetic alterations found in individuals with mental illnesses act in brain cells to cause changes in cellular and circuit function and ultimately behavior.
Budget Policy: The FY 2023 President’s Budget request is $833.9 million, an increase of $46.6 million or 5.9 percent compared with the FY 2022 CR level.
The Division of Translational Research (DTR) supports integrative, multidisciplinary research and training programs that translate findings from basic science to discover the causes, mechanisms, and trajectories of mental illnesses, and to develop effective interventions for individuals across the lifespan. DTR supports research using innovative forms of scientific analysis, including computational psychiatry and machine learning, to elucidate the characteristics of, and risk factors for, mental illnesses; the neurobehavioral mechanisms of psychopathology; the trajectories of risk and resilience based on the interactive influences of genetics, brain development, environment, and experience; and the design and testing of innovative treatments and interventions. As such, DTR-supported research efforts may have intermediate-term impact and pave the way towards effective treatment and prevention for mental illnesses.
One area of high priority for DTR is to improve outcomes for individuals at clinical high risk for psychosis. To accelerate progress towards this goal, NIMH and the Foundation for NIH launched AMP® SCZ, as detailed in the Director’s Overview section above.62 This flagship study builds upon the successes of prior investments to identify biomarkers of risk for progression to schizophrenia; such studies include the North American Prodrome Longitudinal Study (NAPLS) which identified promising biomarkers of risk63,64 and developed a risk calculator to predict conversion to psychosis.65 In collaboration with the Department of Defense, private foundations, and industry, DTR supports the Advancing Understanding of RecOvery afteR traumA (AURORA) Study,66 a landmark study to understand the consequences of trauma. Additionally, DTR supports research using advanced digital techniques (including natural language processing,67 machine learning, and predictive coding68) to predict mental health outcomes such as risk for suicide, and to facilitate the development of precision medicine approaches to prevent and treat post-traumatic stress disorder. DTR also supports work harnessing the latest advances in artificial intelligence to advance mechanistic understanding of how circuits in the brain shape behavior.69
Social Disconnection and Suicide Risk in Late Life
Suicide rates are significantly elevated among older adults, though the age of greatest risk differs between men (75+) and women (45-64).70 Older adults are also more likely to be socially disconnected due to exiting the workforce, experiencing bereavement, and enduring functional limitations that limit both in-person and remote/digital social interactions. Social isolation is associated with as much as a three-fold greater risk of suicide in middle and late life,71 and loneliness doubles the odds of experiencing suicidal thoughts later in life.72 As the American population rapidly ages – over 20 percent of the population will be over the age of 65 by 2030 – there is an urgent need to advance our mechanistic understanding of this link between social disconnection and suicide risk and to develop interventions to address social disconnection and prevent suicide. In response to this need, NIMH is seeking to support research identifying the neurobiological and environmental mechanisms associated with social isolation and loneliness that increase risk for suicidal thoughts and behavior in late life, identifying treatment targets for new interventions, and optimizing existing interventions in collaboration with health care and community services that serve elderly patients.73,74
Budget Policy: The FY 2023 President’s Budget request is $546.3 million, an increase of $30.5 million or 5.9 percent compared with the FY 2022 CR level.
Services and Intervention Research The Division of Services and Intervention Research (DSIR) supports research thatevaluates the effectiveness of psychosocial, pharmacological, somatic, rehabilitative, and combined interventions to prevent or treat mental illnesses. DSIR-supported research refines and evaluates treatment and preventive interventions across the lifespan, focusing on acute and long-term symptom reduction, remission, and improved community functioning. DSIR also supports mental health services research, including interventions to improve the quality and outcomes of care; organization- and system- level interventions to enhance service delivery; and strategies for widespread dissemination and implementation of evidence-based treatments into routine care settings. DSIR funds studies that are designed to have rapid impact, targeted at improving care for individuals with mental illnesses.
DSIR initiatives encourage practice-based research with near-term potential for improving intervention effectiveness and service delivery, as illustrated by the Advanced Laboratories for Accelerating the Reach and Impact of Treatments for Youth and Adults with Mental Illness (ALACRITY) Research Centers program.75,76 ALACRITY-funded researchers aim to increase the effectiveness of existing interventions; improve the delivery and quality of evidence-based services; and accelerate the implementation and continuous improvement of new practices among key populations and in diverse health care settings. Many of the centers leverage digital health platforms and data science methods to learn about mental illness onset and progression in clinical populations, improve diagnosis, and deliver targeted interventions via mobile health technologies. Since it first launched in 2017, the ALACRITY program has supported 205 publications. Building on the successful ALACRITY Center model, in FY 2021, NIMH launched a parallel Advanced Center research program, Practice-Based Suicide Prevention Research Centers, to address NIMH suicide prevention priorities and help reduce the national suicide rate.77,78
Budget Policy: The FY 2023 President’s Budget request is $214.7 million, an increase of $12.0 million or 5.9 percent compared with the FY 2022 CR level.
Using Just-in-Time Adaptive Interventions to Optimize Established Adolescent Mental Health Treatments
Decades of adolescent mental health interventions research has resulted in an arsenal of evidence-based psychotherapies. However, the majority of these evidence-based psychotherapies only modestly outperform usual care for youth mental disorders, especially for anxiety disorder, conduct disorder, and attentiondeficit/ hyperactivity disorder.79,80 Additionally, adolescence is a developmental period characterized by heightened risk for new onset or worsening mental illness, and adolescents struggle to engage with and adhere to traditional face-to-face interventions more than any other age group, suggesting a need for digital alternatives. To meet this need, NIMH is supporting research focused on enhancing the potency of established adolescent mental health treatments through the use of developmentally informed and theoretically grounded just-in-time adaptive interventions (JITAIs).81 JITAIs use smartphone and/or sensor data to monitor an individual’s behavior or state and deliver responsive, tailored micro-interventions at opportune moments. The increasing availability of powerful mobile and sensing technologies has now made it feasible to test the clinical impact of JITAIs. By supporting JITAI research, NIMH hopes to capitalize on this unique intersection of emerging technology and intervention science to improve the effectiveness of treatments for adolescent mental disorders.
The Division of AIDS Research (DAR) supports research and research training that addresses the priority areas outlined in the NIH Strategic Plan for HIV and HIV-Related Research82 and the HHS National HIV/AIDS Strategy.83 DAR-supported research includes behavioral and social science studies aimed at reducing HIV/AIDS incidence through the development, testing, and implementation of new and improved prevention strategies, as well as improving health outcomes of individuals living with HIV through improved linkage to care and adherence to effective treatments. DAR also supports research to understand, prevent, and treat the neurological disorders and mental illnesses associated with living with HIV. DAR is participating in cure research by supporting studies to eradicate or silence HIV from biological reservoirs in the central nervous system (CNS), where the virus may evade detection and treatment. HIV latency in the CNS is critically important to consider in studies of eradication and reactivation. Many drugs designed to eradicate the virus are unable to penetrate the blood-brain barrier of the CNS, which thus provides a protective reservoir for HIV.
DAR encourages targeted research to understand the mechanisms underlying HIV-induced neuronal pathology and the resulting motor and cognitive dysfunction that results, with the goal of identifying preventive and therapeutic interventions.
DAR research also places special emphasis on World Health Organization-defined key populations, health disparities, and the impact of mental illnesses that may increase the risk for contracting HIV or negatively impact the health outcomes of individuals living with HIV. Additionally, DAR engages with multidisciplinary experts in NIH-wide planning efforts to ensure effective integration of behavioral and biomedical approaches to help achieve an AIDS- free generation.
Budget Policy: The FY 2023 President’s Budget request is $176.0 million, an increase of $2.2 million or 1.3 percent compared with the FY 2022 CR level.
The Division of Intramural Research Programs (IRP) is the internal research component of NIMH, complementing the Institute’s extramural grant funding program. IRP scientists investigate basic, translational, and clinical aspects of brain function and behavior, conducting state-of-the-art research using unique NIH resources. In addition, the IRP provides an excellent environment for training the next generation of basic and clinical scientists.
IRP researchers are developing new and improved methods in functional magnetic resonance imaging (fMRI) and exploring advanced computational methods to evaluate brain function and mental illnesses. Many IRP researchers use fMRI and behavioral tasks to investigate differences in brain circuitry underlying key brain functions such as learning, perception, and attention, which are affected in mental illnesses. IRP researchers use cutting edge genetic techniques to investigate the circuitry underlying behavioral responses to threat,84 which are aberrant in individuals with anxiety disorders. To better understand how mental disorders emerge, IRP scientists use innovative analyses of extensive clinical, genetic, and brain imaging datasets to study the effects of gene expression and sex differences on brain anatomy during development.85,86 IRP scientists are also exploring novel medications and other treatments for depression in adults, including ketamine and other experimental fast-acting antidepressant medications, transcranial magnetic stimulation (TMS), and next generation seizure therapy.
Using clinical assessments, brain imaging, and sleep studies, they aim to better understand suicide.87 IRP researchers also developed the Ask Suicide-Screening Questions (ASQ) tool for use among both youth and adults in various medical settings.88 To help researchers around the world implement pilot suicide risk screening programs, IRP researchers work closely with colleagues in the NIMH Center for Global Mental Health Research and collaborate with other government agencies such as the Indian Health Service.
Budget Policy: The FY 2023 President’s Budget request is $221.6 million, an increase of $6.3 million or 2.9 percent compared with the FY 2022 CR level.
Research Management and Support
Research Management and Support (RMS) activities provide administrative, budgetary, logistical, and scientific support in the review, award, and monitoring of research and training grants, as well as for research and development contracts. RMS functions include coordination and evaluation of NIMH programs, regulatory compliance, and liaising with other federal agencies, Congress, and the public. Through RMS activities, NIMH continues to provide accountability and administrative support for meritorious basic, translational, and clinical research and continues to promote health information dissemination, education, and outreach activities.
Budget Policy: The FY 2023 President’s Budget request is $100.4 million, an increase of $2.8 million or 2.9 percent compared with the FY 2022 CR level.
Appropriations History
| Fiscal Year | Budget Estimate to Congress | House Allowance | Senate Allowance | Appropriation |
|---|---|---|---|---|
| 2014 | $1,465,782,000 | $1,456,041,000 | $$1,446,172,000 | |
| Rescission | $0 | |||
| 2015 | $1,440,076,000 | $1,463,036,000 | ||
| Rescission | $0 | |||
| 2016 | $1,489,417,000 | $1,512,401,000 | $1,520,260,000 | $1,548,390,000 |
| Rescission | $0 | |||
| 2017 | $1,518,673,000 | $1,599,747,000 | $1,619,537,000 | $1,601,931,000 |
| Rescission | $0 | |||
| 2018[1] | $1,244,901,000 | $1,668,461,000 | $1,724,568,000 | $1,754,775,000 |
| Rescission | $0 | |||
| 2019[2] | $1,612,192,000 | $1,790,231,000 | $1,871,250,000 | $1,870,296,000 |
| Rescission | $0 | |||
| 2020[2] | $1,630,422,000 | $1,961,704,000 | $2,076,244,000 | $2,038,374,000 |
| Rescission | $0 | |||
| 2021[2] | $1,844,865,000 | $2,060,303,000 | $2,139,491,000 | $2,103,708,000vvvv |
| Rescission | $0 | |||
| 2022[2] | $2,213,574,000 | $2,223,085,000 | $2,218,900,000 | $2,103,708,000 |
| Rescission | $0 | |||
| 2023[2] | $2,210,828,000 |
1 Budget Estimate to Congress includes mandatory financing.
2 Includes funds derived by transfer from the NIH Innovation Account under the 21st Century Cures Act
[Top]
Authorizing Legislation
| PHS Act/Other Citation | U.S. Code Citation | 2022 Amount Authorized | FY 2022 CR | 2023 Amount Authorized | FY 2023 President’s Budget | |||
|---|---|---|---|---|---|---|---|---|
| Research and Investigation | Section 301 | 42§241 | Indefinite | $2,103,708,000 | Indefinite | $2,210,828,000 | ||
| National Institute of Mental Health | Section 401(a) | 42§281 | Indefinite | Indefinite | ||||
| Total Budget Authority | $2,103,708,000 | $2,210,828,000 | ||||||
[Top]
Amounts Available for Obligation
| Source of Funding | FY 2021 Final |
FY 2022 CR |
FY 2023 President's Budget* |
| Appropriation2 | $2,103,708 | $2,103,708 | $2,210,828 |
| Secretary's Transfer | -$6,166 | $0 | $0 |
| OAR HIV/AIDS Transfers | $2,194 | $0 | $0 |
| Subtotal, adjusted budget authority | $2,099,736 | $2,103,708 | $2,210,828 |
| Unobligated balance, start of year3 | $2,022 | $2,338 | $0 |
| Unobligated balance, end of year (carryover)3 | -$2,338 | $0 | $0 |
| Subtotal, adjusted budget authority | $2,099,420 | $2,106,046 | $2,210,828 |
| Unobligated balance lapsing | -$10 | $0 | $0 |
| Total obligations | $2,099,410 | $2,106,046 | $2,210,828 |
1 Excludes the following amounts (in thousands) for reimbursable activities carried out by this account: FY 2021 - $6,019 FY 2022 - $10,050 FY 2023 - $10,050
2 Of which $50.0 million in FY 2021, $50.0 million in FY 2022, and $225.0 million in FY 2023 is derived by transfer from the NIH Innovation Account under the 21st Century Cures Act.
3 Reflects 21st Century Cures Act funding not obligated in previous years and carried over into FY 2022.
[Top]
Budget Authority by Object Class
| FY 2022 CR | FY 2023 President's Budget | FY 2023 +/ - FY 2022 | |
| Total compensable workyears: | |||
| Full-time equivalent | 589 | 589 | 0 |
| Full-time equivalent of overtime and holiday hours | 0 | 0 | 0 |
| Average ES salary | $204 | $208 | $5 |
| Average GM/GS grade | 12.9 | 12.9 | 0.0 |
| Average GM/GS salary | $128 | $132 | $4 |
| Average salary, Commissioned Corps (42 U.S.C. 207) | $0 | $0 | $0 |
| Average salary of upgraded positions | $162 | $174 | $12 |
| OBJECT CLASSES | FY 2022 CR | FY 2023 President's Budget | FY 2023 +/ - FY 2022 |
| Personnel Compensation | |||
| 11.1 Full-Time Permanent | $53,823 | $56,774 | $2,950 |
| 11.3 Other Than Full-Time Permanent | $26,644 | $27,250 | $606 |
| 11.5 Other Personnel Compensation | $2,929 | $2,995 | $67 |
| 11.7 Military Personnel | $0 | $0 | $0 |
| 11.8 Special Personnel Services Payments | $11,874 | $12,467 | 593 |
| 11.9 Subtotal Personnel Compensation | $95,270 | $99,486 | $4,216 |
| 12.1 Civilian Personnel Benefits | $31,538 | $33,481 | $1,943 |
| 12.2 Military Personnel Benefits | $0 | $0 | $0 |
| 13.0 Benefits to Former Personnel | $0 | $0 | $0 |
| Subtotal Pay Costs | $126,807 | $132,967 | $6,159 |
| 21.0 Travel & Transportation of Persons | $71 | $72 | $1 |
| 22.0 Transportation of Things | $175 | $176 | $1 |
| 23.1 Rental Payments to GSA | $0 | $0 | $0 |
| 23.2 Rental Payments to Others | $0 | $0 | $0 |
| 23.3 Communications, Utilities & Misc. Charges | $884 | $897 | $13 |
| 24.0 Printing & Reproduction | $0 | $0 | $0 |
| 25.1 Consulting Services | $63,888 | $65,545 | $1,657 |
| 25.2 Other Services | $45,026 | $46,182 | $1,156 |
| 25.3 Purchase of goods and services from government accounts | $137,010 | $143,127 | $6,117 |
| 25.4 Operation & Maintenance of Facilities | $391 | $402 | $1 1 |
| 25.5 R&D Contracts | $19,005 | $19,932 | $927 |
| 25.6 Medical Care | $37 | $37 | $0 |
| 25.7 Operation & Maintenance of Equipment | $11,189 | $11,548 | $359 |
| 25.8 Subsistence & Support of Persons | $0 | $0 | $0 |
| 25.0 Subtotal Other Contractual Services | $276,546 | $286,773 | $10,227 |
| 26.0 Supplies & Materials | $4,614 | $4,705 | $91 |
| 31.0 Equipment | $8,108 | $8,200 | $93 |
| 32.0 Land and Structures | $1,857 | $1,859 | $2 |
| 33.0 Investments & Loans | $0 | $0 | $0 |
| 41.0 Grants, Subsidies and Contributions | $1,684,646 | $1,775,179 | $90,533 |
| 42.0 Insurance Claims and Indemnities | $0 | $0 | $0 |
| 43.0 Interest & Dividends | $1 | $1 | $0 |
| 44.0 Refunds | $0 | $0 | $0 |
| Subtotal Non-Pay Costs | $1,976,901 | $2,077,861 | $100,961 |
| Total Budget Authority by Object Class | $2,103,708 | $2,210,828 | $107,120 |
1 Includes FTEs whose payroll obligations are supported by the NIH Common Fund.
[Top]
Salaries and Expenses
(Dollars in Thousands)
| OBJECT CLASSES | FY 2022 CR | FY 2023 President's Budget | FY 2023 +/ - FY 2022 |
| Personnel Compensation | |||
| Full-Time Permanent (11.1) | $53,823 | $56,774 | $2,950 |
| Other Than Full-Time Permanent (11.3) | $26,644 | $27,250 | $606 |
| Other Personnel Compensation (11.5) | $2,929 | $2,995 | $67 |
| Military Personnel (11.7) | $0 | $0 | $0 |
| Special Personnel Services Payments (11.8) | $11,874 | $12,467 | $593 |
| Subtotal Personnel Compensation (11.9) | $95,270 | $99,486 | $4,216 |
| Civilian Personnel Benefits (12.1) | $31,538 | $33,481 | $1,943 |
| Military Personnel Benefits (12.2) | $0 | $0 | $0 |
| Benefits to Former Personnel (13.0) | $0 | $0 | $0 |
| Subtotal Pay Costs | $126,807 | $132,967 | $6,159 |
| Travel & Transportation of Persons (21.0) | $71 | $72 | $1 |
| Transportation of Things (22.0) | $175 | $176 | $1 |
| Rental Payments to Others (23.2) | $0 | $0 | $0 |
| Communications, Utilities & Misc. Charges (23.3) | $884 | $897 | $13 |
| Printing & Reproduction (24.0) | $0 | $0 | $0 |
| Other Contractual Services: | |||
| Consultant Services (25.1) | $52,857 | $53,957 | $1,100 |
| Other Services (25.2) | $45,026 | $46,182 | $1,156 |
| Purchases from government accounts (25.3) | $47,370 | $54,438 | $7,068 |
| Operation & Maintenance of Facilities (25.4) | $391 | $402 | $11 |
| Operation & Maintenance of Equipment (25.7) | $11,189 | $11,548 | $359 |
| Subsistence & Support of Persons (25.8) | $0 | $0 | $0 |
| Subtotal Other Contractual Services | $156,832 | $166,526 | $9,694 |
| Supplies & Materials (26.0) | $4,614 | $4,705 | $91 |
| Subtotal Non-Pay Costs | $162,577 | $172,376 | $9,799 |
| Total Administrative Costs | $289,384 | $305,342 | $15,958 |
[Top]
Detail of Full-Time Equivalent Employment (FTE)
| Office/Division | FY 2021 Final | FY 2022 CR | FY 2023 President's Budget | ||||||
| Civilian | Military | Total | Civilian | Military | Total | Civilian | Military | Total | |
| Division of AIDS Research | |||||||||
| Direct: | 15 | - | 15 | 16 | - | 16 | 16 | - | 16 |
| Total: | 15 | - | 15 | 16 | - | 16 | 16 | - | 16 |
| Division of Extramural Activities | |||||||||
| Direct: | 40 | - | 40 | 40 | - | 40 | 40 | - | 40 |
| Total: | 40 | - | 40 | 40 | - | 40 | 40 | - | 40 |
| Division of Intramural Research Programs | |||||||||
| Direct: | 287 | - | 287 | 298 | - | 298 | 298 | - | 298 |
| Reimbursable: | 2 | - | 2 | 2 | - | 2 | 2 | - | 2 |
| Total: | 289 | - | 289 | 300 | - | 300 | 300 | - | 300 |
| Division of Neuroscience and Basic Behavioral Science | |||||||||
| Direct: | 29 | - | 29 | 29 | - | 29 | 29 | - | 29 |
| Total: | 29 | - | 29 | 29 | - | 29 | 29 | - | 29 |
| Division of Services and Intervention Research | |||||||||
| Direct: | 15 | - | 15 | 15 | - | 15 | 15 | - | 15 |
| Total: | 15 | - | 15 | 15 | - | 15 | 15 | - | 15 |
| Division of Translational Research | |||||||||
| Direct: | 29 | - | 29 | 29 | - | 29 | 29 | - | 29 |
| Total: | 29 | - | 29 | 29 | - | 29 | 29 | - | 29 |
| Office of the Director | |||||||||
| Direct: | 140 | - | 140 | 150 | - | 150 | 150 | - | 150 |
| Reimbursable: | 10 | - | 10 | 10 | - | 10 | 10 | - | 10 |
| Total: | 150 | - | 150 | 160 | - | 160 | 160 | - | 160 |
| Total | 567 | - | 567 | 589 | - | 589 | 589 | - | 589 |
| Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||||||||
| FTE's supported by funds from Cooperative Research and Development Agreements | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Fiscal Year | Average GS Grade |
| 2019 | 12.8 |
| 2020 | 12.8 |
| 2021 | 12.9 |
| 2022 | 12.9 |
| 2023 | 12.9 |
[Top]
Detail of Positions
| Grade | FY 2021 Final Final |
FY 2022 CR |
FY 2023 President's Budget |
|---|---|---|---|
| Total, ES Positions | 1 | 1 | 1 |
| Total, ES Salary | $199,300 | $203,834 | $208,471 |
| GM/GS-15 | 77 | 83 | 83 |
| GM/GS-14 | 82 | 88 | 88 |
| GM/GS-13 | 115 | 124 | 124 |
| GS-12 | 85 | 91 | 91 |
| GS-11 | 29 | 31 | 31 |
| GS-10 | 0 | 0 | 0 |
| GS-9 | 17 | 18 | 18 |
| GS-8 | 6 | 6 | 6 |
| GS-7 | 1 | 1 | 1 |
| GS-6 | 0 | 0 | 0 |
| GS-5 | 0 | 0 | 0 |
| GS-4 | 1 | 1 | 1 |
| GS-3 | 1 | 1 | 1 |
| GS-2 | 0 | 0 | 0 |
| GS-1 | 0 | 0 | 0 |
| Subtotal | 414 | 444 | 444 |
| Commissioned Corps (42 U.S.C. 207): | 0 | 0 | 0 |
| Assistant Surgeon General | 0 | 0 | 0 |
| Director Grade | 0 | 0 | 0 |
| Senior Grade | 0 | 0 | 0 |
| Full Grade | 0 | 0 | 0 |
| Senior Assistant Grade | 0 | 0 | 0 |
| Assistant Grade | 0 | 0 | 0 |
| Subtotal | 0 | 0 | 0 |
| Ungraded | 170 | 170 | 170 |
| Total permanent positions | 417 | 417 | 417 |
| Total positions, end of year | 575 | 578 | 590 |
| Total full-time equivalent (FTE) employment, end of year | 567 | 589 | 589 |
| Average ES salary | $199,300 | $203,834 | $208,471 |
| Average GM/GS grade | 12.9 | 12.9 | 12.9 |
| Average GM/GS salary | $124,700 | $128,385 | $132,178 |
| 1Includes FTEs whose payroll obligations are supported by the NIH Common Fund. | |||
References:
1 Substance Abuse and Mental Health Services Administration. (2020). Key substance use and mental health indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (HHS Publication No. PEP20-07-01-001, NSDUH Series H-55). Rockville, MD: Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration. Retrieved from www.samhsa.gov/data
2 Institute of Health Metrics and Evaluation. ghdx.healthdata.org/gbd-results-tool accessed October 2021.
3 CDC, NCIPC. WISQARS: www.cdc.gov/injury/wisqars/index.html accessed October 2021.
4 www.nimh.nih.gov/about/strategic-planning-reports
5 www.nimh.nih.gov/sites/default/files/documents/about/strategic-planning-reports/SP2020-ProgressReport - FINAL.pdf
6 www.fda.gov/news-events/press-announcements/fda-approves-new-nasal-spray-medication-treatment-resistant-depression-available-only-certified
7 www.nimh.nih.gov/news/research-highlights/2021/nimh-addresses-critical-need-for-rapid-acting-interventions-for-severe-suicide-risk
8 reporter.nih.gov/project-details/10115267
9 www.nimh.nih.gov/news/science-news/2021/study-identifies-risk-factors-for-elevated-anxiety-in-young-adults-during-covid-19-pandemic
10 covid19.nih.gov/news-and-stories/covid19-ripple-effects
11 www.nimh.nih.gov/about/director/messages/coping-with-traumatic-events
12 www.nimh.nih.gov/get-involved/education-awareness/shareable-resources-on-coping-with-covid-19
13 grants.nih.gov/grants/guide/notice-files/NOT-MH-20-073.html
14 grants.nih.gov/grants/guide/notice-files/NOT-MH-21-190.html
15 www.nimh.nih.gov/news/science-news/2021/nimh-directors-statement-our-commitment-to-ending-structural-racism-in-biomedical-research
16 www.nimh.nih.gov/health/topics/schizophrenia/raise/raise-questions-and-answers
17 www.nimh.nih.gov/health/topics/schizophrenia/raise/raise-questions-and-answers#11
18 www.pubmed.ncbi.nlm.nih.gov/26481174/
19 www.nimh.nih.gov/news/science-news/2019/nih-announces-funding-awards-for-national-early-psychosis-learning-community
21 www.nationalepinet.org/core-assessment-battery-cab/
22 www.nimh.nih.gov/health/statistics/schizophrenia
23 www.nimh.nih.gov/research/research-funded-by-nimh/research-initiatives/accelerating-medicines-partnership-schizophrenia-amp-scz
24 www.nimh.nih.gov/news/research-highlights/2020/nimh-part-of-collaborative-effort-to-advance-early-intervention-for-individuals-at-risk-of-developing-schizophrenia
25 reporter.nih.gov/project-details/10092863
26 reporter.nih.gov/project-details/10093852
27 reporter.nih.gov/project-details/10092398
28 www.nimh.nih.gov/news/research-highlights/2020/using-mobile-technology-to-improve-care-for-teens-with-depression
29 www.nimh.nih.gov/news/research-highlights/2020/supporting-the-development-of-early-autism-screening-tools
30 fnih.org/what-we-do/biomarkers-consortium/programs/autism-biomarkers
31 www.nimh.nih.gov/news/research-highlights/2020/testing-and-refining-biomarkers-to-support-intervention-research-for-children-with-autism
32 www.cdc.gov/injury/wisqars/index.html
33 www.nimh.nih.gov/news/science-news/2021/adaptive-screener-may-help-identify-youth-at-risk-of-suicide
34 www.nimh.nih.gov/health/topics/eating-disorders
35 www.nimh.nih.gov/about/director/messages/2021/from-brain-mechanisms-to-novel-therapies-understanding-and-treating-eating-disorders
36 pubmed.ncbi.nlm.nih.gov/26457555/
37 pubmed.ncbi.nlm.nih.gov/28231717/
38 reporter.nih.gov/search/00FFC5M4aUaD_UormL30YQ/project-details/9805065
39 reporter.nih.gov/search/Yjhumy3a1ka9fvLtxs-QWA/project-details/9917857
40 reporter.nih.gov/search/SXbl2ZEKsk-IhNNJWdt3qw/project-details/9955368
41 reporter.nih.gov/search/30XS75iUuEuc2eRIAkqCBQ/project-details/10085684
42 reporter.nih.gov/search/oYAe6oEOgE6ZuIRNdv8qLw/project-details/9984537
43 reporter.nih.gov/search/bP-DZ7IpRU6iyrBOfs8qjg/project-details/10096423
44 braininitiative.nih.gov/about/overview
45 braininitiative.nih.gov/brain-programs/cell-census-network-biccn
46 www.nature.com/nature/volumes/598/issues/7879
48 www.nimh.nih.gov/about/director/messages/2021/a-milestone-in-mapping-the-brain
49 www.nimh.nih.gov/news/science-news/2020/nih-funded-study-sheds-light-on-abnormal-neural-function-in-rare-genetic-disorder
50 www.nimh.nih.gov/research/research-funded-by-nimh/rdoc/about-rdoc
51 www.nimh.nih.gov/about/director/messages/2020/rdoc-at-ten-years-part-1
52 www.nimh.nih.gov/about/director/messages/2020/rdoc-at-ten-years-part-2-the-next-ten-years
53 www.nimh.nih.gov/funding/grant-writing-and-application-process/concept-clearances/2020/systems-level-interventions-for-detecting-and-preventing-suicide-and-suicidal-behavior-in-at-risk-youth
54 theactionalliance.org/news/national-action-alliance-suicide-prevention-announces-goal-reduce-suicide-20-percent-2025
55 www.cdc.gov/mmwr/volumes/67/wr/mm6708a1.htm
56 www.cdc.gov/ncbddd/autism/addm-community-report/spotlight-on-closing-racial-gaps.html
57 www.nimh.nih.gov/funding/grant-writing-and-application-process/concept-clearances/2021/addressing-mental-health-disparities-research-gaps-aggregating-and-mining-existing-data-sets-for-secondary-analyses
58 grants.nih.gov/grants/guide/rfa-files/rfa-mh-18-400.html
59 grants.nih.gov/grants/guide/rfa-files/rfa-mh-18-410.html
60 grants.nih.gov/grants/guide/rfa-files/rfa-mh-20-305.html
61 grants.nih.gov/grants/guide/rfa-files/rfa-mh-20-307.html
62 www.nih.gov/news-events/news-releases/nih-public-private-partnership-advance-early-interventions-schizophrenia
63 www.pubmed.ncbi.nlm.nih.gov/33667856/
64 www.pubmed.ncbi.nlm.nih.gov/29971330/
65 www.ncbi.nlm.nih.gov/pmc/articles/PMC5048498/
66 https://reporter.nih.gov/project-details/10019595
67 www.pubmed.ncbi.nlm.nih.gov/30710497/
68 www.pubmed.ncbi.nlm.nih.gov/30389840/
69 www.grants.nih.gov/grants/guide/pa-files/PAR-19-344.html
70 www.cdc.gov/nchs/products/databriefs/db398.htm
71 pubmed.ncbi.nlm.nih.gov/26222043/
72 pubmed.ncbi.nlm.nih.gov/28910599/
73 www.nimh.nih.gov/funding/grant-writing-and-application-process/concept-clearances/2021/research-on-late-life-suicide-mechanisms-and-future-treatment-targets
74 www.nimh.nih.gov/news/events/2020/virtual-workshop-social-disconnection-and-late-life-suicide-mechanisms-treatment-targets-and-interventions
75 grants.nih.gov/grants/guide/pa-files/PAR-16-354.html
76 grants.nih.gov/grants/guide/pa-files/PAR-18-701.html
77 grants.nih.gov/grants/guide/pa-files/PAR-20-286.html
79 pubmed.ncbi.nlm.nih.gov/23754332/
80 www.nimh.nih.gov/funding/grant-writing-and-application-process/concept-clearances/2021/just-in-time-adaptive-interventions-to-optimize-adolescent-mental-health-treatments
81 pubmed.ncbi.nlm.nih.gov/27663578/
82 oar.nih.gov/hiv-policy-and-research/strategic-plan
83 www.hiv.gov/blog/hhs-and-the-national-hivaids-strategy
84 pubmed.ncbi.nlm.nih.gov/34413514/
85 pubmed.ncbi.nlm.nih.gov/33811142/
86 pubmed.ncbi.nlm.nih.gov/34294918/
87 clinicaltrials.gov/ct2/show/NCT02543983
88 www.nimh.nih.gov/research/research-conducted-at-nimh/asq-toolkit-materials
