Goal 1: Define the Brain Mechanisms Underlying Complex Behaviors
Through basic science, researchers endeavor to answer fundamental questions about the mechanisms (e.g., brain, behavioral, environmental, psychosocial) that contribute to cognition, perception, motivation, and social behavior. We have seen extraordinary progress in basic science over the past several years, including in neuroscience. New tools have enabled precise mapping and the ability to modulate brain circuits across model systems, from cells in a dish to the human brain. New techniques have improved the resolution of structural and functional imaging in humans. New sensor technologies are transforming the study of behavior. These new tools, techniques, and technologies will help us piece together the many complex connections among genes, the brain, and behavior. Researchers are also exploring how these aspects of mental function become altered in mental illnesses.
The vast number of cells and connections in the brain make understanding its function in complex behavior particularly challenging. New tools and technologies are helping us create a detailed map of the circuits involved in complex behavior, including those associated with mental illnesses. For example, to address the range of individual variation in brain circuits, the Human Connectome Project provided a reference atlas of neuronal connectivity—or a connectome—of 1,200 healthy brains. Researchers are now mapping long-distance brain connections and looking at their variability in unprecedented detail. These efforts are underway across development and across mental illnesses.
The genomics revolution, fueled by technological advances, has revealed insights into the genetic architecture of mental illnesses. Over the past several years, large, replicated genomic studies have revealed many common and rare variants associated with the most heritable conditions (e.g., schizophrenia, bipolar disorder, autism). We are also making strides in identifying the genetic and nongenetic factors that control gene expression and play other roles in mental health and illness. While we have gone from few clues to many, we still cannot fully explain the root causes of mental illnesses. Researchers have begun the task of sorting through the complex patterns of genomic variation and environmental moderators to define and elucidate how these variations confer risk and resilience. We now know hundreds of identifying locations in the genome where genetic variation raises risk for psychiatric disorders. Because most participants in these studies have been of European descent, the findings may not be applicable to all. NIMH is expanding efforts to increase the diversity of the study participants across our genomics research to better benefit people of all racial and ethnic groups. Researchers are also exploring the role of nongenomic factors (e.g., the environment, experience, the microbiome) and their impact on the risk for mental illnesses, including their impact on gene expression.
We seek to understand how the interplay of molecular, cellular, circuit-level, genetic, and environmental factors influence the development of mental illnesses through animal and human studies. Multidisciplinary approaches integrating statistics, mathematics, physics, computer science, and engineering will help us begin to explain how our brain predicts, interprets, alters, and responds to a complex world. Through basic science, we will achieve a more refined understanding of the brain mechanisms underlying complex behaviors, which will drive progress toward the novel interventions of tomorrow.
The following Objectives further define this Goal:
To truly transform our understanding of mental illnesses, we need to identify the roles of all brain cell types and circuits in the myriad aspects of mental processes. Knowing how brain cells work together in circuits to drive cognitive, affective, and social processes will inform future circuit-based preventive and treatment interventions. New tools and techniques that span units of analysis (e.g., genes, molecules, cells, circuits, physiology, behavior) will transform our understanding of the brain, thus fostering our understanding of mental illnesses.
To better elucidate the brain mechanisms underlying cognitive, affective, and social processes, NIMH will support research that employs the following Strategies:
Interest areas include:
- Determining the phenotypic properties and dynamic interactions of neurons, astrocytes, oligodendrocytes, microglia, immune cells, and other cell types and how they contribute to brain organization and function.
- Exploring the genomic, molecular, and physiological factors in cell-to-cell variation and determining the functional consequences of this variation.
- Applying advanced neuroanatomical and functional approaches to map neural circuits at micro-, meso- and macro-scales.
Interest areas include:
- Elucidating the developmental processes that lead to the establishment of functional brain networks subserving these domains, including modifying factors (e.g., genomic, experiential) affecting these trajectories.
- Identifying the mechanisms that mediate normal cellular communication and plasticity at the level of molecular control, signal transduction, synapses, circuits, and/or behavior. Examining how alterations of these mechanisms may disrupt function; such mechanisms may involve non-neural components (e.g., immune system, microbiome, blood-brain barrier, vasculature).
- Developing and validating experimentally grounded theories for how the brain computes within these domains across spatiotemporal scales and levels of neurobiological abstraction (e.g., coordinated neural activity patterns and network state changes).
- Applying novel behavioral assays of the domains that are causally linked to specific mechanisms at multiple units of analysis (e.g., genetic, molecular, cellular, circuit, physiological, behavioral, systems). These approaches will be prioritized over studies relying on traditional behavioral tests that presume congruence with human symptoms of mental illnesses and do not give insight into the function of the circuit(s) under investigation.
- Evaluating the preclinical utility of modifying cellular, synaptic or circuit function for therapeutic benefit.
Interest areas include:
- Developing novel assays that can be used to interrogate key regulators of cellular communication using in situ and circuit-based models for screening, target discovery, and development of novel probes of cell function.
- Advancing human cell-based assays using induced pluripotent stem cells (iPSCs) for studying the molecular factors in mental illnesses, with an emphasis on optimizing robustness, scalability, reproducibility, and fidelity to in vivo human cell phenotypes, maturation, three-dimensional organization, and/or circuit function.
- Developing novel, age-appropriate imaging assays with higher spatial and temporal resolution for visualization and analyses of brain structure, maturation, connectivity, and function, with particular emphasis on advancing real-time measurement approaches.
- Developing innovative computational tools for the analysis and interpretation of neural activity including single unit, local field potentials, and other electrophysiological temporal dynamic patterns.
- Developing and validating novel, objective physiological and behavioral measures as research tools to assess synaptic plasticity and circuit function in experimental systems, and as assays for assessing therapeutic targets in humans.
- Advancing objective, quantitative assays to track, manipulate, and analyze behavior at high temporal resolution in a range of species, ages, and settings, and across multiple modalities and systems.
- Developing noninvasive assays for interrogating and manipulating brain circuit function for therapeutic purposes.
- Advancing novel assays to develop biomarkers of disease and for therapeutic discovery.
A full understanding of the multifaceted contributors to risk for mental illnesses requires examination of genomic, epigenomic, and other factors, including the environment and experience, worldwide. Understanding how these factors contribute to adaptive and maladaptive behaviors, mental function and dysfunction, and mental illnesses is critical for developing improved diagnostics and interventions that are effective for diverse individuals and populations. The genetic architecture of mental illnesses is extraordinarily complex. While the field of genomics has achieved remarkable advances in the past few years, the exact mechanisms that place certain individuals and populations at higher risk than others remain unknown. We need comprehensive approaches to understand genomic and non-genomic risk factors, and such investigations must consider diverse populations from around the world. To facilitate the transition of knowledge to practice, we need novel study designs, advanced genomic technologies, and innovative statistical and bioinformatic methods. These approaches will help us to revolutionize the analysis and interpretation of genetic associations and will speed the transition of this knowledge to practice.
To more effectively identify the genomic and non-genomic factors associated with mental illnesses, NIMH will support research that employs the following Strategies:
Interest areas include:
- Performing large, well-powered, whole genome and exome-, epigenome-, and other “ome”-wide studies in appropriate tissues.
- Elucidating genetic architecture and heritability across the full allele frequency spectrum.
- Mapping and identifying causal variants within risk loci.
- Analyzing co-heritability and shared genetic risk architecture using cross-trait analyses.
- Collecting and genomically characterizing ancestrally diverse cohorts.
Interest areas include:
- Conducting robust, well-powered, and unbiased genome-wide x phenome-wide association studies by leveraging large-scale genetic and phenotypic/exposure data from biobanks, health systems, and other population-scale cohorts.
- Conducting Mendelian randomization studies that identify modifiable exposures mediating or mitigating risk for mental illnesses.
- Developing epidemiologic studies that incorporate individual polygenic risk scores, and other genetic markers of risk, and leveraging existing large, population-based cohorts, including ethnically and ancestrally diverse cohorts, registries, and/or health systems to conduct analyses that advance understanding of the complex etiologies, trajectories, comorbidities, and treatment responses of severe mental illnesses.
Interest areas include:
- Creating human molecular reference maps from defined cell types and circuits.
- Elucidating the relationship between genomic features, such as gene regulatory elements and chromatin structure, and the spatiotemporal dynamics of gene and protein expression in healthy individuals and those with mental illnesses.
- Assembling reference, multi-omic molecular maps (e.g., epigenomic, transcriptomic, proteomic) across development, regions, and cell types of the human brain.
- Mapping quantitative trait loci (e.g., expression, methylation, histone acetylation, chromatin accessibility) across development, regions, and cell types of the human brain.
- Identifying the developmental periods, signaling pathways, cell types, and neural systems driving disease pathogenesis in humans.
Interest areas include:
- Increasing the power and reliability of association studies including whole genome, exome-, epigenome-, phenome-, and other “ome”-wide studies.
- Integrating multi-omic datasets from tissues and single cells.
- Integrating phenotype data spanning multiple units (e.g., genetic variation, gene expression, electrophysiology, neuroimaging, behavior).
- Focusing on robust genome-wide and brain-wide association studies, genome-wide x phenome-wide interaction studies, and genome-wide epistasis detection.
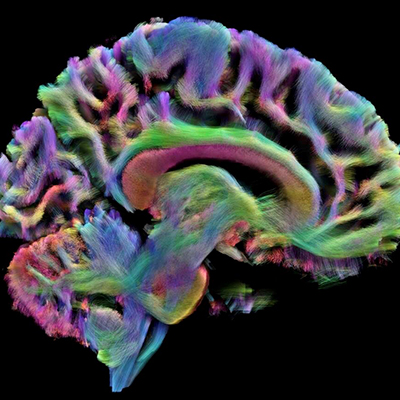
Most of what we currently know about human brain circuits comes from studying healthy functioning. To understand changes in neural structure and function related to mental illnesses, we must apply the research tools we have in hand to characterize the neural circuits implicated in mental illnesses across diverse populations. It is becoming increasingly possible to map both proximal and distal neural connectivity in the brain, enabling an understanding of the relationships between neuronal structure and function at the systems level. To develop comprehensive understanding of neural connectivity in mental illnesses, we must extend existing structural and functional mapping to the cellular level. Connectomic studies of the brain are bringing us innovative tools and technologies. Emerging developments include robust molecular markers for synapses, new tracers for identifying circuit inputs and outputs, high density electrode arrays, and novel microscopy techniques to reconstruct brain circuits. New technologies are faster, less expensive, and scalable for anatomic reconstruction of neural circuits at all biological scales. Focused studies of circuit disruption in mental illnesses will be essential to translate knowledge gained from these technologies into novel targets for therapeutics.
To better characterize and analyze the neural circuit mechanisms involved in mental illnesses, NIMH will support research that employs the following Strategies:
Interest areas include:
- Conducting brain-wide analyses to determine which neural circuits drive network patterns associated with a pathology.
- Characterizing network components at the molecular, single-cell, morphological, microenvironmental, or circuit level that contribute to risk for mental illnesses.
- Conducting connectomic studies during brain development, from prenatal to late adulthood.
Interest areas include:
- Investigating how molecular, cellular, and/or circuit-level changes in the brain, or changes in response to environmental factors, affect the coordination of neural activity patterns (very large-scale samples) during cognitive function, emotional regulation, and social cognition at one or more stage of development, from prenatal to late adulthood.
Interest areas include:
- Validating translatable biomarkers using analysis of neural circuits; combining approaches, such as those that assess or detect synaptic integrity, plasticity, and function; as well as immune signaling activity and cells that affect neural circuits.
- Integrating molecular and genomic data from large-scale multiomic studies with connectomics and functional approaches in humans to formulate multilevel hypotheses regarding circuit function and dysfunction in mental illness.
- Testing the causal nature of circuit-based hypotheses in animal, computational, and human experimental systems.
Interest areas include:
- Creating or improving methods to investigate the connectivity of brain networks, at total or very large scale, and during one or more stages of development that are relevant to mental illnesses, including age-appropriate, novel imaging tools for visualization and analyses of brain structure and function.
- Pioneering strategies to use circuit-based technologies to identify circuit-specific intervention targets.
- Developing novel technologies to modulate specific circuit elements with the potential for translation into humans.
Progress for Goal 1
Advancing basic science of brain, genomics, and behavior to understand mental illnesses.
Updated: