From Breakthroughs to Best Practices: How NIMH Transforms Research Into Real-World Care
Patricia Arean, Susan Azrin, Michael Freed, Adam Haim, Jennifer Humensky, Stephen O’Connor, Jane Pearson, Mary Rooney, Matthew Rudorfer, Joel Sherrill, and Belinda Sims, on behalf of the Division of Services and Intervention Research.
• 75th Anniversary
For 75 years, NIMH has transformed the understanding and treatment of mental illnesses through basic and clinical research—bringing hope to millions of people. This Director’s Message, guest written by NIMH’s Division of Services and Intervention Research, is part of an anniversary series celebrating this momentous milestone.
More than one in five adults in the United States live with a mental illness, and this number is expected to rise in the coming decades. Since its establishment, the National Institute of Mental Health (NIMH) has known that people need more than exciting scientific discoveries—they need access to effective treatments and the best quality of care available. After all, finding new treatments and cures means little to the millions of people impacted by mental illnesses if there is no way to translate these breakthroughs into policy and practice.
In the Division of Services and Intervention Research (DSIR), we provide the critical link between basic and clinical science and explore the best practices to implement those evidence-based treatments. We’re dedicated to growing and investing in this field of science, and although much work is still to be done, we’ve had some notable successes impacting real-world public health practices and policies.
Improving outcomes for people with early psychosis
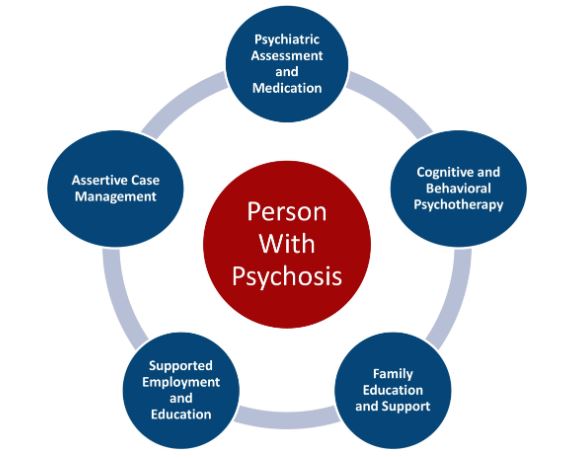
One example of research that has bridged the divide between science and policy is the Recovery After an Initial Schizophrenia Episode, or RAISE, studies. Research has shown that young people with schizophrenia and related psychotic disorders have much better outcomes when they receive effective treatment within months of their first symptoms. The RAISE studies, which NIMH supported, focused on methods to detect and treat early psychosis in a timelier fashion. These studies found that a type of care called coordinated specialty care (CSC)—a recovery-oriented, team-based approach to treating early psychosis—was more effective than the typical care used at the time.
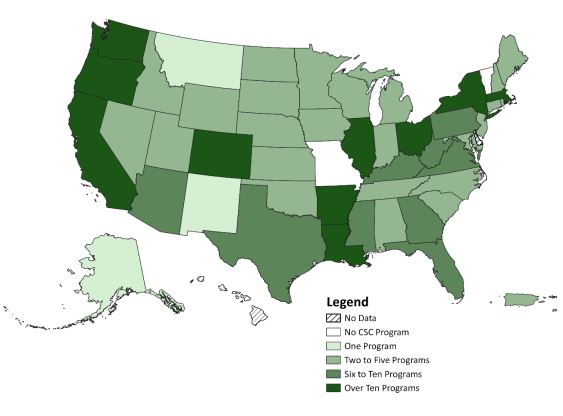
NIMH engaged extensively with members of the early schizophrenia care community to ensure RAISE findings would be relevant and actionable for rapid translation into practice. These efforts created the momentum for the broad expansion of CSC treatment programs nationwide. In 2023, the creation of associated billing codes further supported this model of mental health care, allowing for increased adoption by care providers.
From CSC programs in two states in 2008, the United States now has more than 360 such programs, allowing more people to receive this evidence-based care.
Removing barriers to schizophrenia treatment
Clozapine, the only drug approved for treatment-resistant schizophrenia, is underutilized in the United States, particularly among African American communities. Many reasons have been linked to this disparity, including provider bias, lack of trust in the mental health care system for African American clients, and an overprescribing of first-generation antipsychotic medication for African Americans with schizophrenia. Additionally, clozapine has been associated with an increased risk of the onset or exacerbation of neutropenia, a condition that affects white blood cells and impairs the body’s ability to fight infection. Benign ethnic neutropenia is a chronic form of neutropenia that's present from birth and commonly seen in people of African descent.
In 2015, NIMH supported a large, multinational study that investigated the use of clozapine in individuals of African descent who have benign neutropenia . Individuals with treatment-resistant schizophrenia who had benign neutropenia had previously been declared ineligible to receive clozapine treatment due to the Food and Drug Administration’s prescribing guidelines related to this medication. The finding of this NIMH-supported study opened up clozapine treatment to a whole new group of individuals with schizophrenia, allowing them to benefit from this important medication.

Building upon these findings, NIMH is currently funding research that evaluates the effectiveness of an educational program for clinicians about clozapine . Hundreds of prescribers and clinicians throughout the state of Maryland are participating in an innovative educational tele-mentoring program that connects them with centralized experts. The prescribing activity of clinicians participating in the educational program will be compared with those who have not participated to see if the program is effective at increasing the use of clozapine among those who would benefit from it.
Given the real-world context of this study, the findings can potentially inform clinical practice and make a needed treatment more accessible to many African Americans.
Preventing mental illnesses in youth
Recognizing that many mental health conditions have their origins early in life, NIMH has supported several seminal studies showing the effectiveness of interventions designed to prevent conduct disorder and other behavioral conditions in youth. These include evaluations of a classroom-wide behavioral intervention called the Good Behavior Game , a school-home wraparound intervention called Fast Track , and a brief family-based intervention for toddlers called Family Check-up .
Today, NIMH continues to support the analysis of data from participants in these studies who have been followed into adulthood . Initial results from these longitudinal analyses show sustained effects of the interventions on conduct disorder and unanticipated positive impacts on other mental health outcomes, such as reductions in adolescent and adult depression, anxiety, and suicide risk, thus demonstrating the broad and enduring effects of early prevention efforts.
Early intervention represents an important pathway to making quality care accessible to everyone, particularly when embedded within a broader approach that addresses social determinants of health. NIMH is currently supporting research that tests strategies to improve access to prevention services, including primary care-based depression prevention for adolescents and mental illness prevention for at-risk Latinx youth .
Suicide prevention in emergency departments
An estimated 20% of people who die by suicide visit the emergency department in the 60 days before their death, making these settings an important target for suicide prevention efforts. Given the importance of emergency departments as a place to identify and provide support for people at risk for suicide, NIMH has supported research establishing the effectiveness of suicide prevention services in these settings.
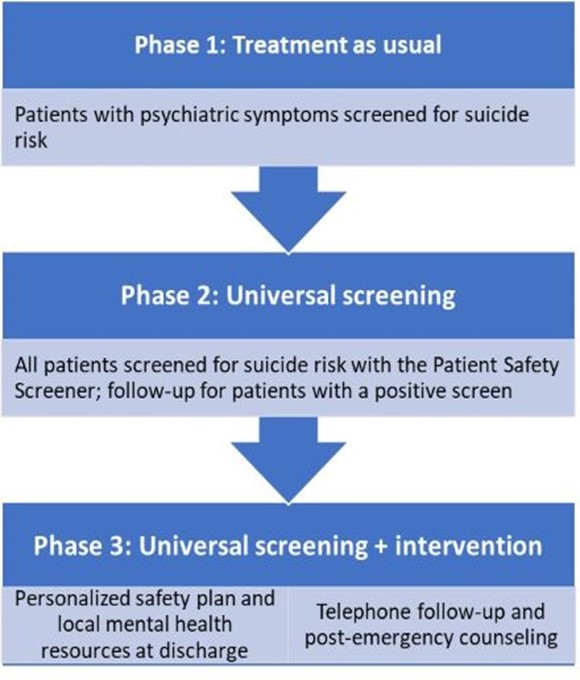
An example of this research is the multisite Emergency Department Safety Assessment and Follow-up Evaluation (ED-SAFE) study. ED-SAFE demonstrated that providing universal screening for suicide risk and a brief safety planning intervention in emergency departments, combined with limited follow-up contacts once people had been discharged, decreased subsequent suicide attempts by 30% compared to usual care.
A follow-up study also supported by NIMH, called ED-SAFE 2 , tested the integration of universal screening for suicide risk and safety planning into the clinical workflow of eight emergency departments. Study results indicated that integration of this clinical workflow resulted in sustained reductions in suicide deaths and subsequent acute health care visits.
These landmark studies convey the power of providing relatively brief, well-timed interventions during emergency encounters to reduce the risk of later suicide. NIMH continues to fund research to expand the reach of emergency department-based interventions, including the use of digital health technologies and strategies to overcome workforce shortages and other barriers to implementing suicide screening and intervention (for instance, digital technology to increase the reach of ED-SAFE ; a multi-component, tailored strategy for suicide risk reduction ). NIMH works closely with public and private partners to take recent data, like those collected during the ED-SAFE studies, and help translate them into real-world practice .
Moving forward
The studies and projects shared here are only a few examples of exciting areas of investment that have resulted in real-world changes in care. Although we’ve made progress, we recognize the need to continue supporting research with near-term potential and cultivating a vibrant workforce to lead the next generation of services and intervention research.
Further, NIMH is committed to working with researchers, communities, payors, advocacy groups, state policymakers, federal agencies, and others to help support intervention and services science that will significantly impact mental health policy and care practices—ultimately helping people access better mental health care.

